In humans, the critical window of brain development is between the third trimester of gestation and 2 years of age( Reference Dobbing 1 ). Intra-uterine and neonatal insults have long-term detrimental effects on neurodevelopmental outcomes( Reference Mwaniki, Atieno and Lawn 2 , Reference Laus, Vales and Costa 3 ), which are not regulated only genetically. It is known that nutrients regulate brain development during gestation and early postnatal life( Reference Kretchmer, Beard and Carlson 4 , Reference Georgieff 5 ). Therefore, early nutrition during these critical windows of rapid brain development might be essential for later cognitive functioning and behaviour. Nutritional insults and malnutrition in early periods may affect brain cell proliferation and differentiation, synaptogenesis or dendritic arborisation and myelination, processes that are in turn associated with delays in cognitive functions( Reference Laus, Vales and Costa 3 ).
There is compelling evidence relating nutrient supply and nutritional status in early life with mental performance. However, some nutrients appear to have a stronger effect on brain development during gestation and early infancy, such as protein, Fe, Zn, Se, folates( Reference Georgieff 5 ), long-chain PUFA( Reference De Souza, Fernandes and do 6 ) and vitamin D( Reference Currenti 7 ), among others.
Classical models to study the effects of nutrition on later mental performance are nutritional intervention studies in preterm infants, who are within a critical period vulnerable to suboptimal early nutrition in terms of brain development. A clinical trial performed in 360 preterm infants, who were randomised to a preterm enriched formula (higher energy, protein and fat) or a standard term formula, showed that infants who were nutrient supplemented had improved intelligence quotients at 7·5–8 years of life( Reference Lucas, Morley and Cole 8 ).
Other models relating nutrient supply and nutritional status to later cognitive function were usually observational or interventional studies on under-nourished children in developing countries. Studies providing energy and protein supplementation to under-nourished children showed benefits on their development, suggesting that this may be attributed to energy and protein supplementation rather than to micronutrients( Reference Grantham-McGregor 9 , Reference Pollitt, Saco-Pollitt and Jahari 10 ). A study conducted in Guatemala demonstrated that infants exposed to a protein–energy supplementation (during gestation and the first 2 years of life) scored significantly better in knowledge, numeracy, reading, vocabulary, time-reaction in information-processing tasks during adolescence than those who were not supplemented( Reference Pollitt, Gorman and Engle 11 ). Moreover, when these children were followed-up 20 years later, the authors found a better educational achievement among those who received protein supplementation in infancy compared with those who received energy supplementation( Reference Li, Barnhart, Stein and Martorell 12 ).
Regarding well-nourished infants, there are no data from large prospective follow-up studies on the possible effect of different levels of protein intake early in life on later neurodevelopment. In the last few years, trends on protein recommendations during infancy and childhood have tended to be lower than that in the past, as shown by a significant reduction recommended by the last WHO and the FAO Joint Report( 13 ).
The Childhood Obesity Project, a randomised clinical trial conducted in well-nourished infants from five European countries, showed that lower protein (LP) formula intake during the 1st year of life led to significant lower BMI at 2( Reference Koletzko, von Kries and Closa 14 ) and 6 years( Reference Weber, Grote and Closa-Monasterolo 15 )of age. Formulae provided to infants during the 1st year of life were both within the normal ranges recommended by the EU Directive for Infant and the Follow-on Formulae( 16 ). However, variability in normal diets among healthy infants may lead to significantly different protein intakes.
It remains to be demonstrated whether LP intakes (within the normal ranges) among healthy infants, a part of being able to reduce obesity risk, are safe in terms of mental performance achievement.
Our aim was to demonstrate that LP content in infant formulae during the 1st year of life does not affect cognition and behaviour later in childhood compared with higher protein (HP) formulae intake.
Methods
Design
This study was a European multi-centre randomised clinical trial, in which infants were randomised to be fed a HP (infant formula 2·9 g protein/418·4 kJ (100 kcal) and follow-on formula 4·4 g protein/100 ml) or LP content formula (infant formula 1·77 g protein/418·4 kJ (100 kcal) and follow-on formula 2·2 g protein/100 ml) during the 1st year of life, and were followed-up at the age of 8 years with a neuropsychological battery of tests as a part of the Nutrimenthe Project. Details about the nutritional intervention have been published elsewhere( Reference Koletzko, von Kries and Closa 14 ). An observational control group of breast-fed (BF) infants was recruited for comparison, as recommended by the European Society of Pediatric Gastroenterology Hepatology and Nutrition( Reference Aggett, Agostoni and Goulet 17 ), and were followed-up until the age of 8 years accordingly. Children were recruited by the research teams in clinics from Germany, Belgium, Italy, Poland and Spain during the 1st 8 weeks of life from October 2002 to July 2004. In brief, inclusion criteria were that infants should be born at term, should be healthy with appropriate weight and should not have disorders or medications altering growth and/or feeding. Formula-fed infants had to be exclusively formula-fed at the end of the 8th week of life. BF children had to be exclusively BF since birth (and abandonment of exclusive breast-feeding before the 3 months was a criterion to discontinue).
The growth of children was assessed until the age of 6 years( Reference Weber, Grote and Closa-Monasterolo 15 ). At 8 years of age, all the participants who had not expressed previously their willingness to not be contacted were approached by telephone to be invited for an additional visit.
Neuropsychological assessment
A neuropsychological battery of tests was carried out in children from the five European countries at the age of 8 years. Table 1 shows the tests used to assess the different domains.
Table 1 Neuropsychological battery of tests passed at 8 years of age
Psychologists from the different countries were trained and provided with Standard Operating Procedures Manuals.
The Recall of Objects Test was used to assess visual memory in short term and long term( Reference Snodgrass and Vanderwart 18 ). This test has a reliability of 0·74 from 4 to 17 years. In this test, the child was asked to look at a sheet with different pictures for 20 s. The child was then asked to recall the objects immediately (short-term memory) and after 20 min (delayed memory). After this, the child was asked to recognise the drawings in a sheet of paper (recognition). Hits, intrusions and perseverances were recorded at the different trials. Immediate visual memory score (hits 1st part–(intrusions 1st part+perseverances 1st part)) and delayed visual memory score (hits 2nd part–(intrusions 2nd part+perseverances 2nd part)) were calculated.
The Rey Auditory Verbal Learning Test( Reference Rey 19 ) was administered to assess verbal memory. To pass this test, the examiner read lists of words that the child had to remember and repeat (in the short term, long term and as recognition). Hits, intrusions and perseverances were recorded at the different trials. There was a 1st part in which learning and attention was assessed, a 2nd part in which an interference list of words was included and a 3rd and 4th part in which short-term and long-term verbal memory were assessed, respectively. Overall learning achievement, loss after interference and loss after temporal delay were calculated. Total perseverances, intrusions and interferences were summarised. Test–re-test correlation coefficients ranged from 0·36 to 0·68. The Cronbach’s α coefficient was 0·80( Reference De Sousa-Magalhães, Fernandes-Malloy-Diniz and Cavalheiro-Hamdan 20 ) The validity of this test is supported for its correlation with similar tools from 0·50 to 0·65( Reference Rey 19 ).
The Continuous Performance Test (CPT)( Reference Conners, Epstein and Angold 21 , Reference Conners 22 ) was used to assess sustained attention. To perform this task, the child was asked to press a computer key every time a yellow A appeared on the screen, but not to press the key if any other letter in any other colour appeared (during 11′ 39″. Hits, commissions and omissions were recorded at every different trial. The median test–re-test correlation of the CPT has been 0·67, suggesting a good level of reliability.
The Cancellation Test( Reference Woodcock and Muñoz-Sandoval 23 – Reference Woodcock, McGrew and Mather 25 ) was used to assess visual attention and processing speed, asking the child to mark five figures that should be equal to a model in a template that included several models. The child had 3 min to find as many equal figures as possible. Hits, commissions and omissions were recorded. The reliability of the Cancellation test for processing speed was 0·91 and for visual-spatial thinking it was 0·80( Reference McGrew and Woodcock 26 ).
The Hooper Visual Organisation Test (HVOT)( Reference Hooper 27 ) was administered to assess visual-perceptual integration. The test consisted of thirty line drawings, each showing a common object that had been cut into several pieces. The pieces were scattered on the page like parts of a puzzle. The child’s task was doing a mental puzzle, telling where the object would be if the pieces were put back together correctly. Each recognised object was a hit. The coefficient alpha for the HVOT was 0·882, and the inter-rater reliabilities ranged from 0·977 to 0·992( Reference Lopez, Lazar and Oh 28 ).
The Animals test assessed verbal fluency at the semantic level, asking the child to state as many animals’ names (hits) as possible.
The Nepsy’s Token Test( Reference Korkman, Kirk and Kemp 29 , Reference Korkman, Kirk and Kemp 30 ) consisted of giving instructions to the child to mark on a figures template in order to assess the verbal comprehension (with each correct mark considered a hit). The validity of the Nepsy’s token test has been shown by comparison with many tests such as the Wechsler Intelligence Scale for Children, fourth edition (WISC–IV; Wechsler, 2003)( Reference Korkman, Kirk and Kemp 29 , Reference Korkman, Kirk and Kemp 30 ).
The Symbol Digit Modalities Test( Reference Smith 31 ) consisted of asking the child to relate symbols with numbers following a given template with a reference key during a limited time period (90 s). Hits were recorded. We used this test to assess processing speed. This test has shown a test–re-test reliability of 0·80( Reference Smith 31 ).
The Grooved Pegboard Test( 32 ) consisted of asking the child to place pegs in holes as fast as possible. The child needed to ascertain the proper orientation of the peg to place it in the hole; therefore, this task helped determine visual-motor coordination. For each hand, (dominant/non-dominant) three scores were recorded: the total time for completing the test (s), total number of pegs dropped and the total number of pegs correctly placed in the board.
The Stroop Test( Reference Golden 33 ) was used to assess reading fluency, selective attention and impulsivity/inhibition by asking the child (1st) to read as fast as possible the name of colours that appear written in black (hits), (2nd) to state the colour of coloured crosses that were shown (hits) and (3rd) to state the name of the colour that was written but coloured in a different colour (hits). Flexibility/shifting were then estimated through an interference index. The interference measure was calculated by subtracting the average time needed to complete the 1st two subtasks from the time needed to complete the third subtask (Interference=time 3rd task–(time 1st task×time 2nd task)/(time 1st task+time 2nd task))). This test has shown reliabilities between 0·73 and 0·89( Reference Golden 33 ).
The Reversal Digits task (of Woodcook–Muñoz battery of tests)( Reference Woodcock, McGrew and Mather 25 ) was used to assess Working memory (attention+hearing short-term memory) by asking the child to repeat in inverse order the lists of numbers that the examiner called out. Every correct answer was recorded as a hit. This test has a median reliability of 0·88( Reference Woodcock, McGrew and Mather 25 ).
Reasoning was assessed using the Kaufman-ABC II test( Reference Kaufman and Kaufman 34 ), by showing the child a series of images that formed a logical linear pattern, in which a part of the image was missing. The child should select the missing part from several options. Every correct image chosen was recorded as a hit. This test has shown an internal consistency of 0·89 and a test–re-test reliability of 0·74( Reference Kaufman and Kaufman 34 ).
The Children’s Colour Trail Test( Reference Llorente, Williams and Satz 35 ) consisted of linking numbers considering its colours including interferences to assess the child’s flexibility/shifting; time taken was recorded (the faster the child was, the better the performance). Cognitive flexibility was calculated by subtracting the time to perform the 1st part from the time to perform the 2nd part of the test. The interference index was also calculated (Interference index=(time 2nd part–time 1st part)/time 1st part) (higher the interference index, lower the inhibitory control). The temporal test–re-test reliability of this test was modest (from 0·46 to 0·60). The concurrent validity from correlation with other tests ranges from 0·59 to 0·74( Reference Llorente, Williams and Satz 35 ).
The Hungry Donkey Task (HDT)( Reference Crone and van der Molen 36 ) was performed to assess the child’s decision-making abilities. This was a computer-based test in which a donkey chose from four doors, each with a trend to cost an apple or get rewarded with apples (red or green apples). The objective was to fetch the donkey the maximum number of green apples as possible. The task consisted of four parts in which hits were recorded. The total score was calculated as the sum of hits from the four parts.
Behaviour
The degree of internalising and externalising behavioural problems was assessed by administering the mothers with the Child Behaviour Checklist 4–18 (CBCL)( Reference Achenbach and Rescorla 37 , Reference Achenbach 38 ). CBCL has a good reliability with internal coefficients ranging from 0·78 to 0·97 on the Syndrome scales and 0·72 to 0·91 on the DSM-Oriented scales( Reference Achenbach and Rescorla 37 , Reference Achenbach 38 ). Z-scores were calculated using the references for societies( Reference Achenbach and Rescorla 37 ).
Perinatal characteristics
At recruitment, perinatal characteristics such as gestational age, mother’s age at child birth and delivery type were obtained from hospital records, and data regarding smoking habits (yes/no), alcohol consumption (yes/no) and stress during pregnancy (yes/no) were obtained from the mothers through a questionnaire at the time of recruitment.
Socio-demographic factors
Nationality (foreign/not foreign) and the mother’s marital status (single mother/mother married or living in partnership) were recorded through a questionnaire at recruitment. Information regarding parents’ highest educational level was collected from the participants at the time of recruitment and recorded according to the International Standard Classification of Education – ISCED-97( 39 ), and classified as low (pre-preliminary and primary level of education), medium (secondary and post-secondary level of education) and high (tertiary level of education).
Ethics
This study was carried out according to the Declaration of Helsinki( 40 ), and was approved by ethics committees of all the study centres. Parents or legal caregivers signed the written informed consents to participate in the study.
Statistics
As there were socio-cultural differences between countries, we calculated sex and country internal Z-scores for all the tests. All the results are presented as Z-scores. Descriptive results are presented as median and interquartile range; 25th, 75th percentiles.
Differences between LP and HP groups were assessed using the Student t test or the Mann–Whitney U test (as appropriate) after assessing data distribution. To compare the two randomised groups (LP and HP) with the observational group (BF), we used ANOVA or the Kruskal–Wallis test with Bonferroni post hoc comparisons (as appropriate).
We performed adjusted analyses using ANCOVA or the Mann–Whitney U test (as appropriate) with correction for multiple testing (Bonferroni post hoc comparisons) to assess differences by feeding groups. Considered confounders were sex, parents’ education level (low, medium, high), delivery type (vaginal v. caesarean section), gestational age, child’s head circumference at birth (Z-score referred to WHO standards( 41 ), calculated with WHO Anthro software for PC( 42 )) and at 8 years of age (cm), maternal smoking during pregnancy or any other time, mother’s age and marital status (single v. married) at the time of child birth and parents’ nationality (both parents foreign/not foreign).
Statistical significance was accepted at P<0·05. The data management and statistical analyses were conducted using IBM SPSS, version 20.0 (IBM Corp.).
Results
A total of 1678 infants were recruited in the five European countries (550 HP, 540 LP and 588 BF) (Fig. 1). The median age at inclusion to formula groups was 14 d (interquartile range: 3–30 d). At 12 months of age, 1099 children still remained in the study. Of the 652 participants included in the study at 8 years of age, 537 (82·4 %) (Fig. 1) agreed to be assessed with the neuropsychological battery of tests, which required approximately 2 h of participation.
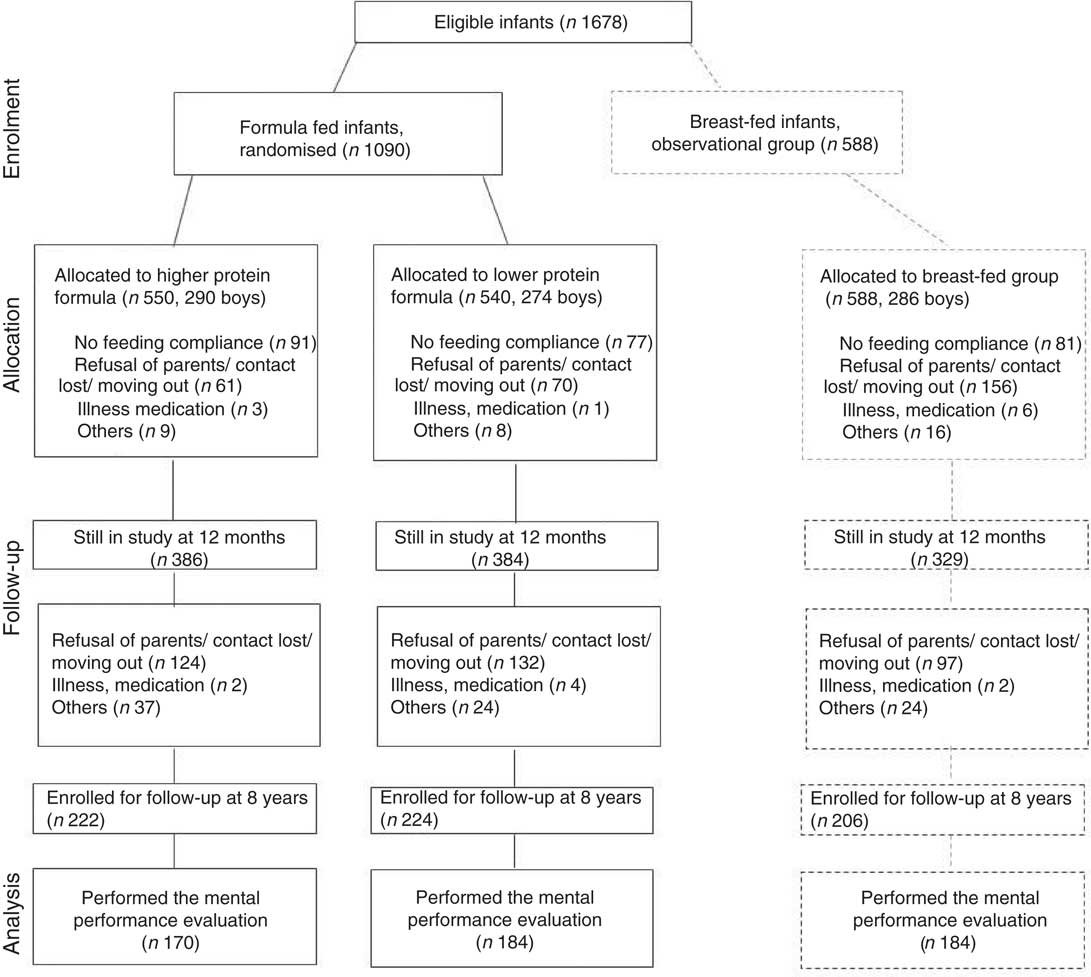
Fig. 1 Flow chart of participants from inclusion up to 8 years of age.
Children in the formula-fed groups who had withdrawn from the study or did not take part in the neuropsychological assessment at 8 years of age did not differ from the children who took part in some of the baseline characteristics such us birth weight, birth length, gestational age and maternal stress during pregnancy (data not shown).
Children who withdrew from the study had bigger head circumference at birth (34·3 (sd 1·3) v. 34·1 (sd 1·4), P=0·039) and younger mothers (29·3 (sd 5·4) v. 30·9 (sd 4·8), P<0·001) compared with children in the study at 8 years of age, but leaving the study did not interact with the study formula. Children who participated in the study were born more frequently by caesarean section (28·5 v. 19·8 %, P=0·001), had foreign parents more frequently (8·0 v. 6·7 %, P<0·001), had fewer parents with low education level (14·5 v. 26·1 %, P<0·001), had single mothers less frequently (7·7 v. 4·5 %, P=0·030), had mothers who smoked less frequently until the 12th week of gestation (24·4 v. 36·9 %, P<0·001) and beyond (21·9 v. 31·5 %, P=0·001) and had mothers who drank alcohol during pregnancy more frequently (25·4 v. 16·2 %, P<0·001).
Table 2 shows the perinatal baseline characteristics of the study sample by feeding group at 8 years of age. Children fed the LP and HP formulae had similar baseline characteristics at inclusion, as there were no differences in anthropometrical, socio-demographic characteristics, gestational age and mother’s age at child birth between them. Children fed the LP formula were born in higher proportion by caesarean section (P=0·020) and their mothers smoked more frequently (P=0·009, for tobacco before and beyond 12th week of gestation) compared with infants fed the HP formula.
Table 2 Anthropometric baseline characteristics of the children assessed with the neuropsychological battery of tests at 8 years of age (Mean values and standard deviations; frequencies and percentages)
HP, higher protein; LP, lower protein.
* P<0·05, † P<0.01, ‡ P<0.001 v. HP; a P<0.05, b P<0·001 v. LP.
BF infants significantly differed from formula-fed infants in several baseline characteristics such as gestational age, delivery type, maternal education, maternal age and maternal smoking habits (Table 2).
Figure 2 shows the main results for LP- and HP-fed children for all the assessed domains (Z-scores). There were no statistically significant differences between feeding groups in any of the assessed domains such as visual memory (neither immediate nor delayed), verbal memory (both in the short and the long term as well as immediate and delayed free recall), visual attention, sustained attention, visual-perceptual integration, processing speed, visual-motor coordination, verbal comprehension, verbal fluency, impulsivity/inhibition, selective attention, flexibility/shifting, working memory, reasoning, selective and focused attention, visual-spatial skills, decision making and any of the behaviour scales assessed with CBCL (internalising problems, externalising problems or total problems).
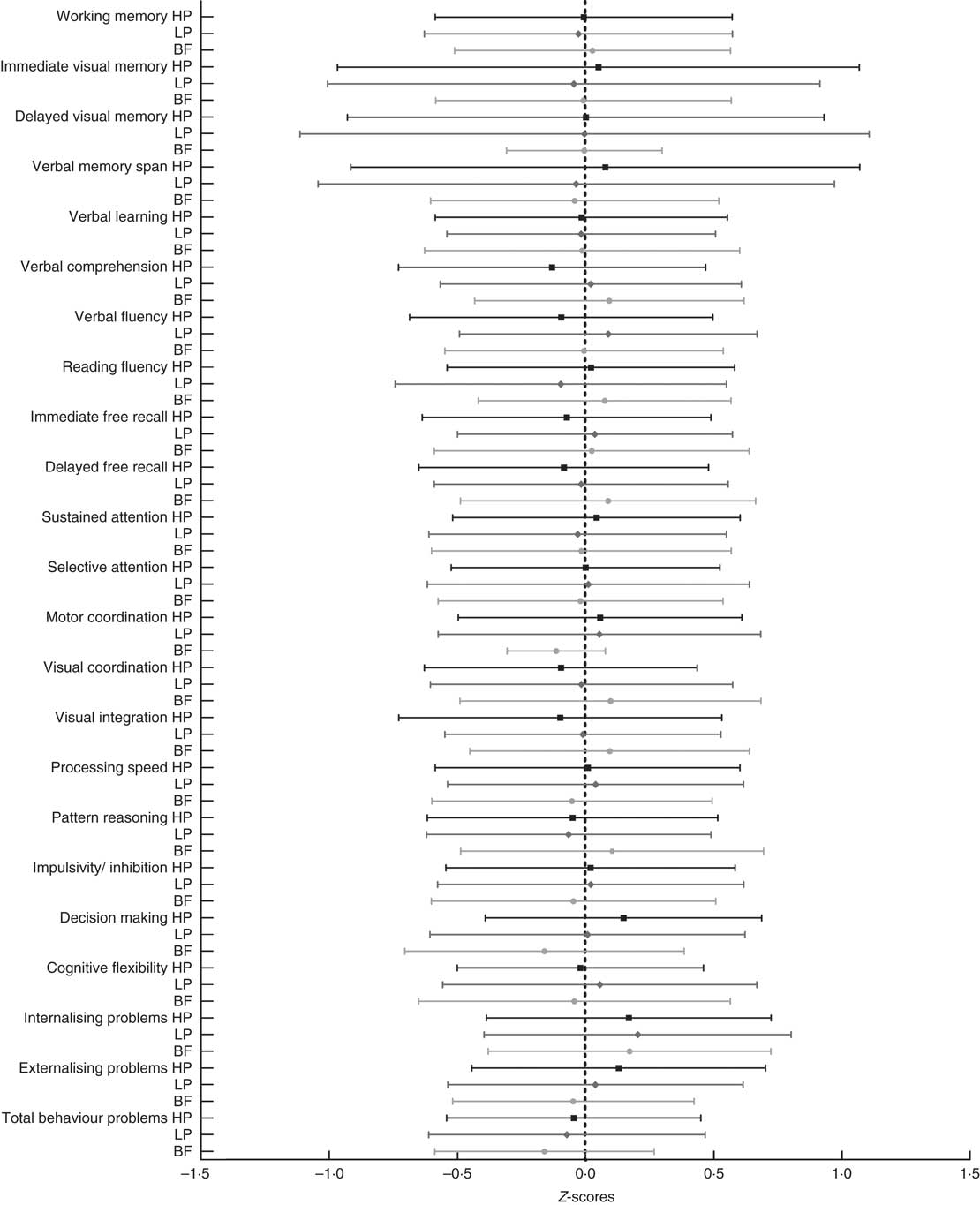
Fig. 2 Neuropsychological assessment results of children fed the lower and the higher protein formulae and breast-fed (mean (2 sd)). Effect size estimates are reported as online Supplementary material. BF, breast-fed group; HP, higher protein formula group; LP, lower protein formula group; attention; there were no differences between feeding groups in any of the assessed domains in adjusted models.
We performed adjusted analyses, considering factors that could influence neurodevelopment, such as parental education level and nationality, mother’s age and marital status, maternal smoking, child’s gestational age at birth, delivery type and head circumference at birth and at 8 years of age. These adjusted analyses confirmed no differences in any of the neuropsychological domains and behaviour between 8-year-old children fed the higher or the LP formula during the 1st year of life.
Unadjusted analyses comparing children who had been BF for at least 3 months showed similar behaviour and performance in all the domains compared with the HP and LP children (data not shown), except for the HDT (decision making), which was worse in the BF group (0·123 (95 % CI –0·839, 0·512)) than in the HP group (0·320 (95 % CI –0·308, 0·621)) (P=0·048). Adjusted analyses including the confounders mentioned above discarded any significant difference.
Discussion
This study aimed to assess the effect of feeding healthy, term infants with different amounts of protein (within the accepted range) during the 1st year of life (a critical period for brain growth and development) on mental performance later in life (at 8 years of age). To pose this question, we depended on the existing literature showing improved mental performance among preterm and under-nourished children who had been protein supplemented. The importance of such studies lies on the recent trends towards LP intake recommendations( 13 ) – for example, to prevent obesity risk. In this context, it was demonstrated that LP content in infant formulae within the normal ranges( 16 ) reduced the later obesity risk (by achieving significant lower BMI at 2 years), but did not have any negative effect on length( Reference Koletzko, von Kries and Closa 14 ). In a scenario where reduced protein intake is recommended, and this reduction seems to have preventive effects on obesity but not deleterious effects on growth, it remains a necessity to carry out a safety analysis confirming the similar neurodevelopment in childhood of those who have been fed a LP formula in early life. To test this hypothesis, we selected an extensive neuropsychological battery of tests for different domains and functions rather than a test assessing overall ability (i.e. intelligence quotient). In nutrition studies, one particular domain may be affected differently than others at different ages, and an overall ability test may not detect these differential patterns( Reference Schmitt, Benton and Kallus 43 , Reference Isaacs and Oates 44 ).
The results from this randomised clinical trial show no significant differences between 8-year-old children who had been fed the lower and the HP content formula during the 1st year of life in memory (verbal and visual), attention (spatial, focused and sustained), perception, language (fluency and comprehension), processing speed, motor coordination and executive functions (shifting/flexibility), inhibition/impulsivity, working memory, reasoning, selective and focused attention, visual-spatial skills or decision making, confirming the safety of the LP content formula.
Previous studies reporting different mental performances in children fed HP intakes( Reference Laus, Vales and Costa 3 , Reference Lucas, Morley and Cole 8 , Reference Grantham-McGregor 9 , Reference Pollitt, Gorman and Engle 11 , Reference Li, Barnhart, Stein and Martorell 12 ) had been undertaken in special populations with special needs, but not in in-term, well-nourished children.
We did not find any difference in mental performance between the formula-fed groups and the BF group. Taking into account that BF children are considered as a gold standard of neurodevelopment, these results may indicate that lowering or increasing protein intake in healthy well-nourished infants during the 1st year of life may not produce any deleterious effect on later mental performance.
There is a large number of publications relating breast-feeding and cognitive development; however, such an association is weaker after adjusting for confounders such as maternal intelligence quotient( Reference Nyaradi, Li, Hickling and Foster 45 ). We hypothesise that our results are not fully consistent with some previously published because the heterogeneous duration of breast-feeding in our study sample, which could be no longer than 3 months. This issue may be of importance, as it has demonstrated a duration-dependent effect on brain structure development( Reference Isaacs, Gadian, Sabatini, Chong, Quinn and Fischl 46 , Reference Kafouri, Kramer, Leonard and Perron 47 ).
A limitation of our study might be the high attrition rate up to the age of 8 years, and the differences found between feeding groups in baseline characteristics (that could be modulators of mental performance). However, we performed covariate analyses including all the possible modulators (such as education level, delivery type or smoking during pregnancy) to adjust the possible effect of feeding mode by these factors and we observed the same results: no effect of protein intake on later cognition and behaviour.
The main strengths of our study are the randomised clinical trial design, the large multi-European country sample and the extensive neuropsychological battery of tests used to assess different domains and functions.
In summary, herewith we report on the safety of LP content in infant formulae (closer to the content of human milk) according to long-term mental performance.
Acknowledgements
The authors gratefully acknowledge participants for their enthusiastic support to the study, Cristina Campoy for her efforts to coordinate the Nutrimenthe Project, Miguel Pérez-Garcia (UGR) for the design of the neuropsychological battery of tests and advice with its use and Ainara Blanco (URV) for her contribution to the fieldwork.
The studies reported here have been carried out with partial financial support from the Commission of the European Communities, specific RTD Programme ‘Quality of Life and Management of Living Resources’, within the 5th Framework Programme, research grants no. QLRT–2001–00389 and QLK1-CT-2002-30582, and the 7th Framework Programme (FP7/2008-2013), under grant agreement nº 212652 (NUTRIMENTHE Project ‘The Effect of Diet on the Mental Performance of Children’, the contract FP7-289346-EARLY NUTRITION and the European Research Council Advanced Grant ERC-2012-AdG – no. 322605 META-GROWTH. This manuscript does not necessarily reflect the views of the Commission and in no way anticipates the future policy in this area. The participating company had no decisive role in the conduct and analysis of the study. The formula for the study was produced by Bledina (Villefranche-sur-Saône Cédex, France, part of Danone Baby Nutrition), who operated as a partner of this EU project and received a grant from the EU Commission for this task. No funding bodies had any role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
The authors’ responsibilities were as follows: J. E. and V. L. contributed equally as first authors of the final version; R.C.-M., J. E., B. K., E. R. and D. G. conceived and designed the research; V. L., E. V., K. S., N. F. and G. B. acquired data; M. W. and V. G. managed data and advised the statistical analyses; V. L. performed the statistical analyses and drafted the article; and F. C. and J. E. revised the article for important intellectual content; all the authors read and gave their final approval of the version to be published.
There are no conflicts of interest.
This paper was published as a supplement in the British Journal of Nutrition, the publication of which was supported by the Nutrimenthe Consortium. The paper has undergone the standard journal formal review.
Supplementary Material
For supplementary material/s referred to in this article, please visit http://dx.doi.org/10.1017/S0007114515000768
Appendix: European Childhood Obesity Project Group
Beyer J., Fritsch M., Grote V., Haile G., Handel U., Hannibal I., Koletzko B., Kreichauf S., Pawellek I., Schiess S., Verwied-Jorky S., von Kries R., Weber M. (Children’s University Hospital, University of Munich Medical Centre, Munich, Germany), Dobrzańska A., Gruszfeld D., Janas R., Wierzbicka A., Socha P., Stolarczyk A., Socha J., (Children’s Memorial Health Institute, Warsaw, Poland), Carlier C., Dain E., Goyens P., Van Hees J. N., Hoyos J., Langhendries J. P., Martin F., Poncelet P., Xhonneux A., (ULB Bruxelles and CHC St Vincent Liege), Perrin, E. (Danone Research Centre for Specialised Nutrition, Schiphol, The Netherlands), Agostoni C., Giovannini M., Re Dionigi A., Riva E., Scaglioni S., Vecchi F., Verducci E. (University of Milan), Closa-Monasterolo R., Escribano J., Blanco A., Canals F., Cardona M., Ferré N., Gispert-Llauradó M., Luque V., Mendez-Riera G., Rubio-Torrents M. C., Zaragoza-Jordana M. (URV).







