Polycystic ovary syndrome (PCOS) is one of the most common hormonal, inflammatory and oxidant disorders among women of reproductive age worldwide(Reference De Leo, Musacchio and Cappelli1). PCOS has been known as the leading cause of infertility among women(Reference Alchami, O’Donovan and Davies2). Approximately, 70 % of women with PCOS have infertility(Reference Melo, Ferriani and Navarro3). These patients may have missed, irregular or prolonged menstrual cycles or high levels of androgens. Follicles cannot grow and mature due to exceptional levels of sex hormone. Thus, ovaries may store numerous immature follicles and fail to release an egg regularly(Reference Jonard and Dewailly4).
N-acetylcysteine (NAC) is a safe, economic and affordable drug which is used for the stimulation of ovulation(Reference Ghomian, Khadem and Moeindarbari5). This medication is an acetylated variant of l-cysteine, a great source of sulfhydryl groups. NAC is recognised as an antioxidant agent that can directly scavenge reactive oxygen species and is beneficial for PCOS patients. In a meta-analysis study, beneficial effects of NAC supplementation on IL-8, malondialdehyde and homocysteine levels have been shown. TNF-α and IL-6 levels could be positively impressed by NAC(Reference Faghfouri, Zarezadeh and Tavakoli-Rouzbehani6). Also, NAC has several biologic impacts, such as reducing insulin resistance, regulating the insulin receptor in human erythrocytes and influencing the insulin secretion in pancreatic β-cells. Also, NAC has other anti-inflammatory characteristics by increasing the cellular levels of glutathione (GSH) and promoting apoptosis in PCOS patients(Reference Teimouri, Mollashahi and Paracheh7).
Oligo ovulation or anovulation is the most common cause of infertility in PCOS women. Thus, induction of regular ovulation is vital for these patients. In subjects with PCOS, NAC can reduce insulin and testosterone levels and facilitate serum levels of homocysteine and lipid profile(Reference Alchami, O’Donovan and Davies2). Teimouri et al. showed that adding NAC supplements to letrozole was efficient for fertility rate and the number of ovulatory follicles in women with PCOS(Reference Teimouri, Mollashahi and Paracheh7).
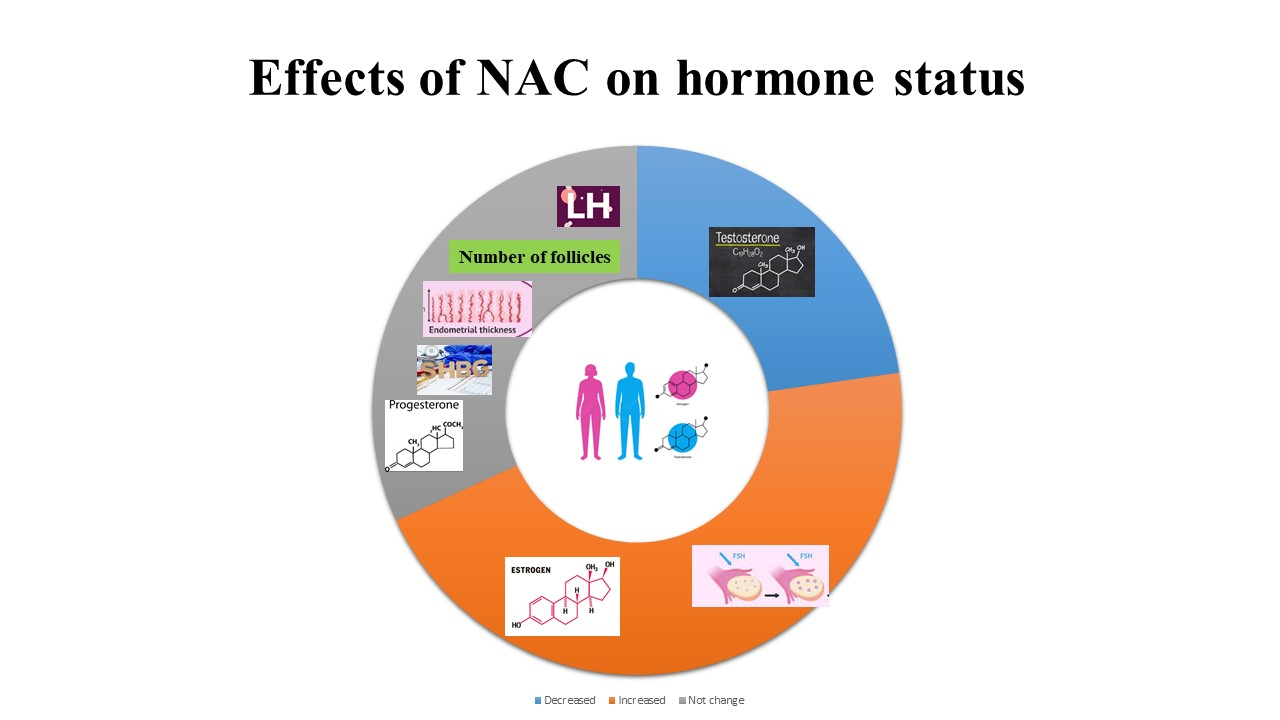
NAC supplementation could increase the average number of ovulatory follicles >18 mm and peak endometrial thickness in PCOS women(Reference Maged, Elsawah and Abdelhafez8). Treatment with NAC induces ovulation, decreases miscarriage rates and increases live birth rates(Reference Nasr9). Also, among infertile males, NAC consumption improves the sperm parameters and oxidative stress as low levels of follicle-stimulating hormone (FSH) and luteinising hormone (LH) and high levels of testosterone, increased sperm count and motility and decreased abnormal sperm morphology and DNA fragmentation(Reference Jannatifar, Parivar and Roodbari10). Other potential effects of NAC for PCOS patients are lowering androgen levels, regulating menstrual cycles, increasing the follicle size, decreasing hirsutism, free testosterone and menstrual irregularity(Reference Oner and Muderris11).
Indeed the role of NAC on sexual hormones is characterised as decreased serum levels of testosterone and androgen levels among PCOS women, reduced levels of FSH and LH and increased levels of testosterone in infertile men(Reference Ghomian, Khadem and Moeindarbari5). Also, serum levels of oestradiol (E2) and progesterone were improved in PCOS women after NAC consumption(Reference Nasr9). Results of a recent study showed no effect of NAC on levels of FSH, LH and FSH/LH ratio among infertile PCOS women(Reference Nemati, Nemati and Taheri12). In another study, NAC supplementation had no significant effect on serum levels of sex hormone-binding globulin (SHBG), LH, FSH, LH/FSH, E2 and testosterone in PCOS patients after 12 weeks(Reference Ghomian, Khadem and Moeindarbari5,Reference Nasr9,Reference Nemati, Nemati and Taheri12,Reference Badawy, State and Abdelgawad13) .
In animal studies, E2 and progesterone levels were not changed after NAC supplementation in the serum of goats(Reference Luo, Ao and Duan14). It has been also revealed that levels of hormones and spermatogenesis were not different among adult male Wistar rats following NAC consumption(Reference Shahrzad, Shariati and Naimi15). However, acrylamide and NAC supplementation enhanced FSH, LH and testosterone levels(Reference Shahrzad, Shariati and Naimi15). In another in vivo study, a reduction in levels of testosterone and an increase in levels of LH and FSH were seen after NAC supplementation among adult male Wistar rats(Reference Moghadam, Shariati and Naeimi16).
Hyperandrogenism and anovulation are characterised by insulin resistance and hyperinsulinaemia. Thus, reducing insulin resistance is an efficient approach in these patients(Reference Carmina and Azziz17). Numerous studies have indicated that NAC is effective for the induction of ovulation and pregnancy rates in PCOS patients. On the other hand, NAC might increase the chance of pregnancy(Reference Maged, Elsawah and Abdelhafez8,Reference Hassan, Alalfy and Hassan18) .
Considering several benefits of NAC in patients with PCOS, there is still unresolved controversy among clinical trials investigating the efficiency of NAC supplementation in improving ovulation and sex hormones profile in PCOS patients. Therefore, the present meta-analysis aimed to evaluate the effects of NAC supplementation on infertility parameters such as ovulation biomarkers and serum levels of sex hormones in women with PCOS.
Materials and methods
A systematic search was conducted in the international scientific databases, including PubMed, Embase, Web of Science, Scopus and Cochrane Central Library, for relevant studies published up to September 2021. In the search strategy, only studies in English were included. MeSH terms and keywords were used. The search was conducted using the following search pattern: ‘Acetylcysteine’ [Mesh] OR ‘acetylcysteine’ [tiab] OR ‘nacetylcysteine’ [tiab] OR ‘n-acetyl cysteine’ [tiab]) OR ‘NAC’ [tiab] AND ‘ovulation’ [Mesh] OR ‘total testosterone’ [tiab] OR ‘progesterone’ [tiab] OR ‘sexual function’ [tiab] OR ‘impotence/erectile/dysfunction’ [tiab] OR ‘sex hormone-binding globulin (SHBG) ’ [tiab] AND ‘Polycystic Ovary Syndrome’ [tiab] OR ‘Ovary Syndrome’ [tiab] OR ‘Polycystic Syndrome’ [tiab] OR ‘Polycystic Ovary’ [tiab] OR ‘Polycystic ovary disease’ [tiab] OR ‘Stein-Leventhal Syndrome’ [tiab] OR ‘Stein Leventhal Syndrome’ [tiab] OR ‘Syndrome, Stein-Leventhal’ [tiab] OR ‘Sclerocystic Ovarian Degeneration’ [tiab] OR ‘Ovarian Degeneration, Sclerocystic’ [tiab]. The wild-card term‘*’ was used to increase the sensitivity of our search strategy. Only studies in English were included in the meta-analysis. In addition to searching in databases, we checked the references of related articles for any missing eligible articles (hand-search method). It should be noted that the protocol was not registered at the registry of systematic reviews/meta-analyses (PROSPERO).
Inclusion and exclusion criteria
We included potentially relevant studies if they met the following inclusion criteria: (a) original randomised clinical trials with either parallel or cross-over design; (b) supplementation with NAC in one group in comparison with a placebo group and (c) reporting means and sd at least for one of the following parameters: number of follicles, endometrial thickness, total testosterone (TT), progesterone, LH levels, FSH levels, E2 and SHBG.
In addition, the following studies were excluded: in vitro, in vivo, ex vivo studies, case reports, observational studies (cross-sectional, case–control, cohort) and quasi-experimental studies. Studies supplemented NAC along with other interventions. Besides, studies on pregnant and lactating women were excluded.
Data extraction
Two independent reviewers evaluated the articles following the inclusion criteria. As a first step, titles and abstracts were reviewed. Then, relevant studies were assessed to ensure the suitability of a study for full-text assessment. Any disagreement was resolved by discussion with the senior author.
From the selected studies, the following data were extracted: first author’s name, publication year, sample size, study location, mean age of participants, intervention (type, dose, and duration of supplementation), study design and end-point values (as means and sd) for the number of follicles, endometrial thickness, TT, progesterone, serum LH levels, serum FSH levels, E2 and SHBG in both intervention and control groups.
Risk of bias assessment
The Cochrane Collaboration’s risk of bias tool was employed to assess the risk of bias for each study(Reference Higgins, Altman and Gøtzsche19). The tool consists of seven domains, including random sequence generation, allocation concealment, performance bias, reporting bias, detection bias, attrition bias and other sources of bias. If the study contains a methodological defect that may affect its findings, the study was given a ‘high risk’ score; if there was no defect for that domain, a ‘low risk’ score; if the information was insufficient to determine the effect, an ‘uncertain risk’ score. If the trial had ‘low risk’ for all domains, a high-quality study was considered a low risk of bias. Risk bias assessments were conducted independently by two reviewers.
Data synthesis and statistical analysis
To obtain the overall effect size, means and sd of after values in the NAC and control groups were analysed. We utilised a random-effects model to get the overall effect size if the amount of between-study heterogeneity was significant. Heterogeneity was determined using I 2 statistics and Cochrane’s Q test. I 2 value >50 % or P < 0·1 for the Q test was considered significant heterogeneity. If heterogeneity was not significant, the fixed-effects model was employed to estimate the overall effect size. To detect potential sources of heterogeneity, subgroup analyses were performed according to the predefined variables, including duration of the intervention, NAC dosage, study location and the type of control. The sensitivity analysis was used to identify the dependence of overall effect size on a single study. The small-study effect was evaluated by the formal tests of Egger’s and Begg’s. Publication bias was determined by visual inspection of the funnel plot. In the presence of publication bias, trim and fill analysis was used to simulate a model without publication bias presenting a new effect size by inserting new fictitious studies. All the statistical analyses were performed using Stata, version 16 (Stata Corp.). P < 0·05 was considered as the significance level.
Results
Selected studies and systematic review
A total of 931 articles were obtained from a systematic search of electronic databases. After removing duplicate papers and screening the articles carefully by the title and abstract, thirty-five papers were included. Seventeen articles after the full-text review were excluded. Overall, eighteen articles met the inclusion criteria and enrolled in the meta-analysis. Two of them were from the hand-search of the related articles. The flow diagram of the literature search process is presented in online Supplementary Fig. 1. Overall, eighteen clinical trials published between 2002 and 2021 were included in the meta-analysis. Table 1 summarises the characteristics of the included studies. The mean age of participants was from 23 to 29 years. In addition, nine studies of these studies were performed in Egypt(Reference Badawy, State and Abdelgawad13,Reference Hassan, Alalfy and Hassan18,Reference Badawy, El Nashar and El Totongy20,Reference Elnashar, Fahmy and Mansour21,Reference Hashim, Anwar and El-Fatah22,Reference Nasr9,Reference Elgindy, El-Huseiny and Mostafa23,Reference Maged, Elsawah and Abdelhafez8,Reference El Sharkwy and Abd El Aziz24) , four in Iran(Reference Nemati, Nemati and Taheri12,Reference Ghomian, Khadem and Moeindarbari5,Reference Teimouri, Mollashahi and Paracheh7,Reference Cheraghi, Mehranjani and Shariatzadeh25) , two in Turkey(Reference Kose and Naziroglu26,Reference Oner and Muderris11) , two in India(Reference Chandil, Pande and Sen27,Reference Gayatri, Kumar and Kumar28) and one in Italy(Reference Fulghesu, Ciampelli and Muzj29). NAC was administered in various doses, from 1·2 to 1·8 g. The duration of the intervention varied from 5 d to 24 weeks among the studies.
Table 1. Study characteristics of included studies

NR, not reported; Con, control; PCOS, polycystic ovary syndrome; NAC, N-acetylcysteine.
Risk of bias assessment
The results of evaluating the quality of the included studies are presented in online Supplementary Fig. 2. Overall, five studies were defined as high quality(Reference Hassan, Alalfy and Hassan18,Reference Badawy, El Nashar and El Totongy20,Reference El Sharkwy and Abd El Aziz24,Reference Kose and Naziroglu26,Reference Ghomian, Khadem and Moeindarbari5) . In the study by Gayatri et al. (Reference Gayatri, Kumar and Kumar28), participants were not randomly assigned to the intervention and control groups, and seven studies described an allocation concealment method(Reference Hassan, Alalfy and Hassan18,Reference Badawy, El Nashar and El Totongy20–Reference Hashim, Anwar and El-Fatah22,Reference Elgindy, El-Huseiny and Mostafa23,Reference Ghomian, Khadem and Moeindarbari5,Reference Maged, Elsawah and Abdelhafez8) . The blinding of subjects and researchers was reported in four studies(Reference Hashim, Anwar and El-Fatah22,Reference Nasr9,Reference Chandil, Pande and Sen27,Reference Gayatri, Kumar and Kumar28) . In three studies, several patients did not complete the study and had a high risk of bias in the incomplete outcome data domain(Reference Oner and Muderris11,Reference Kose and Naziroglu26,Reference Fulghesu, Ciampelli and Muzj29) .
Effects of N-acetylcysteine on number of follicles
A pooled analysis of eight effect sizes with seven studies (subjects = 1888; intervention, 970; control, 918) on the number of follicles revealed no significant effect following the intervention (weighted mean difference (WMD): −0·10; 95 % CI (−1·02, 0·82), P = 0·829) (online Supplementary Fig. 3). The level of heterogeneity was considerable (I 2 = 99·4 %, ‘P < 0·001’), which was reduced with subgrouping by country, treatment dosage, type of control and duration of studies. There were no significant changes in results following subgroup analysis (Table 2). Removing an individual research at a time by sensitivity analysis did not affect the results. Begg’s test revealed no presence of small-study effects (P = 0·536).
Table 2. Subgroup analyses for the effects of N-acetylcysteine on ovulation and sex hormones profile (95 % confidence intervals)

WMD, weighted mean difference; SMD, standardised mean difference; LH, luteinising hormone; FSH, follicle-stimulating hormone; E2, oestradiol; NR, not reported.
Effects of N-acetylcysteine on endometrial thickness
The effects of NAC on endometrial thickness were reported in eleven studies with thirteen effect sizes (subjects = 2663; intervention, 1356; control, 1307). The analysis indicated no significant change in endometrial thickness by NAC (WMD = 0·11 mm; 95 % CI (-0·95, 1·17), P = 0·839) (online Supplementary Fig. 4(a)). A significant between-study heterogeneity was observed (I 2 = 99·3 %, ‘P < 0·001’). The type of control and study location were identified as sources of high heterogeneity following subgroup analysis. In addition, according to the subgroup analysis, there was a significant increase in endometrial thickness in studies conducted in Egypt (P = 0·025) (Table 2). Sensitivity analysis determined that no particular study likely affected the pooled results. We found significant small-study effects using Egger’s but not Begg’s tests (‘P < 0·001’ and P = 0·161, respectively). Furthermore, visual inspection of the funnel plot revealed the asymmetric distribution (online Supplementary Fig. 4(b)). Thus, trim and fill analysis was conducted with five imputed studies. The corrected effect size for publication bias showed significant changes after trim and fill analysis (WMD = −1·385 mm; 95 % CI (−2·736, −0·034), P < 0·05) (online Supplementary Fig. 4(c)).
Effects of N-acetylcysteine on luteinising hormone
Overall, ten effect sizes from eight studies with 990 participants (intervention, 509; control, 481) have examined the effects of NAC supplementation on LH, revealing no significant changes in NAC group compared with control group (standardised mean difference = 0·10 mg/ml; 95 % CI (−0·12, 0·33), P = 0·365) (online Supplementary Fig. 5(a)). Significant heterogeneity was seen among the studies (I 2 = 61 %, P = 0·006). Study location, treatment duration and type of control were detected as sources of heterogeneity following subgroup analysis (Table 2). Sensitivity analysis demonstrated that the overall effect size regarding the effects of NAC on LH did not depend on one individual study. No small-study effects were found using Egger’s and Begg’s tests (P = 0·927 and 1·00, respectively). Moreover, funnel plot visual inspection revealed no sign of publication bias (online Supplementary Fig. 4(b)).
Effects of N-acetylcysteine on oestradiol
According to the eight studies with ten effect sizes on 2160 individuals (intervention, 1119; control, 1041), NAC supplementation did not significantly affect E2 levels (WMD = −15·96 pg/ml; 95 % CI (−35·54, 3·62), P = 0·110) (online Supplementary Fig. 6(a)). There was a significant between-study heterogeneity (I 2 = 94·4 %, ‘P < 0·001’), which was decreased with subgrouping by type of control, study location, treatment dosage and duration of studies (Table 2). Subgroup analysis showed that NAC supplementation significantly decreased E2 levels when the supplementation was accompanied by metformin (P = 0·019). Moreover, supplementation with a higher dosage of NAC (1·8 g/d) had a considerable impact on decreasing E2 compared with lower doses (1·2 g/d) (P = 0·049). Sensitivity analysis demonstrated no evidence of the impact of a single study on the results. The Egger’s and Begg’s tests showed no significant small-study effect (P = 0·444 and P = 0·721, respectively). In addition, publication bias was revealed by visual inspection of the funnel plot (online Supplementary Fig. 6(b)). Thus, trim and fill analysis was done with four imputed studies resulting in a significant change in the results (WMD = −0·390 pg/ml; 95 % CI (−0·728, −0·052), P < 0·05) (online Supplementary Fig. 6(c)).
Effects of N-acetylcysteine on follicle-stimulating hormone
A significant increase in FSH levels was observed by NAC supplementation in the combined analysis of six studies with seven effect sizes (subjects = 610; intervention, 319; control, 291) (standardised mean difference: 0·39; 95 % CI (0·07, 0·71); P = 0·01) (online Supplementary Fig. 7(a)). Significant between-study heterogeneity (I 2 = 70·9 %, P = 0·002) was reduced by subgrouping by study location, treatment duration and type of control (Table 2). By removing El Sharkwy et al. (Reference Maged, Elsawah and Abdelhafez8) (effect size (ES): 0·37 mg/ml, 95 % CI (−0·04, 0·78)) and Nemati et al.(Reference Nemati, Nemati and Taheri12) (ES: 0·34 mg/ml, 95 % CI (−0·41, 0·72)) studies, the significant effects of NAC on FSH levels became non-significant. The result of Begg’s tests was not significant in identifying small-study effects (P = 0·764).
Effects of N-acetylcysteine on total testosterone
Combining the data of six studies with eight effect sizes (subjects = 725; intervention, 369; control, 356) showed a significant effect of NAC on TT levels (standardised mean difference: −0·25; 95 % CI (−0·39, −0·10); ‘P < 0·001’) (online Supplementary Fig. 7(b)). There was a significant between-study heterogeneity (I 2 = 53·9 %, P = 0·034) in which the study location and duration of studies were revealed as the sources of heterogeneity following subgroup analysis. Performing subgroup analysis revealed that the effects of NAC on TT levels in studies with intervention duration ≥ 8 weeks were more robust than the entire sample (Table 2). Sensitivity analysis revealed that no single study likely affected the pooled results. There were no significant small-study effects using Begg’s test (P = 0·764).
Effects of N-acetylcysteine on progesterone
The pooled results of five studies (subjects = 1842; intervention, 947; control, 895) indicated that there were no significant effects of NAC supplementation on progesterone (WMD = −0·29, 95 % CI (−2·47, 1·89); P = 0·794) (online Supplementary Fig. 8(a)). There was considerable between-study heterogeneity (I 2 = 99·5 %, ‘P < 0·001’). No subgroup analysis was performed on studies. No significant difference in overall effect size was shown after removing each study using sensitivity analysis. The results of Begg’s test revealed no presence of a small-study effect (P = 0·806).
Effects of N-acetylcysteine on sex hormone-binding globulin
Pooling data from four studies with five effect sizes (subjects = 414; intervention, 220; control, 194) showed no significant effect of NAC supplementation on SHGB levels (WMD: 1·68 nmol/l, 95 % CI (−2·10, 5·45), P = 0·383) (online Supplementary Fig. 8(b)). No heterogeneity was detected among studies (I 2 = 0·0 %, P = 0·851). Subgroup analysis was not performed due to the low number of studies. Sensitivity analysis revealed that the overall effect size did not depend on one individual study. No significant small-study effects were performing Begg’s test (P = 0·806).
Discussion
Pooled analysis of eighteen randomised clinical trials with a total population of 3161 in the current study revealed that NAC supplementation had significant increasing and decreasing effects on FSH and TT levels, respectively. However, the elimination of publication bias using trim and fill analysis revealed that NAC also could decrease E2 levels and endometrial thickness. Country, type of control and intervention duration were the possible sources of high heterogeneity in the pooled analyses.
Several studies have investigated the effectiveness of NAC in the reproductive performance of females. Mona et al. showed that NAC administration before the chemotherapy could improve reproductive functions and the gonadal hormone disturbance in female rats through its protective effects against oxidative stress(Reference Helal30). Naimi et al. reported that NAC alone had no significant beneficial effect on the number of ovarian follicles and the levels of hormones in adult rats. However, in a dose-dependent manner, its combination with acrylamide led to the significant elevation of the number of ovarian follicles and the levels of FSH, E2 and progesterone(Reference Naimi, Shariati and Naimi31). This was in line with our finding on E2 levels. However, due to the limited range of administered dosages of NAC, subgroup analysis based on the dosage was not performed on LH, FSH and TT levels. Performed pooled analyses on the number of follicles and endometrial thickness revealed that the effects of NAC on these variables were not in a dose-dependent manner. Furthermore, it has been demonstrated that higher doses of NAC (1·8 g/d) have decreasing effects on E2 levels compared with lower doses. This result could be explained with respect to the fact that E2 might be dose-dependent in response to NAC. Previous studies showed that with different doses of NAC, different effects could be observed(Reference Cavallini, Ferraretti and Gianaroli32). For example, NAC consumption at a dose of 1·8 g/d for 12 weeks showed improvement in ovulation and pregnancy rates among patients with PCOS compared with 1·2 g daily after 12 weeks(Reference Nemati, Nemati and Taheri12,Reference Nasr9) . Also, it has been shown that a longer duration of supplementation might be more effective. It is difficult to achieve desirable and continuous results in a short intervention time. For example, a study with supplementation of 1·8 g/d for 6 weeks compared with another NAC intervention with 1·8 g/d for 24 weeks; changes in fasting glucose or fasting insulin were not significant in the first study; however, these biochemical markers were improved significantly in the second study. A decline in TT was reported in both studies(Reference Elnashar, Fahmy and Mansour21,Reference Chandil, Pande and Sen27) .
Subgroup analysis based on the country showed that the improving effects of NAC on the endometrial thickness are more significant in some countries. This could be due to the differences in ethnicity of participants. Epigenetic and environmental changes are various in different countries, and this issue may lead to different responses to NAC supplementation(Reference Diamanti-Kandarakis, Kandarakis and Legro33). However, due to the limited number of countries in which studies have been performed, exact interpretation of this issue must be with precaution.
In addition, NAC increases the cellular levels of antioxidants and reduces GSH at higher doses. Therefore, NAC can potentially improve insulin receptor activity in human erythrocytes and improve insulin secretion in response to glucose(Reference Badawy, State and Abdelgawad13).
It has been shown that BMI, alcohol use and smoking influence E2 serum levels(Reference Sriprasert, Kono and Karim34). Recent studies showed that BMI and E2 levels have positive association. Women with high BMI score had high E2 levels. Indeed, increased E2 levels among overweight and obese postmenopausal women were due to the increased fat mass and E2 production in adipose tissue(Reference Gruber, Tschugguel and Schneeberger35). Rinaldi et al. showed that intake of alcohol increased serum levels of dehydroepiandrosterone sulphate, testosterone, androstenedione and oestrone compared with non-consumers women(Reference Rinaldi, Peeters and Bezemer36,Reference Shafrir, Zhang and Poole37) . Another study revealed that alcohol consumption is related to change in plasma sex hormone levels in premenopausal women(Reference Sarkola, Mäkisalo and Fukunaga38). In postmenopausal women, alcohol ingestion was related to increased plasma E2 and oestrone levels(Reference Ginsburg, Mello and Mendelson39). Cigarette smoking is related to increase in 2-hydroxylation pathway of E2 and decrease in bio-availability of oestrogen(Reference Michnovicz, Hershcopf and Naganuma40). A review study proposed another mechanisms underlying the potential interaction of the smoking and oestrogen metabolites such as decrease in oestrogen activity, SHBG levels, aromatase enzyme activity, C-20, 22 desmolase enzyme levels and increase in free testosterone levels, hyperandrogenism and the hepatic metabolism of steroid(Reference Ruan and Mueck41).
NAC, compared with metformin, led to a decrease in E2 levels. However, the effects of NAC on the number of follicles, endometrial thickness, LH and FSH levels were not markedly different. Metformin, through the induction of 5' AMP-activated protein kinase and subsequently insulin sensitivity, has been widely used as a therapeutic agent in various conditions, including type 2 diabetes mellitus, PCOS and gestational diabetes(Reference Rice, Elia and Jawad42). These pathways could contribute to a synergistic effect of metformin and NAC on sex hormones profile. These factors have been ignored in the relationship between NAC and E2 levels. Therefore, a definite interpretation of more decreasing effects of NAC on E2 levels than metformin needs more studies. Nasr et al. reported that NAC supplementation increases the number of follicles in PCOS women(Reference Elgindy, El-Huseiny and Mostafa23). According to the bias assessment using the Cochrane Collaboration’s risk of bias tool, this study had a lower risk of bias; therefore, its results could be reliable. However, additional studies are needed to compare the effects of NAC with placebo on the number of follicles. El Sharkwy et al. demonstrated that NAC, in comparison with l-carnitine, led to a significant increase in FSH levels(Reference El Sharkwy and Abd El Aziz24). Due to the higher number of participants, this study was greatly weighted and influenced the overall results, so removing of mentioned study in sensitivity analysis changed the increasing effects of NAC on the FSH levels. Other mechanisms proposed for the effects of l-carnitine on FSH and LH levels could be attributed to the regulation of lipid peroxidation and activity of antioxidant enzymes(Reference Rezaei, Mardanshahi and Shafaroudi43). A comparison of two meta-analyses with the subjects of NAC and l-carnitine supplementation on inflammatory and oxidative stress biomarkers revealed that NAC had better effects than l-carnitine(Reference Faghfouri, Zarezadeh and Tavakoli-Rouzbehani6,Reference Fathizadeh, Milajerdi and Reiner44) . Similarly, our results suggested that improving the effects of NAC on FSH levels was more significant than l-carnitine. However, due to the limited number of conducted studies, more conclusions must be declared with precaution. On the other hand, the hormone status and other metabolites levels, such as serum 25(OH)D in women younger than 30 years, are lower than that in women 30 years and older(Reference Nakamura, Nashimoto and Matsuyama45). Thus, this situation also may affect the results(Reference Steiner, Herring and Kesner46).
NAC supplementation for ≥ 8 weeks led to a significant decrease in TT. In other investigated variables, extending supplementation duration was ineffective in the overall results. Regarding TT, studies with shorter duration had smaller sample sizes than studies with longer duration studies. Therefore, they might not have enough power to reach a significant result.
The risk of bias in one included study was low, in two was moderate and other included studies had a higher risk of bias. Also, publication bias could change the effects of NAC on E2 levels and endometrial thickness. As there was no unexplained heterogeneity, our results had no inconsistency. Participants of included studies in seventeen of eighteen studies had PCOS. Therefore, our results could be generalised to these patients.
Different underlying mechanisms have explained how NAC could affect reproductive biomarkers. NAC is the source of the sulfhydryl group that is essential for removing free radicals like H2O2, OH* and O2 -*(Reference Sadowska, Manuel and De Backer47). As well, NAC supplementation increased levels of GSH in individuals with low GSH levels and improved redox homoeostasis(Reference Paschalis, Theodorou and Margaritelis48). Moreover, reactive oxygen species-induced mitogen-activated protein kinase activation could be inhibited by NAC(Reference Xiong, Zhang and Zheng49). Therefore, NAC, through decreasing lipid peroxidation, could have beneficial effects on reproductive biomarkers. It must be noted that the GSH levels might be effective in the relationship between NAC and reproductive biomarkers(Reference Atkuri, Mantovani and Herzenberg50). Therefore, measuring GSH levels to determine the availability of cysteine as the limiting step must be considered in future studies. Badawy et al. reported that NAC induced ovulation in PCOS patients through increasing insulin sensitivity(Reference Badawy, State and Abdelgawad13). This was similar to the effects of metformin on PCOS.
Our systematic review and meta-analysis had some limitations that must be noted. First, only a limited number of the studies have assessed the effects of NAC on progesterone and SHBG levels. Consequently, subgroup analysis could not be performed on these biomarkers. Second, due to this cause, the comprehensive subgroup analysis based on dosage or type of control in some biomarkers was not performed. Therefore, a definite interpretation on the effects of different dosages of NAC should be considered cautiously. Third, in some cases, publication bias has changed the overall results. However, its impact was neutralised by performing trim and fill analysis. As well, the risk of bias was almost high in the included studies that might affect the quality of evidence. Therefore, future studies must focus on the proper design to diminish the possible sources of bias. As well, further studies are needed to compare the synergistic effects of NAC, metformin and l-carnitine on reproductive biomarkers in patients with PCOS. This study had some strengths too. First, to our knowledge, current study is the first comprehensive systematic review and meta-analysis addressing this issue, so far. Second, all possible subgroup and bias-controlling analyses were performed to obtain reliable results on the effects of NAC on the reproductive biomarkers.
Conclusion
The results indicated that NAC supplementation decreased TT levels and increased FSH levels. Oestrogen levels also were increased after correcting publication bias. These might contribute to a better function of the reproductive system. However, this conclusion should be with precaution as the other sex hormones and ovulation parameters were not influenced by NAC supplementation, significantly. Overall, this study supports the efficacy and favourable effects of NAC supplementation on improvement of reproductive system function.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S0007114522003270
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Baqiyatallah Hospital, for all their support and guidance during carrying out this study.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
K. P. was responsible for designing and coordinating the study. All authors were responsible for data collection, data analysis and data interpretation in the manuscript. E. E., Z. S. A., and K. P. were responsible for the statistical work and for writing the manuscript. K. P. was responsible for reviewing the manuscript. All authors read and approved the final manuscript.
The authors declare that they have no competing interests.