War is associated with death, disability and invisible psychological injuries,Reference Murthy and Lakshminarayana1 many of which affect children and adolescents.Reference Barbara2 Post-traumatic stress disorder (PTSD) among children affected by war is well documented,Reference Slone and Mann3,Reference Slone, Lavi, Ozer and Pollak4 and although this may be linked to conflict and war settings,Reference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Wa5 other factors can contribute to adverse mental health experiences, including poverty and deprivation.Reference Macksoud6 A total of 85% of the world's population live in one of the 153 countries currently classified as a low- and middle-income country (LMIC).7 This majority accounts for 80% of all people globally with mental health challenges;Reference Yatham, Sivathasan, Yoon, da Silva and Ravindran8,Reference Weinmann and Koesters9 however, data on mental health prevalence and outcomes in these settings are lacking. Many children and adolescents affected by war live in low-resource countries, where mental health services are unavailable or inaccessible.10 Our review, therefore, focuses on psychological support for children and adolescents with PTSD in LMICs in the Middle East.
Many Middle Eastern countries, regardless of income class, have an insufficient number of psychiatrists to cope with demand, and lack specialised child and adolescent psychiatry (CAP) services.Reference Clausen, Bazaid, Azeem, Abdelrahim, Elgawad and Alamiri11 In a study by Clausen et al of 15 Middle Eastern countries (including Palestine and Jordan), the authors identified an almost complete absence of CAP services, resulting in a lack of established national training guidelines. Consequently, many young people are at risk of developing long-term mental health conditions that will go unidentified and untreated from an early age.Reference Clausen, Bazaid, Azeem, Abdelrahim, Elgawad and Alamiri11 The lack of CAP services is a global issue; however, research has shown that the demand is greater in low-resource countries not only because they lack essential resources, but also because 90% of children and adolescents live in LMICs whereas 95% of psychiatrists are in high-income countries.Reference Clausen, Bazaid, Azeem, Abdelrahim, Elgawad and Alamiri11 This makes the low-resource requirements and scalability of some psychosocial interventions particularly suited to LMICs in the Middle East (Iran, Iraq, Jordan, Lebanon, Palestine, Syria, Yemen and Turkey7,12 ).
Non-governmental organisations play an important role in providing mental health services for children in LMIC in the Middle East10 and assessing psychosocial concerns.Reference Wells, Steel, Abo-hilal, Hassan and Lawsin13 Non-governmental organisations and academic divisions that specialise in child mental health have highlighted the need for mental health programmes and the scaling up of mental health services.Reference Chisholm, Flisher, Lund, Patel and Saxena14 The World Health Organization responded to this lack of services by developing the Mental Health Gap Action Programme, where psychological and psychosocial interventions are considered first-line therapy, including cognitive–behavioural therapy (CBT) and narrative exposure therapy.Reference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Wa5
War has affected several Middle Eastern countries such as Palestine, Iraq and Lebanon for decades, whereas countries such as Syria have experienced intensive war more recently. A wave of protests and overthrowing of dictatorships across the region in 2010, known as the Arab Spring, led to intense violence in countries like Syria, with many people becoming internally displaced and/or refugees.Reference Amawi, Mollica, Lavelle, Osman and Nasir15 Publications from the Middle East are scarce, particularly in CAP services;Reference Clausen, Bazaid, Azeem, Abdelrahim, Elgawad and Alamiri11 however, some evidence suggests a high prevalence of PTSD in countries such as Palestine and Iraq, compared with high-income, non-Middle Eastern countries.Reference Attanayake, McKay, Joffres, Singh, Burkle and Mills16 Dimitry's systematic review of 21 studies involving 11 000 children and adolescents in Palestine found PTSD prevalence to range from 23 to 70%.Reference Dimitry17 The percentage of Lebanese children and adolescents exposed to different traumatic experiences in Dimitry's review was also high (up to 94%).Reference Dimitry17 In another study, 43% of Lebanese children met PTSD criteria for war-related trauma that was experienced up to 10 years previously, highlighting a complex and potentially delayed response in processing trauma.Reference Macksoud and Aber18 One study of Iraqi children found that 14% had a diagnosis of PTSD,Reference Razokhi, Taha, Taib, Sadik and Al Gasseer19 whereas 35–45% of Syrian children in Syria and Turkey are estimated to be experiencing PTSD symptoms.Reference Perkins, Ajeeb, Fadel and Saleh20,Reference Sirin and Rogers-Sirin21 Given this high prevalence of PTSD and trauma, ongoing conflict in these war-affected regions and lack of services in the Middle East, the provision of effective interventions for this vulnerable population and evidence to guide future research are warranted and urgently needed.
Rationale for the review
Before undertaking this review, we identified five other reviewsReference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Wa5,Reference Yatham, Sivathasan, Yoon, da Silva and Ravindran8,Reference Sirin and Rogers-Sirin22–Reference Purgato, Gross, Betancourt, Bolton, Bonetto and Gastaldon24 that examined psychological/psychosocial interventions in LMICs; two reviews found suggestive evidence of efficacy of interventions targeting children;Reference Morina, Malek, Nickerson and Bryant22,Reference Barbui, Purgato, Abdulmalik, Acarturk, Eaton and Gastaldon23 two other studies identified beneficial effects for trauma-focused interventions only or so-called first-line strategies, such as CBT;Reference Yatham, Sivathasan, Yoon, da Silva and Ravindran8,Reference Purgato, Gross, Betancourt, Bolton, Bonetto and Gastaldon24 and one review found very low-quality evidence for children's psychological/psychosocial interventions.Reference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Wa5 However, some of these reviews included studies with adults and children in the same sample, with more focus on results from adults in the sample,Reference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Wa5,Reference Barbui, Purgato, Abdulmalik, Acarturk, Eaton and Gastaldon23 or they included studies with different designs other than randomised controlled trials (RCTs)Reference Yatham, Sivathasan, Yoon, da Silva and Ravindran8 or that were conducted in various humanitarian crisis settings such as natural disasters, mass violence and armed conflicts,Reference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Wa5,Reference Morina, Malek, Nickerson and Bryant22 rather than war and conflict specifically. There are no known recent reviews to our knowledge that focus on the unique context specific to LMICs in the Middle East, to summarise evidence on psychosocial intervention for war-affected children in this area.
Although recent reviews have evaluated PTSD interventions in LMICs more broadly,Reference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Wa5,Reference Yatham, Sivathasan, Yoon, da Silva and Ravindran8,Reference Sirin and Rogers-Sirin22–Reference Purgato, Gross, Betancourt, Bolton, Bonetto and Gastaldon24 these have not focused solely on the Middle East, where armed conflicts and wars are currently ongoing. War-related stressors and trauma are expected to lead to heightened prevalence of mental health problems, particularly PTSD.Reference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Wa5 There is good initial evidence that early interventions for children and adolescents can prevent long-term psychological problems such as PTSD;Reference Macksoud6 however, results require further investigation, using robust methods. A previous systematic review mentioned the lack of RCTs in LMICs;Reference Morina, Malek, Nickerson and Bryant22 consequently, further research in this field could provide much needed guidance for future work and recommendations.
The aim of this systematic review is therefore to evaluate the effectiveness of available RCT-assessed interventions for children and adolescents who have been exposed to war and conflict in LMICs in the Middle East. Many children and adolescents previously living in LMICs in the Middle East have been displaced, with large populations moving into Middle Eastern countries not currently experiencing war, such as Jordan, Lebanon and Turkey.Reference Drescher, Kiselev, Akhtar, Acarturk, Bryant and Ilkkursun25 We therefore expanded our review focus to include children and adolescents who have been displaced to these regions. Four research questions are addressed: What are the available RCT-assessed interventions for children and adolescents? Are these interventions effective in reducing PTSD symptoms as a main outcome, and other psychological outcomes if measured, compared with control groups? Do children and adolescents benefit in different ways from the intervention based on demographic characteristics and war exposure? Finally, are there additionally reported benefits or consequences associated with these interventions (such as reduced distress, relief or new skill development)?
Method
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines were followedReference Moher, Liberati, Tetzlaff and Altman26 and the systematic review protocol was registered on the PROSPERO database (reference: CRD42019140370). Meta-analysis was considered but, because of the small number of studies and varied treatment implementation and assessment, qualitative narrative synthesis was used to summarise findings.
Inclusion criteria
Studies were included if they were published in English in a peer-reviewed journal; were RCTs of psychological or psychosocial interventions; and were undertaken with children and adolescents aged ≤18 years, who are refugees or internally displaced, or have been exposed to wars and conflicts, and live in LMICs in the Middle East. All study participants indicated PTSD symptom scores above the clinical cut-off.
It is important to mention that although in the PROSPERO record we indicated the target age group to be <18 years, because of the lack of RCTs in this range, we included one study with participants aged ≤18 years. The average age of the studyReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 sample (range 12–18 years, average 14.25 years) was comparable with other included studies.
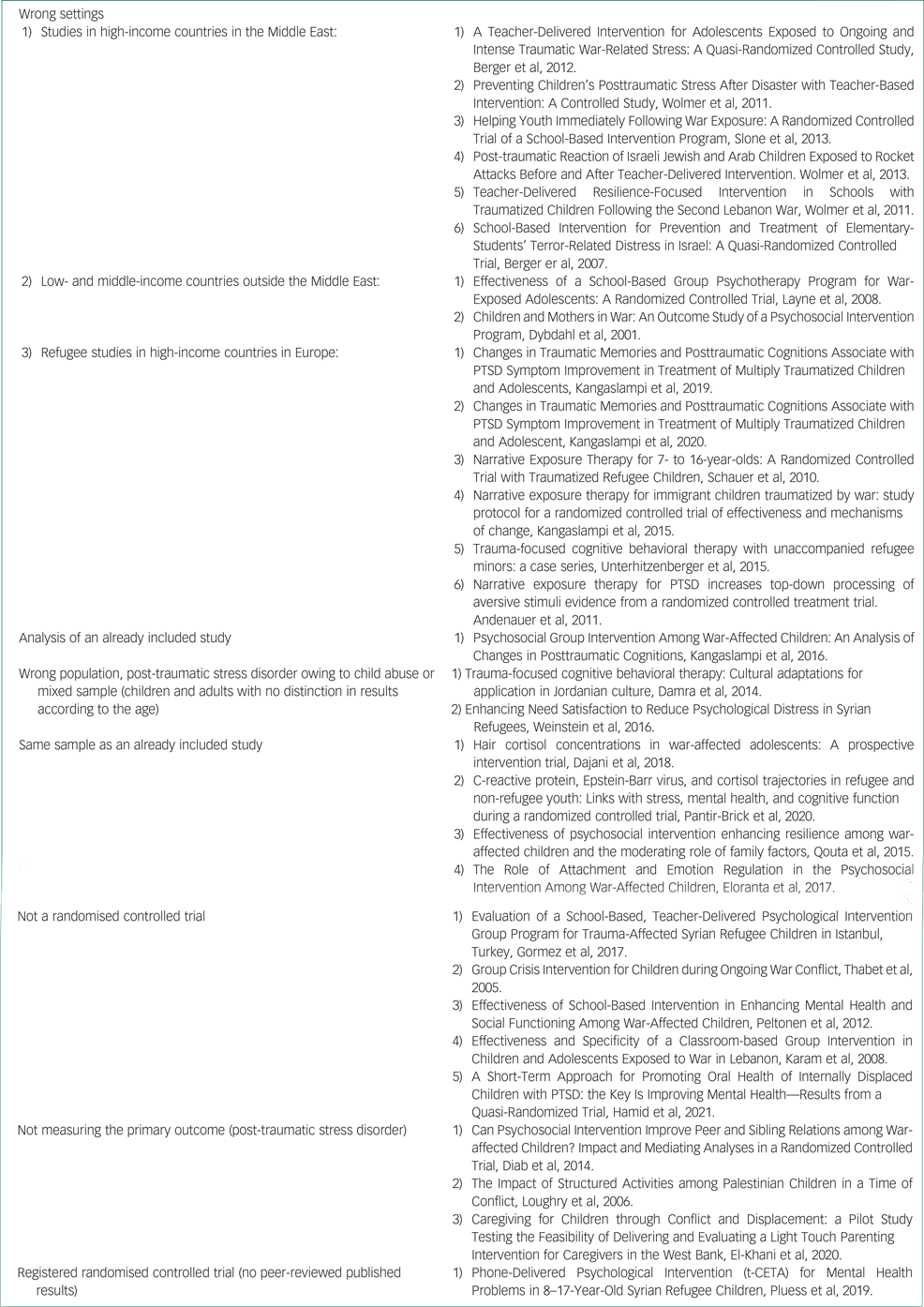
Exclusion criteria
Studies were excluded if they were undertaken with children and adolescents who were refugees or internally displaced living in high-income countries (whether inside or outside the Middle East), conducted in LMICs outside the Middle East, did not measure PTSD as a primary or secondary outcome, or included a mixed age sample (i.e. adults and children) without results presented separately by age. In addition, studies were excluded when war or conflict was not identified as one of the causes of PTSD.
Search strategy and selection process
The following databases were searched from their inception until December 2021: PubMed, Cochrane Library and Ovid (Medline, PsycINFO, Global Health and EMBASE). The following keywords were used: Effect*, treatment, intervention, ‘psychological interventions’, PTSD, trauma, ‘post trauma’, ‘posttraumatic stress disorder’, child, ‘school age’, adolescent, youth, ‘middle east’, ‘Arab countries’, ‘middle income’, ‘low income’, LMIC, war, conflicts, ‘armed conflicts’, refugee, ‘internally displaced’. Search results were filtered to include only RCT studies. Reference lists of previous systematic reviewsReference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Wa5,Reference Yatham, Sivathasan, Yoon, da Silva and Ravindran8,Reference Morina, Malek, Nickerson and Bryant22,Reference Zhang, Zhou, Yang, Hetrick, Weisz and Cuijpers28,Reference Jordans, Tol, Komproe and De Jong29 were manually checked and suitable studies included. Titles and abstracts were reviewed independently against the inclusion/exclusion criteria by two authors (A.F.A., A.R.M.) and duplicates were removed. Full texts of the remaining articles were then assessed for inclusion by two authors.
Data extraction
Author A.F.A. extracted the following data from all studies: country/location of the intervention, participant characteristics, type of intervention and control conditions, outcome measures, PTSD diagnosis or symptoms score at baseline/follow-up, number and duration of follow-up, subgroup analysis, war stressors, treatment fidelity, therapist training and any other important notes. The data used was that for participants who had completed follow-up.
Quality assessment
We used the Cochrane Collaboration Risk of Bias Tool (CCRBT)Reference Higgins, Altman, Gøtzsche, Jüni, Moher and Oxman30 to assess four main types of bias: selection bias, attrition bias, detection bias and reporting bias. Given the nature of psychological interventions, where participant blinding to treatment condition was not possible, the ‘blinding’ component of the CCRBT was not used. Additional risk of biases was assessed from miscellaneous sources. Assessments were conducted independently by two authors (A.F.A. and A.R.M.), using the grading system (high, low or unclear risk), with any disagreements resolved through discussion.
Results
The systematic search yielded 1008 potentially relevant articles. Inspection of titles and abstracts reduced this to 64 articles, of which 28 were duplications. After full-text examination of the remaining 36 articles, six met inclusion/exclusion criteria, and data were then extracted (Fig. 1, Table 1).

Fig. 1 Flow diagram. PTSD, post-traumatic stress disorder; RCT, randomised controlled trial.
Table 1 Characteristics of included studies
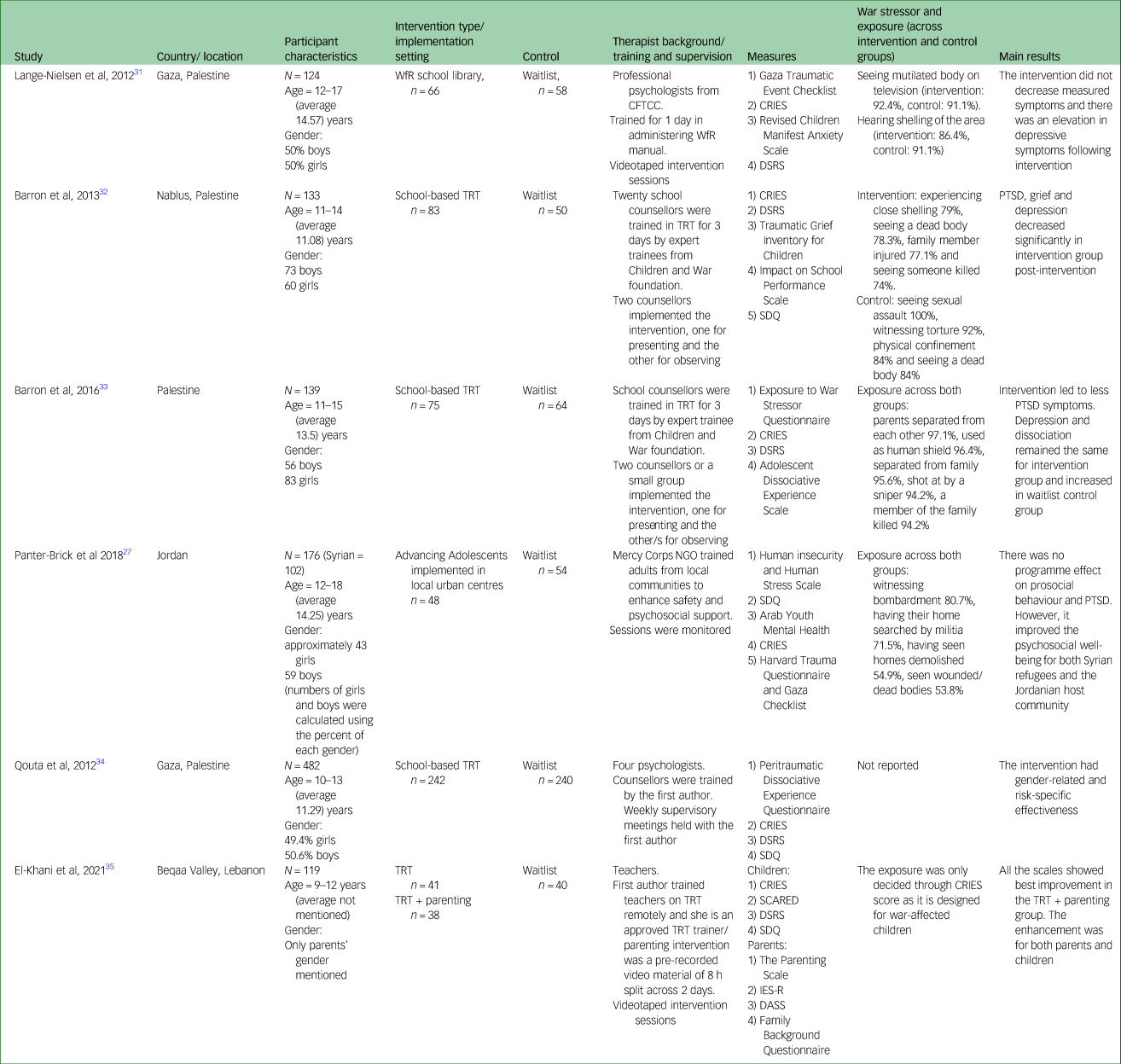
WfR, Writing for Recovery; CFTCC, Child and Family Training and Counseling Center; CRIES, Child Revised Impact of Events Scale; DSRS, Depression Self-Rating Scale for Children; TRT, Teaching Recovery Techniques; SDQ, Strengths and Difficulties Questionnaire; PTSD, post-traumatic stress disorder; NGO, non-governmental organization; SCARED, Screen for Childhood Anxiety-Related Disorders; IES-R, Impact of Events Scale Revised; DASS, Depression–Anxiety–Stress Scale.
Study samples and settings
Four of the included studies took place in Palestine with Palestinian children and adolescents in three different locations (Gaza, Nablus and West Bank),Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31–Reference Qouta, Palosaari, Diab and Punam34 one took place in JordanReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 and involved Syrian refugees and Jordanian adolescents, and one took place in LebanonReference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 and included Syrian refugees. Included participants in all studies were children and adolescents aged between 9 and 18 years, with average ages around 11 years in two of the studies in Palestine,Reference Barron, Abdallah and Smith32,Reference Qouta, Palosaari, Diab and Punam34 13 years in the third study in Palestine,Reference Barron, Abdallah and Heltne33 and 14 years in the fourth study in Palestine and the study in Jordan.Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27,Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 Gender distribution was almost equal in two studies,Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31,Reference Qouta, Palosaari, Diab and Punam34 boys predominated (57.8% and 54.9%) in two studiesReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27,Reference Barron, Abdallah and Smith32 and girls predominated (59.7%) in one study.Reference Barron, Abdallah and Heltne33 The study by El-Khani et alReference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 did not report age and gender. This does not include all LMICs in the Middle East (Iran, Iraq, Jordan, Lebanon, Palestine, Syria, Yemen and Turkey7,12 ), and therefore results cannot be generalised to all Middle Eastern locations.
Gaza, Nablus and villages in the West Bank have been highly affected with ongoing military operations and violence. Two studies that took place in Gaza included schools in areas shelled during the Gaza war in 2008/2009Reference Qouta, Palosaari, Diab and Punam34 and from a refugee camp in Gaza.Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 Nablus and some villages near East Jerusalem in West Bank were selected in the studies by Barron et alReference Barron, Abdallah and Smith32,Reference Barron, Abdallah and Heltne33 because of high levels of ongoing military violence. Refugees displaced from Syria for an average of 2.7 years were included in the Jordan studyReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 as they experienced war and traumatic events related to war, such as witnessing bombardment before moving to Jordan. Syrian child refugees who were displaced to Lebanon and scored 17 or more on the Child Revised Impact of Events Scale (CRIES-13) were included in the Lebanon study.Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35
The combined sample size was 1099 participants, with sample sizes in contributing studies ranging from 102Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 to 482.Reference Qouta, Palosaari, Diab and Punam34 In the study by Panter-Brick et al,Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 only Syrian children (56.3% and 60% in intervention and control groups, respectively) were included because Jordanian children were not exposed to war and their PTSD symptoms resulted from other causes, such as domestic abuse. The number of Syrian children (n = 102 (43 females); 48 in the intervention and 54 in the control conditions) was calculated from data provided in the paper. It was not possible to extract some data of interest separately for Syrian children as they were reported with Jordanian children as one group.
War and trauma exposure
There were no significant differences between intervention and control groups on war and trauma exposure in any of the four studies that included these data (Table 1). One study with a ‘Teaching Recovery Techniques’ (TRT) intervention reported experienced traumatic events ranging from nine to 26 events per participant.Reference Barron, Abdallah and Heltne33 Sixteen children in this study experienced 24 events each. The second TRT study reported that girls in the control group had higher levels of exposure compared with boys.Reference Barron, Abdallah and Smith32 All participants included in the Syrian sample at the baseline of the Panter-Brick et al studyReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 reported an average of 6.36 traumatic events, and 82.5% of Syrian refugees reported four or more lifetime trauma exposures.
The nature and types of traumatic events and stressors reported (Table 1) were war related. War events such as house or area shelling was reported in one TRT studyReference Barron, Abdallah and Heltne33 (79% of intervention group reported this event), the ‘Writing for Recovery’ (WfR) studyReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 (86.4% in the intervention group and 91.1% in the control group) and the ‘Advancing Adolescents’ studyReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 (54.9%). Seeing a dead or injured body, whether a family member or a stranger, was also reported in two of the TRT studies (74–78%Reference Barron, Abdallah and Smith32 and 94%Reference Barron, Abdallah and Heltne33), the WfR study (91–92%)Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 and the Advancing Adolescents study (53.8%).Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 All control group participants in one TRT study reported seeing someone sexually assaulted (100%).Reference Barron, Abdallah and Smith32
Intervention and control types
All studies implemented school-based interventions except for the study by Panter-Brick et al,Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 where the intervention took place at different community centres in Jordan. All interventions were implemented in groups rather one-to-one sessions. Three types of interventions were used: one CBT-oriented, one derived from narrative therapy (all trauma-informed) and one community-based psychosocial care intervention. These three are detailed below.
Teaching Recovery Techniques
TRTReference Barron, Abdallah and Smith32–Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 was developed by the Children and War Foundation to be used with children and adolescents in wars and disaster contexts.Reference Barron, Abdallah and Heltne33 It is a skills-based programme, and derived from trauma-focused CBT,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 delivered by teachers or school counsellors, consisting of five sessions lasting for 90 min each. Sessions aim to help students understand trauma, cope with loss, and learn strategies to manage PTSD symptoms such as intrusive memories, hyperarousal and avoidance. School counsellors who delivered the programme first attended a 3-day training programme delivered by two specialists from the Children and War Foundation.
The study by El-Khani et alReference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 added three additional sessions with a parenting component (TRT + P) to one of the intervention groups. They identified parenting skills through systematic and analytical approaches, and they identified parental needs from examples mentioned when interviewing parents in conflicts areas. The new component aimed to understand behavioural change and to enhance positive child–parent interaction through simple techniques like rewarding desirable behaviour by using available material in low-resource sittings, such as behavioural charts.Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 It is important to mention that this studyReference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 was implemented during the COVID-19 pandemic, and that the intervention was implemented online.
Writing for Recovery
WfRReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 is a manualised intervention based on narrative therapy techniques, also developed by the Children and War Foundation. The programme is for children and adolescents with a history of trauma, aged 12–18 years.Reference Yule, Dyregrov, Neuner, Pennebaker, Raundalen and Emmerik36 It includes six writing sessions over three consecutive days: two sessions per day (15 min each), with a break of 10 min in-between. The writing tasks progress from general expression of emotions and detailing traumatic memory to developing insightful perspectives, with the intention to develop new narration for the traumatic event by facilitating and reframing insight. The intervention does not require specialist mental health training and was delivered by teachers after completing a 1-day training programme.
Advancing Adolescents
Advancing AdolescentsReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 is an 8-week programme of 16 sessions (two sessions per week), originally undertaken by Mercy Corps (an international non-governmental organisation). The programme is informed by the profound stress attunement framework, which focuses on psychosocial care for vulnerable children and adolescents and improving social interactions via a community-based, non-clinical setting. It consists of three main elements: safety, support and structured group activities for youths living in humanitarian crisis settings. Participants choose their preferred activity, such as playing sports, art and crafts, and vocational or technical skills activities. The programme was delivered by adult volunteers from the community who were trained by Mercy Corps.
All included studies compared a psychological or psychosocial intervention to a control group, except for the study by El-Khani et al,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 which compared an intervention group (TRT + P) with a comparison group (TRT only) and control group. Most studies used waitlist control.Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27,Reference Barron, Abdallah and Smith32–Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 Authors of one studyReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 reported a deviation in the study protocol, as the control group received the WfR intervention after finishing only one of the two planned assessments. The reason this occurred was because of a ‘communication difficulty’.
Measures of PTSD
The CRIESReference Perrin, Meiser-Stedman and Smith37 was used to assess PTSD symptoms in the six included studies (see Table 1).Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27,Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31–Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 The CRIES is a self-report questionnaire for 8- to 18-year-olds, developed by the Children and War Foundation to assess risk of developing PTSD. The measure has eight-item (four for intrusion and four for avoidance) and 13-item (with an additional five items for arousal symptoms) versions.Reference Smith, Perrin, Dyregrov and Yule38 It has good face and construct validity, a stable factor structure and has been adapted to different languages and locations.Reference Perrin, Meiser-Stedman and Smith37
Additional tools were used in two studies. Authors of the first study, evaluating Advancing Adolescents,Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 used the Harvard Trauma Questionnaire,Reference Berthold, Mollica, Silove, Tay, Lavelle and Lindert39 and authors of the second study, evaluating WfR, used the Gaza Traumatic Event Checklist,Reference Thabet40 developed to assess trauma level (specifically for Palestinian children in Gaza), in addition to the CRIES measure.
Other psychological outcomes measures
Depression was assessed in five studiesReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31–Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 with the Depression Self-Rating Scale for Children (DSRS).Reference Birleson41 Peritraumatic dissociation was assessed in two studiesReference Barron, Abdallah and Heltne33,Reference Qouta, Palosaari, Diab and Punam34 with the Peritraumatic Dissociative Experience Scale.Reference Marmar, Metzler, Otte, Wilson and Keane42 Anxiety was assessed in two studiesReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 with the Revised Children Manifest Anxiety ScaleReference Reynolds and Richmond43 and the Screen for Childhood Anxiety-Related Disorders.Reference Birmaher, Khetarpal, Brent, Cully, Balach and Kaufman44
The Strengths and Difficulties Questionnaire (SDQ)Reference Goodman45 was used in four studiesReference Barron, Abdallah and Smith32–Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 to assess psychological distress. The SDQ is a screening tool to measure behaviours and emotion in children. It can be completed independently by children and adolescents, if aged ≥11 years, or their teachers or parents. It contains 25 items (five scales with five items each): emotional symptoms subscale, conduct problems subscale, hyperactivity/inattention subscale, peer relationships problems subscale and prosocial behaviour subscale. Panter-Brick et al used the SDQ, in addition to the Human Insecurity and Human Distress Scale.Reference Ziadni, Hammoudeh, Abu Rmeileh, Hogan, Shannon and Giacaman46,47
War exposure measures
Although four studies included questions about war stressors and exposure, formal war exposure measures were used only in one study. Barron et alReference Barron, Abdallah and Heltne33 used the Exposure to War Stressor Questionnaire,Reference Smith, Perrin, Yule, Hacam and Stuvland48 which is a 26-item measure of ‘yes’ or ‘no’ questions and has no clinical cut-off.
Translation
Measures used in all included studies were in Arabic. All measures were already available in Arabic and validated in previous studies.
Follow-up
Follow-up frequency ranged from one to three sessions after baseline assessment across the studies (see Table 2). Follow-up duration typically ranged from 2 weeks to 2 months post-intervention for the first follow-up. For the studies in which two follow-ups were completed, the second follow-up took place 12 weeks to 4/5 months post-intervention.
Table 2 Post-traumatic stress disorder symptoms by study and intervention/measure, with follow-up intervals
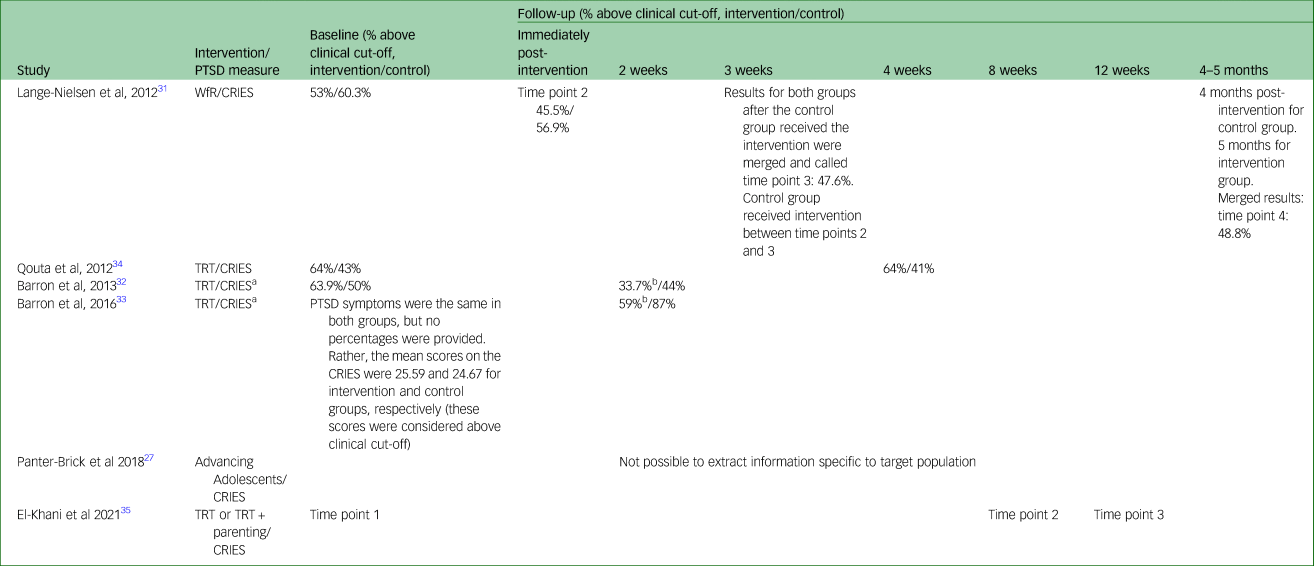
PTSD, post-traumatic stress disorder; WfR, Writing for Recovery; CRIES, Child Revised Impact of Events Scale; TRT, Teaching Recovery Techniques.
a. CRIES: questionnaire was used one month before programme delivery. All other measures: 2 weeks before programme delivery.
b. Significant reduction in intervention condition.
Outcomes
PTSD-related outcomes
Authors of three studies found that the TRT intervention was effective in decreasing PTSD symptom scores.Reference Barron, Abdallah and Smith32,Reference Barron, Abdallah and Heltne33,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 Authors of the fourth TRT studyReference Qouta, Palosaari, Diab and Punam34 found a gender-related and risk-specific effectiveness; girls with lower severity of peritraumatic dissociation at time point 2 and boys at time point 2 had reduced PTSD symptoms.Reference Qouta, Palosaari, Diab and Punam34 However, a correction to results for this study indicated that these differences were not statistically significant.Reference Qouta, Palosaari, Diab and Punamäki49 No treatment effect was found in studies implementing the Advancing Adolescents intervention or WfR programme.
Teaching Recovery Techniques
In one study by Barron et al,Reference Barron, Abdallah and Smith32 pre-intervention post-traumatic stress levels were significantly higher in the intervention group. Fifty-three students (63.9%) in the intervention group exceeded the diagnosis cut-off based on CRIES-8 scores, whereas 25 students (50%) had similar scores in the control group. After the intervention, 28 (33.7%) students in the intervention group and 22 (44%) students in the control group exceeded diagnosis cut-off.
In another study by Barron et al,Reference Barron, Abdallah and Heltne33 pre-intervention post-traumatic stress levels were equal in the intervention and control groups. Average CRIES-8 scores were high in both groups (intervention: 25.59; control group: 24.67). A clinically significant difference was found at post-test in the intervention group, in which the mean decreased to 18.57 compared with 24.16 in control group. Twenty-nine (41%) students in the intervention group no longer met the diagnostic criteria for PTSD, compared with nine (13%) students in control group.
In the study by El-Khani et al,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 the three groups (TRT + P, TRT alone and waitlist) had the same score for avoidance and arousal symptoms at baseline; however, the TRT + P group had a higher intrusive symptoms score (TRT: P = 0.042; waitlist: P = 0.015). The TRT + P group demonstrated significant reductions in intrusive symptoms at time point 2 (P = 0.001) and time point 3 (P < 0.001), avoidance symptoms at time point 3 (P < 0.001) and arousal symptoms at time points 2 and 3 (all P < 0.001), compared with the waitlist group. The TRT group demonstrated significant reductions in intrusive and avoidance symptoms at time point 3 (P < 0.001 and P = 0.049), and arousal symptoms at time points 2 (P = 0.001) and 3 (P < 0.001), compared with the waitlist group. The TRT + P group showed significantly greater decreases in PTSD symptoms, particularly avoidance symptoms, than the TRT-only group.
In the study by Qouta et al,Reference Qouta, Palosaari, Diab and Punam34 post-traumatic stress symptoms were markedly higher in the intervention group: 64% of students in the intervention group and 43% of students in the control group had clinically significant post-traumatic stress symptoms. At follow-up, this had increased to 45% in the control group and remained unchanged in the intervention group.
Writing for Recovery
In a study by Lange-Nielsen et al,Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 baseline levels (time point 1) exceeding the cut-off for clinically significant PTSD symptoms were found in control (60.3%) and intervention (53%) groups. After intervention was delivered and symptoms assessed immediately (time point 2), there was no significant reduction in PTSD symptoms in intervention (45.5%) or control groups (56.6%). Results for both groups were merged at time point 3 after the control group received the intervention, and followed up at time point 4 (see Table 2); however, no significant change occurred between time points 3 (47.6%) and 4 (48.8%).
Advancing Adolescents
In the study by Panter-Brick et al,Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 Syrian participants had higher symptom scores than Jordanian participants for all measured outcomes (P = 0.016 compared with P < 0.001). The intervention was not effective in decreasing post-traumatic stress symptoms.
Other clinical psychological outcomes
Teaching Recovery Techniques
In the study by Barron et al,Reference Barron, Abdallah and Smith32 depression levels were the same across intervention and control groups at baseline. There was a significant reduction in depression score in the intervention group at follow-up (d = 1.24).
In the second study by Barron et al,Reference Barron, Abdallah and Heltne33 depression levels were the same in intervention and control groups at baseline; however, depression scores were slightly higher in females in the intervention group (female mean: 17.10, s.d. = 4.96) compared with females in control group (female mean: 15.17, s.d. = 4.83). No significant reduction was observed in the intervention group post-intervention (P = 0.746). However, the control group experienced an increase in depression scores (increase in mean from 14.71 to 16.2). This increase was significantly related to gender, where authors observed a statistically significant increase in female depression scores in the control group (P < 0.01). No differences were found at baseline between intervention and control groups regarding peritraumatic dissociation after completing the intervention.
In the study by El-Khani et al,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 a significant reduction in DSRS scores was identified at both time points 2 and 3 for both TRT + P groups (time points 2 and 3: P < 0.001) and TRT (time point 2: P = 0.003; time point 3: P = 0.032), whereas no such change was reported for the waitlist group. Average anxiety scores were high (above the clinical cut-off of 34) in all three groups at baseline, decreasing at time point 2, then increasing at time point 3 in the waitlist group. Although there was a slight increase between time points 2 and 3 in the TRT group, the overall decrease between time points 1 and 3 was significant (P < 0.001). The TRT + P group demonstrated the most robust improvement across the three time points (P < 0.001). Psychological distress was high in all three groups at baseline, and only decreased significantly at time point 2 in the TRT + P group, before increasing somewhat by time point 3 (no significant changes overall).
In the study by Qouta et al,Reference Qouta, Palosaari, Diab and Punam34 there was no evidence of improvement in depressive symptoms or psychological distress at time point 2 (post-intervention) or time point 3 (6-month follow-up). Authors reported a clinically significant increase in distress symptoms (see B.4 Adverse Events section).
Writing for Recovery
In the study by Lange-Nielsen et al,Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 time had an effect on depression symptoms, increasing the score overall (P = 0.000). More importantly, there was a statistically significant increase in depression scores in the intervention group, with the percentage scoring above clinical cut-off increasing from 38.5% at time point 1 to 89.4% at time point 2. However, among the merged sample at time points 3 and 4, there was a significant reduction in students scoring above the cut-off of clinical diagnosis between time point 3 (91.1%) and time point 4 (44.3%). There were no significant differences in depression scores between time point 1 (intervention: 38.5%; control: 43.1%) and time point 4 (44.3%). Clinically important anxiety levels did not differ between intervention and control groups at time point 1, neither at time points 2, 3 and 4 (time point 1: intervention 27.3%, control 22.4%; time point 2: intervention 33.3%, control 22.4%; time point 3: merged sample 30.6%; time point 4: merged sample 26%).
Advancing Adolescents
In the study by Panter-Brick et al,Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 improvements in insecurity, distress and mental health difficulties were reported. Using the Human Insecurity and Human Distress Scale, the intervention group showed sustained impact post-intervention (P < 0.01). As scores from both participant nationalities (i.e. participants from Jordan and Syria) were grouped together, it was not possible to report on our sample of interest for these outcome measures.
Demographics and war and trauma exposure outcomes
Age and gender
One study did not report any statistics on age and gender of children participants other than being aged between 9 and 12 years old.Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 Overall, there was no significant effect of moderating factors such as age and gender on main reported outcomes in other included studies, except for the increase in female depression scores in the control group (P < 0.01) in the TRT study by Barron et al.Reference Barron, Abdallah and Heltne33 However, age/gender differences for some interventions were reported at baseline/pre-tests in included studies, and are discussed below.
Teaching Recovery Techniques
One TRT study reported gender difference on the amnesia subtest, as females in intervention and waitlist groups had lower level of dissociative amnesia (P < 0.01).Reference Barron, Abdallah and Heltne33 In the same study, females in the waitlist group experienced higher levels of war stressor pre-test and post-test (P ≤ 0.01). In the second TRT study,Reference Barron, Abdallah and Smith32 significantly higher levels of traumatic grief were reported among females pre-test. In the third TRT study, significantly more males (22.5%) dropped out than females (9.2%; P < 0.001).
Advancing Adolescents
In the Advancing Adolescents study, except for prosocial behaviour and post-traumatic stress reactions, females reported higher baseline symptoms than males for all outcomes (P < 0.003 to P < 0.0001).Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27
Adverse effects
Two studies reported adverse effects at time point 2; one reported an increase in depression symptoms in the WfR interventionReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 and another reported a transient increase in the proportion of children with clinically significant psychological distress.Reference Qouta, Palosaari, Diab and Punam34
Coping skills and support
Three studies reported children's and adolescents’ qualitative comments about the effect of the intervention on their social life and well-being.Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27,Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31,Reference Barron, Abdallah and Smith32 In addition to finding a small effect (d = 0.35) of reduced impact of trauma on performance at school, students in one of the TRT studiesReference Barron, Abdallah and Smith32 positively appraised their experience. They reported feeling relaxed and optimistic, and that their social communication, self-awareness and self-responsibility had improved. Students in a second studyReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 reported intervention participation as a positive experience at time point 3 (88%), which increased at time point 4 (94.3%). A third studyReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 reported improvement in psychosocial well-being of participants post-intervention, increased ability to trust others and having made more friends.
Study quality and risk of bias
We found evidence of high risk of bias and unclear reporting among several studies included in the review (Table 3). Because of the nature of face-to-face psychological intervention research, blinding of teachers, therapists and researchers was often not possible. Authors of three studies noted this specifically: Qouta et alReference Qouta, Palosaari, Diab and Punam34 mentioned blinding without specific detail, Panter-Brick et alReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 noted that participants and fieldworkers were blinded to group allocation and El-Khani et alReference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 reported that researchers who collected the data were blinded to group allocation. Barron et al and El-Khani et al were the only authors to perform an intention-to-treat analysis.Reference Barron, Abdallah and Heltne33,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35
Table 3 Risk of bias assessment
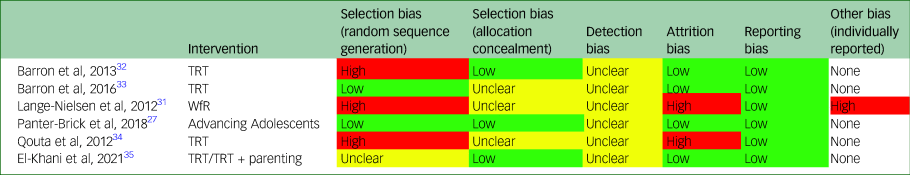
TRT, Teaching Recovery Techniques; WfR, Writing for Recovery.
Selection bias
Random sequence generation
All participants were randomised. Authors of three out of six studies used low-risk randomisation methods (i.e. coin toss).Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27,Reference Barron, Abdallah and Smith32,Reference Barron, Abdallah and Heltne33 Two studies used high-risk methods, including use of consecutive numbers to randomise participantsReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 and group assignment based on gender.Reference Qouta, Palosaari, Diab and Punam34 The last study was ranked unclear risk as they did not mention the randomisation method.Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35
Allocation concealment
Only three studies concealed allocation to intervention and control groups.Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27,Reference Barron, Abdallah and Smith32,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35
Detection bias
Most studies did not address detection bias, except one;Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 however, the information provided was not detailed enough to evaluate bias risk.
Attrition bias
All studies had low attrition rates and detailed expected reasons for drop-out, such as changing school during the study or family moving to new location. Attrition bias risk was identified in two studies; however, because of using high-risk methods to deal with missing data, such as replacing missing data with medianReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 or using an estimation method,Reference Qouta, Palosaari, Diab and Punam34 these methods were deemed unsuitable.
Reporting bias
All studies were evaluated as having low risk of reporting bias.
Other sources of bias
Lange-Nielsen et alReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 reported a study protocol deviation owing to communication difficulties, which meant the waitlist control group completed just one out of two planned assessments before receiving the intervention.
Intervention fidelity
One study made no mention of intervention fidelity.Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 Two studiesReference Barron, Abdallah and Smith32,Reference Barron, Abdallah and Heltne33 assessed programme fidelity by using a questionnaire completed by observers (who observed intervention sessions to assess adherence to the programme) and school counsellors. They were asked about adherence to programme guidelines, programme adaptation and counsellors’ presentation skills. In the first study,Reference Barron, Abdallah and Smith32 counsellors reported a high degree of adherence to the programme (94%), unlike observers (60%). Both agreed on good presentation skills. Programme adaptation reasons were related to supporting students to understand, encouraging them to talk, listening to their experiences and managing session time. In the second study,Reference Barron, Abdallah and Heltne33 counsellors and observers agreed that the guidelines were followed to an acceptable extent, and both agreed on good presentation skills.
Three remaining studies used three methods to evaluate fidelity: for WfR, video recordings showed deviation from the manual, i.e. instructors omitted telling students not to blame themselves;Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 for one study using TRT, weekly supervisory and preparatory meetings with the teacher and the counsellor were employed as a training technique to improve treatment fidelity;Reference Qouta, Palosaari, Diab and Punam34 a second study using TRT provided continued supervision and support via online medial like Skype, WhatsApp and email, in addition to some interviews that were conducted with facilitators.Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35
Discussion
Key findings
The aim of this systematic review was to evaluate the effectiveness of available RCT-assessed psychosocial interventions for children and adolescents who have been exposed to war and conflict in LMICs in the Middle East, and subsequently experience PTSD and other psychological disorders symptoms, compared with control groups. Demographic effects, other beneficial outcomes and/or side-effects were also evaluated.
Previous reviews focusing on children and adolescents in LMICs more broadly found that psychological intervention, especially those that are trauma-focused, may effectively treat PTSDReference Morina, Malek, Nickerson and Bryant22 or have beneficial effect on PTSD symptoms and other psychological problems such as depression and anxiety.Reference Yatham, Sivathasan, Yoon, da Silva and Ravindran8,Reference Purgato, Gross, Betancourt, Bolton, Bonetto and Gastaldon24 But our work highlights unique findings based on LMICs in the Middle East. Two out of three of the included interventions originated from trauma-informed interventions and were delivered in school-based settings. TRT was used in four studies in this reviewReference Barron, Abdallah and Smith32–Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 and was CBT-oriented. The fifth study intervention (WfRReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31) was narrative therapy derived, and the final study used a group psychosocial intervention focusing on well-being in general (Advancing Adolescents).Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 We identified three interventions with promising components, but overall weak evidence of effectiveness. One out of six studies carried out follow-up assessments at 4/5 months.Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 but did not demonstrate any long-term treatment effect. Except for three RCTs evaluating TRT,Reference Barron, Abdallah and Smith32,Reference Barron, Abdallah and Heltne33,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 no other studies demonstrated a statistically significant treatment effect.
Overall, because of the small number of available RCTs, and with samples limited to Palestinian children living in Gaza and the West Bank, and Syrian children living in Jordan and Lebanon, it is not possible to make general statements on the effectiveness of psychological interventions for children and adolescents in LMICs in the Middle East in need of support for PTSD and other psychological disorders. Furthermore, dedicating future research to cover this topic in LMICs in the Middle East is urgent and essential.
Comparison with prior work
Of the three interventions used across six studies, TRT was the only programme that demonstrated a statistically significant reduction in PTSD scores.Reference Barron, Abdallah and Smith32,Reference Barron, Abdallah and Heltne33,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 Results are interpreted cautiously, however, as follow-up assessments were carried out just 2 weeks post-intervention in two studies, which was the shortest follow-up period of all included studies. The third study reported significant reduction up to 12 weeks post intervention, with the best improvement happening at the enhanced TRT group with a parenting component.Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 A lack of long-term effectiveness data has been highlighted by others,Reference Ehntholt, Smith and Yule50,Reference Sarkadi, Ådahl, Stenvall, Ssegonja, Batti and Gavra51 and will be addressed by an upcoming RCT evaluating TRT for refugee children from Middle Eastern LMICs.Reference Sarkadi, Warner, Salari, Fängström, Durbeej and Lampa52 Other previous reviewsReference Barbui, Purgato, Abdulmalik, Acarturk, Eaton and Gastaldon23,Reference Purgato, Gross, Betancourt, Bolton, Bonetto and Gastaldon24 did not specify a certain psychosocial intervention, but found suggestive evidence of decreasing PTSD symptoms of group-based and trauma-focused psychosocial interventions. TRT has been evaluated with children displaced by war living in the UKReference Ehntholt, Smith and Yule50 and Sweden,Reference Sarkadi, Ådahl, Stenvall, Ssegonja, Batti and Gavra51 where statistically significant reductions in post-traumatic symptoms were reported. Qualitative data indicates that TRT may help to normalise experiences, teach coping techniques (i.e. breath control) and facilitate understanding of experience.Reference Sarkadi, Ådahl, Stenvall, Ssegonja, Batti and Gavra51 A strength of TRT is that it could be integrated within existing communities and delivered by a trained professional, such as a teacher, with established rapport among students. The TRT programme can consist of as little as five sessions, which is 50% less than the average of other interventions for children and adolescents in LMICs.Reference Morina, Malek, Nickerson and Bryant22 Implementation may therefore be less susceptible to barriers caused by ongoing armed conflict, lack of financial resources and attrition.
Depression often co-occurs in people affected by war who have PTSD,Reference Morina, Malek, Nickerson and Bryant53 and when we evaluated secondary outcomes, we found this to be the next most commonly assessed variable in five out of six studies. Authors of two studies evaluating TRT reported a significant reduction in depression,Reference Barron, Abdallah and Smith32,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 consistent with past researchReference Sarkadi, Ådahl, Stenvall, Ssegonja, Batti and Gavra51 and results of a past systematic review conducted with youth in LMICs.Reference Yatham, Sivathasan, Yoon, da Silva and Ravindran8 Aside from this, we also found that participants gained clinically significant psychosocial benefits from two interventions (TRTReference Barron, Abdallah and Smith32,Reference Barron, Abdallah and Heltne33 and WfRReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31), such as improvements in school performance, communication, number of friends, self-awareness and self-responsibility. In settings where children and adolescents may be separated from their parentsReference Barron, Abdallah and Heltne33 and social structures fractured by conflict, support and connectedness are especially important for building self-esteem that can be protective in the face of psychological concerns.Reference Betancourt and Williams54 Findings from the Advancing Adolescents studyReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 and one TRT studyReference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 indicated that participants felt reduced insecurity, distress and mental health difficulties, which are important for building resilience.Reference Dray, Bowman, Campbell, Freund, Wolfenden and Hodder55 In one TRT study, non-medical factors such as school performance were assessed as a proxy for psychosocial well-being, and it was argued in this study that the TRT intervention allowed children and adolescents to understand educational gains, suggesting an improvement in student perception of learning capacity.Reference Barron, Abdallah and Smith32 These non-medical elements are important as they reflect another aspect of coping with daily stressors that may be supportive without necessarily resulting in a measurable health effect.
The presence of adverse outcomes in several studies warrants attention. Study authors reported adverse effects following two out of three interventions (TRTReference Qouta, Palosaari, Diab and Punam34 and WfRReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31), including increased distress and depression. Several possible causes may explain these findings. First, timing of data collection is important, particularly as mental health symptoms may fluctuate over time.Reference Miller-Graff and Cummings56 Authors of the WfR studyReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 noted an increase in depression scores between the intervention and first follow-up (time point 2). They suggest that the short follow-up interval (19 days) and effect of recalling traumatic memories might have caused this elevation. This is supported by the decrease in depression scores between time points 3 and 4, and the overall non-significant difference between scores for time points 1 and 4. A second explanation is that interventions may have differential effects on individuals and subgroups. For instance, a previous studyReference Karam, Fayyad, Karam, Tabet, Melhem and Mneimneh57 found that children from one classroom with high exposure to war appeared to account for the significant difference in depression scores, compared with those with low exposure.Reference Karam, Fayyad, Karam, Tabet, Melhem and Mneimneh57 In one study by Barron et al, increased depression scores were only recorded for girls in the control group post-test; however, this might be because of higher exposure to war stressors reported pre-test by girls in the control group.Reference Barron, Abdallah and Heltne33 Others have suggested that in areas where conflict is ongoing, the uncertainty and lack of resolution may be an independent risk factor for trauma responses.Reference Kolltveit, Lange-Nielsen, Thabet, Dyregrov, Pallesen and Johnsen58
Findings from this review suggest limited effectiveness of psychosocial and psychological interventions consistent with one previous systematic review that included adults and children sample in LMICs;Reference Purgato, Gastaldon, Papola, Van Ommeren, Barbui and Wa5 however, this may also reflect the challenging circumstances under which the research takes place.Reference Thompson, Vidgen and Roberts59 War exposure adds complexity to undertaking research,Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31,Reference Qouta, Palosaari, Diab and Punam34 and was high across all included studies. Interventions used with Syrian refugees were implemented in post-war settings, as studies were done in host countries like Jordan and Lebanon;Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 however, conflict was still ongoing in Syria. In the other included studies, intervention implementation or data collection were during an ongoing conflict.Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31–Reference Barron, Abdallah and Heltne33 Experiences of shelling and bombardment were high across three studies (79–86%), based in Nablus,Reference Barron, Abdallah and Heltne33 GazaReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 and Jordan.Reference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27 For interventions to be feasible in war-affected environments, they must address the impact of ongoing conflict on mental health and everyday life.Reference Miller-Graff and Cummings56 Treatment effects may be underestimatedReference Barron, Abdallah and Smith32 or lost in a situation where violence is reoccurring.Reference Thabet, Vostanis and Karim60 Certain communities or districts can also be affected at different times,Reference Miller-Graff and Cummings56 affecting results. Although some argue that offering an intervention post-war may achieve better results,Reference Karam, Fayyad, Karam, Tabet, Melhem and Mneimneh57 there is a clear need for interventions that fit the needs of children and adolescents who live and grow up in conflict and war-affected settings.
Future research
In five out of six studies, authors confirmed that the interventions were culturally accepted and appropriate or suitable with low-resource settings (TRTReference Barron, Abdallah and Smith32–Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 and Advancing AdolescentsReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27). For instance, in one study, trained local researchers reviewed content to ensure culturally sensitive interpretations were adopted.Reference Barron, Abdallah and Heltne33 The same studyReference Barron, Abdallah and Heltne33 considered TRT to be culturally appropriate according to previous research results from school counsellors and adolescents in Palestine.Reference Barron, Abdallah and Smith32 This is important in research where Western interventions are adapted for non-Western settings, as this may affect intervention acceptability and implementation,Reference Miller-Graff and Cummings56 and has been recommended for future research in a previous reviewReference Yatham, Sivathasan, Yoon, da Silva and Ravindran8 highlighting the importance of culturally appropriate assessment of local needs. For instance, although the success of interventions may be enhanced by a supportive adult or caregiver working to support the child throughout the process, this person may not be available in LMICs,Reference Murray, Dorsey, Skavenski, Kasoma, Imasiku and Bolton61 as was observed in several studies included with the review, either because of the lack of knowledge about psychosocial support or the nature of war settings, where one or both parents might be dead or missing. Additionally, the type of relationship between the child or adolescent and their caregiver may differ in distinct contexts.Reference Murray, Dorsey, Skavenski, Kasoma, Imasiku and Bolton61 Evidence suggests that collaborating with local organisations, consulting local mental health specialistsReference Murray, Dorsey, Bolton, Jordans, Rahman and Bass62 and understanding the differences in relationship between caregiver and child or adolescent in different culturesReference Murray, Skavenski, Bass, Wilcox, Bolton and Imasiku63 may all help to adapt Western-developed interventions in LMICs.
We observed several methodological factors that could be addressed in future research of this nature. First, all studies used self-report measures without utilising a rigorous, systematic evaluation for clinical diagnoses. We also found frequent unclear reporting of methods that hindered a full quality assessment. None of the included studies demonstrated that their methods were bias free; however, four studiesReference Panter-Brick, Dajani, Eggerman, Hermosilla, Sancilio and Ager27,Reference Barron, Abdallah and Smith32,Reference Barron, Abdallah and Heltne33,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 were evaluated as having the least risk of bias out of the group. Potential for bias was most common when high-risk methods of randomisation were used, based on genderReference Qouta, Palosaari, Diab and Punam34 or use of consecutive numbersReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 to determine group allocation. Random sequence generation, such as use of a coin toss or computer-based generation methods, can improve methodological rigor and should be considered where possible by future researchers.
All included studies used classroom or group/community-based interventions rather than one-to-one therapy, which is expected because of the lower cost of group interventions and lack of CAP services in LMICs in the Middle East. We found variable implementation and cost-effectiveness data reported across the included studies, which is problematic because this information is essential for those tasked with implementation. Intervention fidelity was assessed in fiveReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31–Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 out of six included studies; however, many of the self-report methods used were subject to bias. Use of videotaping and objective evaluation was employed in one study,Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 and is considered a more accurate method to assess treatment fidelity;Reference Murray, Dorsey, Bolton, Jordans, Rahman and Bass62 however, this is not always feasible in war-affected settings.Reference Karam, Fayyad, Karam, Tabet, Melhem and Mneimneh57 Cost-effectiveness data were reported in one out of six studies,Reference Barron, Abdallah and Heltne33 calculated at US$38.68 per student participating in TRT. Although this may seem inexpensive, in LMICs where there are shortages in basic needs such as food, water and housing, these are prioritised over psychological interventions and research.Reference Barenbaum, Ruchkin and Schwab-Stone64 Nevertheless, where possible, researchers should report implementation data such as cost-effectiveness,Reference Murray, Dorsey, Bolton, Jordans, Rahman and Bass62,Reference Kieling, Baker-Henningham, Belfer, Conti, Ertem and Omigbodun65 as this will help guide decision-makers in the context of limited resources and healthcare funding.Reference Kernick66
El-Khani et alReference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 highlighted their success in implementing the TRT intervention online as a result of the COVID-19 pandemic, and the feasibility of such implementation. They proposed that using technology for online implementation would have potential benefits for settings lacking accessibility to such services, increase opportunities in LMICs,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 and prevent further lack of services and marginalisation owing to the COVID-19 pandemic. Further studies are needed to address this point and to understand the effect of COVID-19 on such interventions (which is beyond the scope of this study).
The heterogeneity of included interventions – in terms of target problems and underpinning theoretical orientation – means that inferences from this review must be made with caution. One included intervention was a group of community-based activities to provide psychosocial care in non-clinical sittings. And the two other interventions were trauma-informed, either CBT or narrative therapy oriented. The TRT intervention was described in three studiesReference Barron, Abdallah and Smith32,Reference Barron, Abdallah and Heltne33,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 as having trauma-focused components or derived from trauma-focused CBT; however, it might be argued that it is a trauma-informed rather than trauma-focused intervention, because of the trauma-specific skills-based nature of the intervention, and that the trauma-focused components are not sufficient compared with traditional trauma-focused CBT. The WfR intervention required participants to write in detail about traumatic events, but the briefness of the intervention and non-guided narration also means that it is better classified as trauma informed. Although, trauma-informed interventions are recommended for surveillance of trauma, and enhancing resilience in children with adverse childhood experiences,Reference Oral, Ramirez, Coohey, Nakada, Walz and Kuntz67 only trauma-focused interventions are recommended by the National Institute for Health and Care Excellence as a first-line treatment for PTSD.68 These points need to be addressed in more detail in future studies comparing effectiveness of trauma-informed versus trauma-focused interventions implemented with war-affected children.
Training and supervision for personnel providing psychosocial interventions are important elements for future research, as the lack of available mental health professionals is a major barrier for intervention implementation in LMICs.Reference Saraceno, van Ommeren, Batniji, Cohen, Gureje and Mahoney69 Often facilitators in low- and middle-income settings deliver high psychosocial interventions with little to no mental health background, often referred to as task-sharing or task-shifting.Reference Murray, Dorsey, Skavenski, Kasoma, Imasiku and Bolton61 Despite this, five out of six studies were evaluated as having an appropriate professional to deliver the intervention. Most had either a formal mental health background,Reference Barron, Abdallah and Smith32–Reference Qouta, Palosaari, Diab and Punam34 were teachers trained specifically to deliver the interventionReference Drescher, Kiselev, Akhtar, Acarturk, Bryant and Ilkkursun25,Reference El-Khani, Cartwright, Maalouf, Haar, Zehra and Çokamay-Yılmaz35 or used interventions that did not require mental health background.Reference Lange-Nielsen, Kolltveit, Aziz, Thabet, Dyregrov and Pallesen31 Although the task-shifting model may be desirable and cost-effective, the availability of supervision and training is still needed for lay counsellors,Reference Murray, Dorsey, Bolton, Jordans, Rahman and Bass62 non-mental health professionals and families involved with service delivery.Reference Saraceno, van Ommeren, Batniji, Cohen, Gureje and Mahoney69 For circumstances where facilitators have minimal mental health training, preliminary research suggests that it may be feasible for remote supervision to be provided,Reference El-Khani, Cartwright, Ang, Henshaw, Tanveer and Calam70 where specialist mental health services are unavailable locally.
Strengths and limitations of the review
To our knowledge, this is the first systematic review focusing on interventions for children and adolescents with PTSD in LMICs in the Middle East. We carried out a detailed review of each study and found several key areas for future researchers to build upon, including the need for follow-up and cost-effectiveness data. RCTs are considered to produce the highest-quality evidence, and so were the intended focus of our review. However, as such study designs tend to be labour-intensive and expensive, they are comparatively rare in LMICs. Important findings from other study designs may therefore have been missed by our review parameters. Given the lack of evidence in this area, future reviewers may consider expanding the age range to include young adults and older adolescents, and to include other conflict-related causes of PTSD, such as state-sponsored violence (e.g. police torture and abuse), as some countries in the Middle East do not suffer from ongoing war but there is widespread violence, identity/ethnic-related attacks and other forms of political violence. It is well-known that RCT results are commonly affected by variability in conditions and populations,Reference Cook and Thigpen71 and therefore may not always be feasible in settings affected by ongoing conflict.Reference Betancourt and Williams54 Challenges in publishing peer-reviewed research from LMICs are identified across many areas of health researchReference Jones and Geneau72 and are not isolated to research on psychological support alone. Studies not published in peer-reviewed journals or English language might have been missed. Inter-rater reliability and kappa statistic about decisions to include studies were not conducted or reported. Finally, we deviated from PROSPERO record by including one study with the age range of 18 years and under (rather than all under 18 years). However, as the average age group for this study was comparable with other included studies, we believe any effect from this adjustment would be negligible, and data was not pooled for quantitative analysis.
In conclusion, this review highlights a paucity of robust evidence on available treatment options for refugee and displaced children and adolescents affected by war from LMICs in the Middle East. Based on the evidence presented, it was not possible to make conclusions regarding the efficacy of the psychosocial interventions for our targeted population, which is also indicative of the broader problem identified from our review, being that there is not enough research in this area. The evidence presented points to a need for continued efforts in developing effective interventions that support children and adolescents affected by war and displacement. Some results are encouraging, as participants reported the acquisition of new social and coping skills, which are needed amid post-war and ongoing conflict, to provide children and adolescents with a sense of safety and stability. Given that several studies reported adverse effects for some interventions, further attention must be given to intervention development and implementation to support this vulnerable population.
Author contributions
A.F.A. and A.R.M. wrote the manuscript, with significant input from M.A.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Declaration of interest
None.
Appendix 1 Detailed Search Methodology

Appendix 2 Excluded Studies









eLetters
No eLetters have been published for this article.