Breast cancer is the most common cancer among women, representing 25 % of all female cancers diagnosed in 2012 worldwide( Reference Ferlay, Soerjomataram and Dikshit1 ). In the Netherlands, the incidence is 131 cases per 100 000 women, which is the third highest incidence rate in Europe( Reference Ferlay, Steliarova-Foucher and Lortet-Tieulent2 ). However, the different patterns in breast cancer prevalence in these countries suggest that lifestyle factors may be involved. For example, substantial nutritional transitions, characterised by increased intake of animal and processed foods, have occurred in several countries which may be at least in part attributable to the concurrent rise in breast cancer( 3 ).
Several studies suggest that specific animal foods may be associated with the risk of breast cancer. For example a meta-analysis by Wu et al. ( Reference Wu, Zeng and Huang4 ) showed an association between meat intake, but no other animal foods, and breast cancer risk in USA and European populations, whereas another meta-analysis of individual cohort studies in North America and Western Europe found no relation between meat, poultry and dairy product intake and breast cancer risk, and only found a positive dose–response relationship between egg intake and breast cancer( Reference Missmer, Smith-Warner and Spiegelman5 ). The European Prospective Investigation into Cancer and Nutrition (EPIC) cohort, on the other hand, found a non-linear positive association of egg intake and breast cancer risk( Reference Pala, Krogh and Berrino6 ), whereas another study only found an association with red meat intake( Reference Farvid, Cho and Chen7 ) which was not confirmed by another meta-analysis( Reference Alexander, Morimoto and Mink8 ).
A potential mechanism for the association between animal food sources and breast cancer risk may be due to their protein content. Proteins may increase insulin-like growth factor 1 (IGF-1) levels, which may contribute to tissue growth and tumour progression when present in excess( Reference Muti, Quattrin and Grant9 , Reference Outwater, Nicholson and Barnard10 ). Also, specific fats in animal foods (i.e. saturated and polyunsaturated fat composition) influence cholesterol levels, which is a precursor for oestrogen( Reference Aune, De Stefani and Ronco11 , Reference Si, Qu and Jiang12 ), which subsequently can affect the risk of breast cancer( Reference Aune, De Stefani and Ronco11 , Reference Si, Qu and Jiang12 ). The World Cancer Research Fund and American Institute for Cancer Research (WCRF/AICR) recently concluded on the basis of a comprehensive systematic review that there is still inconsistency regarding various animal foods and breast cancer risk, which may be due to heterogeneity in terms of study population or limited adjustment for other dietary factors such as dietary fat intake( 13 ). For that reason, we aimed to investigate the association between different animal food sources and risk of postmenopausal breast cancer in a population-based cohort study, taking into account multiple dietary and lifestyle factors.
Methods
Study population and design
This study was embedded in the Rotterdam Study (RS), a population-based prospective cohort of subjects aged 45 years and over, living in Ommoord, a district of Rotterdam, the Netherlands. The RS comprises three cohorts, but in the present study we used only the first cohort (RS-I), which consists of 7983 persons aged 55 years and over, recruited between July 1989 and September 1993. RS-I is comprised of 7983 subjects, of whom 4878 were women, aged 55 years or older. Male patients (n 3105) and those without dietary data (n 1668) were excluded. Dietary data were considered missing when (i) individuals were included during the pilot phase of the study (between 1989 and 1990), (ii) individuals were institutionalised and (iii) the research dietitian considered the dietary data unreliable, for example, when subjects had difficulties with the recall of their food intake. Women with a history of breast cancer (n 1) were also excluded, leaving a final population of analysis of 3209 women, of whom 199 (6·2 %) developed breast cancer during follow-up (Fig. 1).
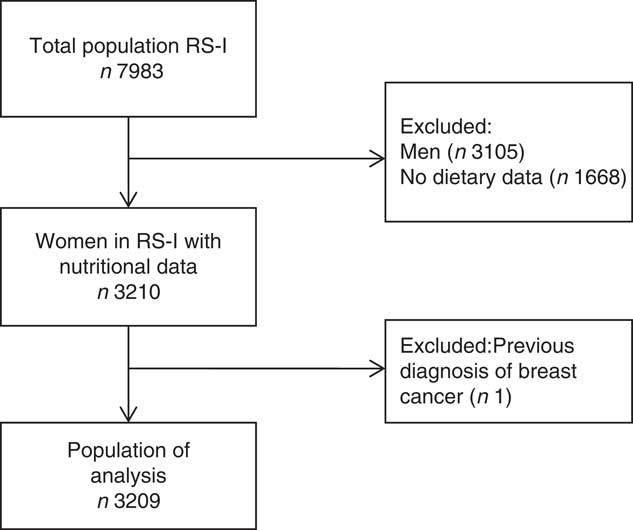
Fig. 1 Flowchart of participants included in the study. RS, Rotterdam Study.
Participants were interviewed at home by trained research nurses and were physically examined at the research centre every 3–4 years. The medical ethics committee of the Erasmus University of Rotterdam approved the study, and written informed consent was obtained from all participants( Reference Ikram, Brusselle and Murad14 ).
Dietary data collection
Dietary intake of different food groups was assessed at baseline using a two-step protocol in order to minimise loss of information. During the home interview, subjects were provided with a meal-based checklist to indicate the foods they had consumed at least twice per month in the previous year. Subsequently, a standardised dietary interview was performed at the research centre using a semi-quantitative FFQ (SFFQ) based on a validated FFQ developed for Dutch adults( Reference Goldbohm, van den Brandt and Brants15 , Reference Feunekes, Van Staveren and De Vries16 ). The FFQ consisted of 170 food items and included questions regarding the type of the food item, frequency of consumption over the last month, week or day and preparation methods. Serving sizes were expressed in natural units, household measures or grams. Intake of nutrients was calculated by the Dutch Food Composition Table( 17 ). For this study, we used the following data on the following dietary exposure variables: energy intake (kJ/d), red meat intake, including processed meat (g/d) and unprocessed meat (g/d), poultry intake (g/d), fatty (>10 g fat/100 g) and lean fish intake (0–10 g fat/100 g) (g/d) as described previously( Reference Mozaffarian, Dashti and Wojczynski18 ), egg intake (g/d) and dairy product intake, divided into milk (majority), yogurt and cheese intake (g/d) as well as dietary covariables such as total fat intake, total Fe intake (mg/d) and potential meat or dairy products replacements (i.e. intake of soya products, nuts and legumes).
Assessment of breast cancer
Data on breast cancer cases were obtained through the general practitioners data and by linkage with a local pathology laboratory in Rotterdam (PATHAN), a national database of pathology (PALGA) and a database of hospital discharges. Two research physicians independently assessed the diagnosis of breast cancer based on medical records and histopathological data. All events were coded, based on pathology, according to the International Classification of Diseases, tenth edition (ICD-10 code C50). In case of discrepancy, consensus was sought or an oncologist decided. Index date was defined as first date found on pathology records. Breast cancer cases indexed before the start of follow-up were excluded at baseline. Information on vital status of participants was obtained on a weekly basis via municipal population registries and through general practitioners’ and hospitals’ databases. All-cause mortality was defined as participants who died from any cause during the total follow-up period. Follow-up data were available until December 2010.
Covariables
During the home interview, participants were asked for information on socio-economic background and lifestyle habits, such as educational level, smoking status and alcohol intake as well as age at menopause, parity and history of breast-feeding, use of hormonal therapy and family history of breast cancer. Body weight, height (for BMI calculation) and waist circumference were measured at baseline by trained research nurses during the examination cycle at the research centre. Physical activity levels were assessed at the third examination cycle (RS-I-3) by means of an adapted version of the Zutphen Physical Activity Questionnaire( Reference Caspersen, Bloemberg and Saris19 ). Data on cholesterol concentrations (mmol/l), sex-hormone binding globulin (SHBG) (nmol/l) and oestrogen (pmol/l) serum levels were also assessed from blood drawn during the visit at the research centre.
Educational level was defined as primary education or higher. Alcohol intake (g/d) was analysed continuously. Smoking status was categorised as former smoker, never smoker and current smoker. As for BMI (kg/m2), categories were defined according to cut-offs for normal weight (18·5–24·9 kg/m2), overweight (≥25·0–29·9 kg/m2) and obesity (≥30 kg/m2)( Reference Gandini, Merzenich and Robertson20 ). Physical activity levels were analysed using metabolic equivalents of task (MET) in which we calculated MET·h/week (i.e. the sum of cycling, walking, sports, domestic work and gardening and in every type of physical activity, that is, cycling, walking, sports, domestic work, gardening). Age at menopause was analysed continuously, whereas parity was categorised as 0–2 pregnancies or three or more pregnancies. Hormonal therapy use and history of breast-feeding, when applicable, were analysed as dichotomous variables (yes v. no).
Statistical analysis
We performed crude and multivariate Cox proportional hazards regressions to analyse the association between dietary intake of animal foods and breast cancer risk. The different animal foods were used as the independent variables. The variables were energy adjusted by the residual method and analysed as continuous variables. Subsequently, they were divided into quartiles and analysed as categorical variables with the lowest quartile as reference group( Reference Willett, Howe and Kushi21 ). Breast cancer diagnosis was used as the dependent variable, and time to follow-up (in years) was used as the underlying timescale. Participants were followed until breast cancer diagnosis, death or end of follow-up. The first model was adjusted for age, whereas the multivariate models were adjusted for potential confounders. We used a change-in-estimate approach, in which we added the covariables to the first model (age-adjusted model) when the effect estimate changed by more than 10 %( Reference Mickey and Greenland22 ). The covariables tested for the multivariate model were educational level, smoking status, alcohol intake, total Fe intake, physical activity, dietary fat intake, total energy intake, age of menopause, parity, hormone use after menopause, breast-feeding history, family history of breast cancer, age at first pregnancy. Linear trends across the quartiles were evaluated by analysing the categorical variables of each food group as a continuous variable. The proportional hazard assumption was met for all models.
We performed several sensitivity analyses. First, we excluded participants with <2 years of follow-up to account for potential reverse causality. Second, to evaluate whether the results were affected by potential mediators as cholesterol and hormone levels, and body composition we additionally adjusted the multivariate model for these covariables cholesterol levels, SHBG, oestrogen levels and BMI. Also, we evaluated the presence of effect modification by BMI, total fat intake, cholesterol and oestrogen and SHBG serum levels as we hypothesised that the association between dietary intake of animal foods and breast cancer may differ by BMI and total fat intake( 23 – Reference Suzuki, Rylander-Rudqvist and Ye31 ), and sex-hormone levels( Reference Key, Appleby and Barnes32 – Reference Ewertz34 ). To evaluate the latter, the product terms of the animal foods and the potential effect modifiers were added to the multivariable model. If there was effect modification, stratified analysis was performed. Further, we examined to what extent associations could be explained by the consumption of plant-based food sources that could replace meat or dairy products such as nuts, legumes or soya by additional adjustment for these food groups. To reduce bias due to missing data, we performed multiple imputation on missing covariates (n 5 imputations; missing data ranged from 0·5 % for educational level to 40·2 % for age at first pregnancy; online Supplementary Tables S1–S3). At last, we conducted competing risk regression to evaluate potential bias from the competing risk of death for breast cancer as an outcome. Results are presented as hazard ratios (HR) and 95 % CI. P value of <0·05 was considered to be statistical significant. Statistical analyses were performed with IBM SPSS Statistics version 21 and STATA version 14.
Results
Study population
Baseline characteristics are presented in Table 1. During the median follow-up of 17 (range 0–22) years, we identified 199 cases of breast cancer (6·2 %) among 3209 women. During follow-up, 1666 (52 %) women died. The average age at breast cancer diagnosis was 66 (sd 7) years. Age-adjusted risk of breast cancer was similar for those with and without dietary data (HR: 1·01, 95 % CI 0·70, 1·45). Dairy products (milk, cheese and yogurt) was the most consumed animal food source, with an energy-adjusted mean intake of 420 (sd 230) g/d, followed by red meat and eggs (Table 2).
Table 1 Characteristics of total study population and according to animal food intake (Numbers and percentages; mean values and standard deviations; medians and ranges)
MET, metabolic equivalent of task; SHBG, sex-hormone binding globulin.
Table 2 Energy-adjusted mean intake of animal foods in g/d* (Mean values and standard deviations; medians and ranges)
* Energy adjusted according to the residual method on the basis of 2500 kcal/d (10460 kJ/d).
Association between animal food sources and breast cancer
The associations between animal food sources and breast cancer risk are presented in Table 3. After adjustment for relevant confounders (multivariate model), no significant association between red meat, poultry or total fish intake and breast cancer risk was found (Table 3). However, when lean fish was subsequently analysed, only the third quartile of intake was associated with an increased risk of breast cancer (HR for third v. lowest quartile: 1·49; 95 % CI 1·01, 2·20) but no significant trend was observed (P trend=0·08). Dairy products (i.e. cheese, milk and yogurt) did not reveal any significant associations. However, intake of milk specifically (second quartile only) was associated with an increased risk of breast cancer relative to low intake, but no significant trend was observed (HR 1·60; 95 % CI 1·07, 2·39, P trend=0·50; Table 3). However, we found a linear trend for egg consumption and breast cancer risk in which a higher intake of egg was associated with a higher risk of breast cancer, which was not altered by the adjustment for confounders (HR for third v. lowest quartile: 1·66; 95 % CI 1·09, 2·55 and HR for highest v. lowest quartile: 1·83; 95 % CI 1·20, 2·79, P trend=0·01) (Table 3).
Table 3 Association between dietary animal foods and breast cancer risk† (Hazard ratios (HR) and 95 % confidence intervals)
* P<0·05.
† Multivariate model: age-adjusted model+adjustment for physical activity (continuously in metabolic equivalent of task scores), smoking status (former, never of current smoker), history of breast cancer in first-degree relatives (yes or no), history of hormone use after menopause (yes or no), parity (0–2 pregnancies or >3 pregnancies), breast-feeding history (yes or no) and age of menopause (continuously). Additional adjustment for educational level, alcohol intake, Fe intake did not alter the HR with more than 10 %.
Sensitivity analyses
Additional sensitivity analysis showed similar effect estimates for all analyses after excluding breast cancer cases that occurred within the first 2 years of follow-up (online Supplementary Table S4). No effect modification by BMI, total fat intake, family history of breast cancer or hormone levels was found for the association between animal food intake and breast cancer (P interaction >0·10; data not shown). Also, after the additional adjustment for other food sources such as the intake of soya, nuts and legumes, higher egg intake as well as indices of body composition and cholesterol and hormone levels, increased egg intake was still associated with a significantly higher risk of breast cancer (data not shown). Results before multiple imputation are presented in online Supplementary Tables S2 and S3. Subject characteristics and HR for the association between dietary animal foods and breast cancer did not significantly differ before and after the multiple imputation procedure (online Supplementary Table S3). However, the level of significance differed for egg intake and breast cancer risk after adjustment for confounding factors (HR: 1·87; 95 % CI 1·23, 2·38 in the age-adjusted model and HR: 1·61; 95 % CI 0·57, 4·61 in the multivariate model, online Supplementary Table S3). In addition, HR were not different after competing risk regression with death as an competing event in the analysis of breast cancer (data not shown).
Discussion
This study demonstrated that high intake of eggs, but not other animal food sources, were associated with an increased breast cancer risk.
In our population, egg intake associated with an increased breast cancer risk corresponded to 13 g of eggs/d or more (i.e. more than approximately 2 eggs/week)( 35 ). These results are in line with the findings from several other studies which also found an increased risk of breast cancer with higher egg intake( Reference Missmer, Smith-Warner and Spiegelman5 , Reference Aune, De Stefani and Ronco11 , Reference Si, Qu and Jiang12 ). The EPIC cohort, which has data on 319 826 women in Europe, found a nonlinear association between dietary egg intake and breast cancer risk, with significant results in the second and fourth quintiles but not in the highest consumption group. The magnitude of this association, however, was much lower than ours (HR fifth v. first quintile: 1·08; 95 % CI 1·00, 1·17). Although the mean intake was comparable with our study (14 g/d), the HR may differ due to different cut-off points of dietary intake( Reference Pala, Krogh and Berrino6 ). A recent meta-analysis also found an increased risk, in overall and also European-specific analyses. This study found that 2–5 eggs/week (or 14–36 g/d) was associated with increased breast cancer risk in European and Asian countries as well as postmenopausal women( Reference Si, Qu and Jiang12 ). However, other studies did not confirm an association with breast cancer risk (median consumption varying from 4 to 63 g/d)( Reference Farvid, Cho and Chen7 , Reference Keum, Lee and Marchand36 ).
A specific mechanism for the association between dietary egg intake and breast cancer is still not fully understood. It may also be speculated that high cholesterol levels present in eggs may increase this risk of breast cancer, as cholesterol is a precursor for steroid hormones like oestrogen( Reference Si, Qu and Jiang12 ). In our study, however, adjustment for cholesterol levels did not alter significantly the effect estimates, nor did adjustment for hormone levels. Also, previous studies on animal foods and breast cancer risk did not identify specific differences in the association according to oestrogen receptor status( Reference Rosato, Bertuccio and Bosetti37 – Reference Guinter, Sandler and McLain39 ). This may imply that other factors may account for this positive association. Other possible pathways may be via the development of obesity and the IGF-1 system. Obesity has been linked to the risk of various cancers including postmenopausal breast cancer( Reference Argolo, Hudis and Iyengar40 ). For that reason, we conducted sensitivity analyses with additional adjustment for indices of body composition. However, results were not altered by adjustment for BMI and waist circumference. High-protein animal foods, such as red meat, dairy products and eggs, are known to elevate IGF-1 levels, a component that has also been associated with both obesity and the development of various types of cancer( Reference Muti, Quattrin and Grant9 , Reference Outwater, Nicholson and Barnard10 ). IGF-1 is thought to play a role in the pathogenesis of breast cancer due to its mitogenic, anti-apoptotic and angiogenic effects specifically on mammary cell lines( Reference Muti, Quattrin and Grant9 , Reference Outwater, Nicholson and Barnard10 ). Indeed, a meta-analysis of seventeen prospective studies showed that plasma concentrations of IGF-1 were associated with an increased breast cancer risk( Reference Key and Appleby41 ). However, since we did not find any association with other food sources, IGF-1 as the underlying biological mechanism for the association between dietary egg intake specifically and breast cancer risk needs further study.
An alternative explanation for the association between dietary eggs intake and breast cancer may be through dioxin exposure. Previous studies found a high dioxin content in eggs in the Netherlands during the time period of dietary data collection( Reference Vries, Kwakkel and Kijlstra42 ). In the 1990s, there were reports of eggs in which more than 3 pg toxic equivalents/g of fat was demonstrated, which exceeded the European Union standard( Reference Vries, Kwakkel and Kijlstra42 ). The effect of dioxins in breast cancer risk is still unclear, but animal models suggest that they disrupt the endocrine system, influencing the risk of hormone-related cancers( Reference Brody, Moysich and Humblet43 ). Although other sources of dioxins could include meat and dairy products( Reference Kogevinas44 ), high dioxin exposure in the Netherlands was mainly due to eggs during the time period of dietary data collection( Reference Vries, Kwakkel and Kijlstra42 ). So far there has been a decreasing trend in dioxin exposure in the Netherlands( Reference Freijer, Hoogerbrugge and Van Klaveren45 ); however, further validation is valuable using more recent data on time trends of dioxin exposure and breast cancer from national registries.
The lack of associations with other animal food sources are consistent with some previous studies. Wu et al. ( Reference Wu, Zeng and Huang4 ) and Farvid et al. ( Reference Farvid, Cho and Chen7 ) also found no association between the intake of poultry, fish, and milk and breast cancer risk. However, results on red meat intake and breast cancer have shown inconsistent results so far; two recent meta-analyses of red and processed meat consumption found no statistically significant positive associations with breast cancer risk( Reference Missmer, Smith-Warner and Spiegelman5 , Reference Alexander, Morimoto and Mink8 ), whereas other studies found a positive association with red as well as processed meat intake and breast cancer risk( Reference Wu, Zeng and Huang4 , Reference Farvid, Cho and Chen7 , Reference Guo, Wei and Zhan46 ). These differences in findings for red meat intake may be due to the differences in the total contribution of meat intake of a daily diet as well as differences in age groups (i.e. diet during adolescence v. middle-aged and elderly) and different categorisations of red meat intake (i.e. processed v. fresh meat). In addition, the timing of consumption might be important because several studies have found that red and processed meat intake particularly during adolescence were associated with an increased risk of breast cancer; however, this concerned mainly premenopausal breast cancer( Reference Farvid, Cho and Chen7 , Reference Farvid, Cho and Chen47 ).
The WCRF/AICR concluded in its latest report that the evidence regarding the role of meat, fish and dairy product intake in breast cancer risk as inconclusive( 23 ). This study adds to the WCRF/AICR report and provides insight on the role of egg intake and breast cancer to facilitate future dietary recommendations on the prevention of breast cancer. Moreover, several national and international dietary guidelines do not provide explicit recommendations on the amount of dietary egg consumption( Reference Kiefte-de Jong, Mathers and Franco48 ).
The strengths of this study include the length of follow-up and prospective study design. In addition, information bias by differential recall was minimised because dietary assessment was performed at the beginning of follow-up when participants were free of cancer and unaware of later research hypotheses. Also, we were able to adjust for a wide range of confounders including multiple dietary factors. Potential limitations also need to be considered. Dietary data were assessed with an SFFQ, so measurement errors may still be present. Although adjustment for total energy intake can reduce the magnitude of these errors, random error may still have diluted our results. In addition, we only had dietary assessments at baseline under the assumption that dietary habits in middle aged and elderly do not change significantly over time. There is a long latency period involved in cancer research. However, we did not have data on diet earlier in life. One study found an association between red meat intake in early adulthood and breast cancer( Reference Farvid, Cho and Chen7 ), suggesting that early life diet may be important. Our cohort included women aged 55 years or older, so we only had data of postmenopausal women; therefore, we cannot extrapolate our findings to premenopausal breast cancer( Reference Pala, Krogh and Berrino6 , Reference Farvid, Cho and Chen7 ). Another drawback could be the lack of data on history of oral contraceptive use and hormone receptor status. Several studies have shown differences in the association between other dietary factors and breast cancer risk by hormone receptor status( Reference Farvid, Cho and Chen7 , Reference Bao, Shu and Zheng38 ). Although we adjusted for oestrogen and SHBG levels in order to diminish the effect of sex hormones, results may be modified by hormone use and receptor status. In addition, physical activity levels were assessed at the third examination cycle, which may lead to residual confounding since physical activity might be associated with a decreased risk of breast cancer( Reference Wu, Zhang and Kang49 ). We used a multiple imputation procedure to account for missing data in covariates, which is considered to be the gold standard to deal with missing data in epidemiological studies. However, an important assumption for a valid multiple imputation procedure is that missing data at random (MAR; i.e. missing data can be predicted by the variables included in the imputation model). Because the MAR assumption cannot be formally tested, we aimed to include as much variables as possible to make the missing at random assumption plausible. However, there were some differences between the original data and after the multiple imputation procedure. For example, the level of significance differed for egg intake and breast cancer after adjustment for confounding factors. Because the HR were not significantly different from the original data, this difference in significance can most likely be explained by differences in the size of the population of analysis. In addition, missing data were mostly with regard to the family history of breast cancer, which reduced the population of analysis from n 3209 to n 1625, without multiple imputation. However, potential bias due to unmeasured factors affecting attrition cannot be fully ruled out. Therefore, results should still be interpreted with caution. At last, due to the small number of breast cancer cases our study design did not allow to conduct in-depth stratified analyses to explore the associations in specific risk groups (i.e. women with a family history of breast cancer).
Conclusions
In conclusion, this study found that the intake of eggs but no other animal foods were associated with a higher risk of postmenopausal breast cancer. This study provides insight into the role of egg intake and breast cancer to facilitate future dietary recommendations on the prevention of breast cancer. Since other animal food sources were not associated with breast cancer risk, further research on potential mechanisms such as related to the IGF-1 system is warranted. This may include further clarification of the role of previous exposure to dioxins or other endocrine disrupting chemicals.
Acknowledgements
The authors gratefully acknowledge the study participants, the staff from the Rotterdam Study and the participating health professionals of the Ommoord area in Rotterdam, The Netherlands.
L. H. M., O. H. F. and J. C. K.-d. J. work with ErasmusAGE, a centre for ageing research across the life course which receives funding from Nestlé Nutrition (Nestec Ltd), Metagenics Inc. and AXA. Funders were not involved in the study design; collection, analysis, and interpretation of the data; writing of the manuscript; and in the decision to submit this article for publication. The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
The authors’ contributions are as follows: J. C. K.-d. J., B. H. S., M. A. I. and O. H. F. designed the research; L. H. M. conducted the research, analysed the data, performed the statistical analysis and wrote the paper; R. R., M. M. and B. H. S. performed data collection on breast cancer; L. H. M. and J. C. K.-d. J. had primary responsibility for the final content; and all authors read and approved the final manuscript.
The authors declare that there are no conflicts of interest.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114519000072







