Introduction
Out-of-hospital cardiac arrest (OHCA) remains a significant cause of death worldwide.1 In Canada, some 40,000 OHCAs occur each year—a figure that equates to approximately one every 13 minutes. 2 Unfortunately, despite advances in medical treatment, overall survival rates of OHCA remain low at 8%–11%.Reference Berdowski, Berg and Tijssen 1 Early bystander cardiopulmonary resuscitation (CPR) and defibrillation are known to be the two most important links in the chain of survival from OHCAReference Hubble, Bachman and Price 3 , Reference Dias, Brown and Saini 4 ; together, they have been shown to increase the likelihood of survival by 75% or more.Reference Weisfeldt, Everson-Stewart and Sitlani 5 However, despite a long-standing recognition of this, bystander CPR rates rarely exceed 30% and have remained consistently low.Reference Nichol, Thomas and Callaway 6 - Reference Vaillancourt, Grimshaw and Brehaut 9 In particular, bystander CPR rates are considerably lower in most Canadian communities when compared to analogous international locations.Reference Vaillancourt, Grimshaw and Brehaut 9 Although rates of bystander CPR are well documented, the reasons that many bystanders are reluctant to perform CPR remain poorly understood.
Through various partnerships and collaborations, both local and nationwide, the resuscitation science community has put forth a strong effort to enhance bystander CPR rates over the past decade. Popular strategies include the integration of effective dispatch-assisted telephone CPR instructions,Reference Vaillancourt, Verma and Trickett 10 - Reference Mirza, Brown and Saini 13 the implementation of CPR education in schools,Reference Cave, Aufderheide and Beeson 14 the organization of mass CPR training events,Reference Fong, Anantharaman and Lim 15 - Reference Selby, Kautz and Moore 17 targeted CPR training for family members of individuals with known cardiovascular disease,Reference Chu, May and Clark 18 , Reference Lie and Richardson 19 and, recently, the promotion of a simplified chest-compression-only (CCO) CPR technique for bystanders.Reference Bhanji, Mancini and Sinz 20 , Reference Blewer, Leary and Esposito 21 However, these efforts have largely been unsuccessful, in that bystander CPR rates in OHCA remain unchanged.Reference Vaillancourt and Stiell 22 , Reference Vaillancourt, Stiell and Wells 23 Recently, international evidence-based guidelines have endorsed a simplified CCO approach for CPR.Reference Bhanji, Mancini and Sinz 20 , Reference Blewer, Leary and Esposito 21 The CCO-CPR approach emphasizes the importance of high-quality chest compressions and removes the requirement of mouth-to-mouth (MTM) ventilation. Studies have shown that CCO-CPR is associated with similar outcomes in adult OHCA when compared to traditional CPR.Reference Omi, Taniguchi and Kaburaki 24 - Reference Bobrow, Spaite and Berg 26 This technique is currently being promoted internationally, with the goal of increasing bystander CPR rates.Reference Sayre, Berg and Cave 25
While several authors have published research describing perspectives from other countries,Reference Hubble, Bachman and Price 3 , Reference Donohoe, Haefeli and Moore 27 - Reference Jelinek, Gennat and Celenza 29 no known studies to date have examined the Canadian public perspective on cardiac arrest and bystander CPR. In particular, no published research exists on the influence of the new resuscitation guidelines on public perspectives toward resuscitation. As such, we sought to investigate Canadian knowledge, perceptions and attitudes toward OHCA and bystander CPR, and determine whether Canadians are more willing to perform the newly endorsed CCO-CPRReference Travers, Rea and Bobrow 30 compared to traditional CPR. Our specific objectives were to 1) determine whether the Canadian general public are more willing to perform CCO-CPR compared to traditional CPR; 2) characterize public knowledge of OHCA; and 3) identify barriers and facilitators to bystander CPR.
Methods
Survey design
A 32-item, online survey instrument was developed and administered according to the Tailored Design Method proposed by Dillman et al.Reference Dillman, Smyth and Christian 31 The survey was developed based on existing literature, expert consultation, and previously documented scenario-based surveys.Reference Coons and Guy 8 , Reference Taniguchi, Sato and Fujita 28 , Reference Axelsson, Thoren and Holmberg 32 - Reference Parnell, Pearson and Galletly 35 Interview data from an exploratory, in-depth qualitative study previously conducted by our research team were used to identify subtopics of particular interest.Reference Cheskes 36 - Reference Green and Thorogood 39 This ensured that the survey tool was robust and designed to fulfill the specific study objectives.
The survey and description of instruction are included in the Appendix (see supplementary material). The first section contained three screening questions to capture data on age, gender, and province of completion. The second section was designed to capture data on past CPR training and to assess participant knowledge of cardiac arrest, CPR, and automatic external defibrillators (AEDs). Questions regarding past exposure to cardiac arrest and performance of CPR in a real-world situation were also included. Determining knowledge of AEDs and willingness to use them in OHCA were not part of the initial objectives for this project. However, after exploring the topic of AEDs in detail throughout the qualitative interviews that informed this study, questions on AEDs were added to this survey. The third section involved scenario-based questions whereby participants were requested to visualize themselves as the witness of an OHCA and respond accordingly. For any given respondent, the order of appearance for two sets of scenarios (2005 v. 2010 instructions) was randomly allocated. The fourth, and final, section of the survey collected additional demographic data (marital status, offspring, education level, ethnicity, and so forth) to allow the evaluation of population representation.
Prior to administration of the survey, a pilot test of the online tool was conducted with a sample of 35 respondents. Upon completing the survey, test respondents were given the opportunity to provide feedback on clarity, brevity, wording of questions, and general concerns and comments in an open-ended fashion. Pilot test data were examined for quality and completeness. Feedback was largely positive in nature, and no suggestions were made regarding improving the clarity of the questionnaire.
This study was approved by both the St. Michael’s Hospital and the University of Toronto Research Ethics Boards.
Study setting and population
The survey was conducted with a representative sample of adults living in Canada. An external marketing company, Canadian Viewpoint, 40 provided nation-wide sampling and recruitment using their existing public research panels. Canadian Viewpoint has a well-established, representative Canadian consumer research panel. Members of the Canadian general public had previously opted to be a part of this research panel, provided their personal contact information to the company, and indicated a willingness to receive survey invitations by email. To be eligible for inclusion, potential participants had to be 18 years of age or older, speak English, and be registered to the Canadian Viewpoint 40 research panel. The three Canadian territories were excluded because their combined population is extremely small relative to Canada as a whole, and, thus, their proportional representation in the survey would be negligible. A primary language other than English was also excluded, because the research team lacked translation abilities.
The sample size requirement was estimated to be 400 participants, based upon the total population of the Canadian provinces and a desired 95% confidence interval (CI) defined a priori. The sample size was selected using a table of population-based estimations for survey responses to achieve a 5% margin of error.Reference Dillman, Smyth and Christian 31 The sample size required for +/- 5% sampling error in a population of 1,000,000 or greater with an estimated 50/50 split of responses is 384. According to Dillman et al., among large populations, there is virtually no difference in the completed sample size required for a given level of precision.Reference Dillman, Smyth and Christian 31 We rounded our sample size up to 400 to ensure that we achieved the target number of responses and sampled five regions: British Columbia, the Prairies, Ontario, Quebec, and the Maritimes. Each of these regions was assigned a quota for the survey sample that was representative of its proportion of the total population reported in the most recent Canadian census. 41
The survey was distributed over a 1-week window. Canadian Viewpoint sent reminder emails to nonresponders at 48 hours after the initial contact in an attempt to maximize the response rate. Participants did not receive any compensation for completing the survey.
Data analysis
Descriptive statistics were used to characterize the study sample and distribution of responses.Reference Dillman, Smyth and Christian 31 Open-ended questions were analysed qualitatively using a broad coding framework.Reference Braun and Clarke 42 The chi-square test, t-test, and multivariable logistic regression analyses were conducted as required to assess any shifts in intent and reported willingness to provide bystander CPR, based on the change from traditional to CCO. Definite willingness (defined as Yes responses) was coded as Yes, and unsure or unwilling responses (defined as Maybe or No responses) were coded as No. Each participant was thus classified as either a Yes or a No for both 2005 and 2010 CPR guidelines. Four groups of individuals within the sample were established for the analysis. The group labeled Y05/Y10 responded Yes to performing both types of CPR. The group labeled N05/N10 responded No to performing both types of CPR. The group labeled Y05/N10 responded Yes to traditional CPR and No to CCO-CPR, and the group labeled N05/Y10 responded the reverse. To evaluate reported changes in willingness based on the guidelines, groups 2 (N05/N10) and 3 (N05/Y10) were compared. Based on the literature and exploratory qualitative data published elsewhere, seven variables with the potential to influence intention to provide CPR were defined a priori and examinedReference Sasson, Meischke and Abella 43 : gender, age, marital status, children, education, immigration status, and prior CPR training. McNemar’s test was used for the analysis of dependent categorical variables in the scenario situations. Analyses were carried out using SAS Version 9.3 (SAS Institute, Cary, NC), and p values of 0.05 or less were considered statistically significant.
Results
We received 428 completed surveys for analysis; 274 (64.0%) of respondents had received some type of CPR training. The demographics of the study participants are provided in Tables 1 and 2 and comparatively listed with results from the 2006 Canadian census to allow an assessment of representativeness.
Table 1 Comparative characteristics of participants and the Canada 2006 Census

* Censored (n≤5).
† Variable not captured by the census.
NA=not available.
Table 2 Age and immigrant status of participants

* One missing value.
Max=maximum; Min=minimum; SD=standard deviation.
Willingness to perform CPR
The results suggest that shifts in attitude exist regarding the 2005 and 2010 guidelines. Figures 1 and 2 summarize the distribution of respondents into the combined 2005/2010 willingness groups. Table 3 provides results of a comparative analysis of N05/N10 and N05/Y10 groups, undertaken to allow an assessment of shifts with the intention to provide CPR based on changes in the guidelines. The distribution of gender between these two groups was significantly different (p=0.0015). Among participants who did not express a willingness to perform CPR according to the 2005 guidelines, women were more likely to indicate a willingness to perform CPR when MTM ventilation was removed (odds ratio: 2.3, 95% CI [1.4, 3.8]). After adjustments for the other variables of interest, female gender was found to be the only factor significantly associated with increased willingness to perform bystander CPR based on the change in the guidelines.

Figure 1 Distribution of respondents by categorical variable into combined 2005/2010 willingness groups.

Figure 2 Age of participants categorized by combined 2005/2010 willingness group.
Table 3 Comparative analysis of N05/N10 and N05/Y10 groups
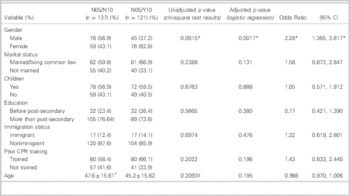
* Significant findings.
† Reported as mean±standard deviation.
‡ Two sample t-test.
CI=confidence interval.
When the OHCA victim was unknown, for the sample as a whole, the proportion of respondents willing to provide CCO-CPR was significantly greater than the proportion of respondents willing to perform traditional CPR with MTM ventilations (61.5% v. 39.7%, p<0.001). In analysing the different scenarios where the victim was identified, the proportion of respondents willing to perform CCO-CPR was significantly greater than the proportion willing to provide traditional CPR in two cases: stranger (55.1% v. 38.8%, p<0.001) and unkempt/homeless individual (47.9% v. 28.5%, p<0.001). Statistically significant differences were not found in the family, friend, and child scenarios.
Knowledge and understanding
When asked to describe a cardiac arrest in their own words, 41.4% of participants indicated that it means the heart has stopped beating. The next most common answer was a heart attack, reported by 20.8% of individuals. Symptoms of cardiac arrest cited by participants are provided in Figure 3. The three most frequently cited symptoms were chest pain, identified by 244 participants (57.0%), followed by difficulty breathing/shortness of breath (239 participants, 55.8%) and other pain (including general pain, left and/or right arm pain, shoulder, jaw, back or neck pain), identified by 159 participants (37.2%).

Figure 3 Percentage of participants citing various signs and symptoms of cardiac arrest.
A total of 400 participants (93.5%) had previously heard of CPR. When asked to list as many steps in performing CPR as possible, airway, breathing, and circulation or some variation of this sequence was noted by 37.6% of participants. Chest compressions and rescue breathing were noted by 22.2%, and only 14% indicated CCO-CPR, as is recommended in the 2010 guidelines. Overall, 24 different chest compression-ventilation ratios were reported. Participant’s perceptions of OHCA survival rates ranged from 50% survival (21%) to 0% survival (1.4%). Only 7% participants endorsed 10%, which is the currently reported rate of cardiac arrest survival.Reference Nichol, Thomas and Callaway 6 , 44
Barriers and facilitators to performing CPR
The most commonly reported rationale for providing CPR was that the respondent felt a duty or responsibility to help, and would act across all ten scenarios. The sole exception was performing traditional CPR on an unkempt individual; for 40.2% of individuals, participants feared doing MTM ventilations and putting themselves at risk for disease or infection, whereas 23.6% of respondents reported similar fears in the case of a stranger. Barriers, such as lack of knowledge/confidence in CPR skills, fear of litigation, and “depends on who else was there to help,” were reported more frequently in the case of the stranger and unkempt individuals.
Discussion
This is the first study to explore the knowledge and willingness to engage in resuscitative efforts in OHCA among members of the general public in Canada. We found that Canadians express a greater willingness to provide CCO-CPR compared to traditional CPR with MTM ventilations; however, our results suggest that significant gaps exist in lay public knowledge with respect to OHCA that may warrant further attention.
The significance of early and effective bystander action has been recognized as the sentinel predictor of survival from OHCA. However, this has not translated well into action at the point of care; bystander CPR rates in Canada remain low, rarely exceeding 30%.Reference Vaillancourt, Grimshaw and Brehaut 9 While other international studies from the United States,Reference Hubble, Bachman and Price 3 , Reference Coons and Guy 8 Europe,Reference Axelsson, Herlitz and Fridlund 7 Asia,Reference Taniguchi, Sato and Fujita 28 Australia,Reference Jelinek, Gennat and Celenza 29 , Reference Dwyer 45 and New ZealandReference Parnell and Larsen 46 have evaluated attitudes, perceptions, and understanding of CPR, our results provide important insights into Canadian perspectives on cardiac arrest and resuscitation. It is also the first study to examine the influence of the new 2010 CCO guidelines on bystander willingness to do CPR.
Significant gaps in knowledge were found in several domains. Participants were overly optimistic about survival from OHCA, with approximately half indicating a survival rate of 50% or higher. In 2006, Donohoe et al. reported a similarly high perception of survival rate, with 65% of respondents believing that at least half of OHCA patients survive.Reference Donohoe, Haefeli and Moore 27 Unrealistic assumptions about survival from OHCA may illustrate a lack of awareness amongst the general public.
Our findings suggest that the ability of the Canadian general public to appreciate when a person has suffered a cardiac arrest is poor. Confusion between the terms heart attack and cardiac arrest has been found elsewhere.Reference Donohoe, Haefeli and Moore 27 , Reference Larsen, Pearson and Galletly 47 Arrest identification is the first step in initiating CPR, and lack of recognition may be a key to the low response rate by bystanders. Identification algorithms have been simplified (e.g., removal of pulse check, recognition of agonal breathing),Reference Berg, Hemphill and Abella 48 and other groups have developed effective strategies to help lay rescuers identify myocardial infarction.Reference Alberts, Perry and Dawson 49 - Reference Bell, Lommel and Fischer 52 It is possible that increasing awareness of these tools would help with the early recognition of OHCA.
Although many participants noted that CPR comprises airway, breathing, circulation, their responses demonstrated confusion in recalling the order. Despite the fact that CCO-CPR has been endorsed since 2008,Reference Sayre, Berg and Cave 25 our data suggest that this is not widely recognized by Canadians. In a 2009 study in Arizona, Coons et al. found similarly poor awareness surrounding CCO-CPR; just over a third of respondents in his study had previously heard of it through print and broadcast media.Reference Coons and Guy 8 Our results are consistent with and provide further support to the existing body of international literature, indicating an increased willingness to perform CPR if MTM ventilations are not required.Reference Hubble, Bachman and Price 3 , Reference Donohoe, Haefeli and Moore 27 , Reference Jelinek, Gennat and Celenza 29 , Reference Kanstad, Nilsen and Fredriksen 33 , Reference Cho, Sohn and Kang 53 , Reference Shibata, Taniguchi and Yoshida 54 Community-wide CPR education initiatives should be promoting the CCO-CPR technique more effectively.
Previous research has found that 67%–80% of respondents indicate a lack of knowledge and/or confidence in skills as a significant barrier.Reference Taniguchi, Sato and Fujita 28 , Reference Kanstad, Nilsen and Fredriksen 33 , Reference Shibata, Taniguchi and Yoshida 54 Fear of litigation was inconsistently reported, with some studies identifying it as a key issueReference Hubble, Bachman and Price 3 , Reference Coons and Guy 8 and others as a very minor issue.Reference Johnston, Clark and Dingle 55 In our study, only 6%–12% of participants cited a lack of knowledge and/or confidence in skills as a barrier, and fear of litigation was not prevalent in any scenario except with a stranger. This discrepancy may be due to the differences in legislation (such as Good Samaritan protection laws) and the litigious culture of other countries.
Our study was also designed to look more closely at the public perception of barriers and facilitators to the performance of bystander CPR, and thus provides important insight into key issues, which may be very informative for the design of future education and knowledge translation strategies. Interestingly, underlying humanitarian and altruistic values appeared to play a key role in participants’ decision-making processes, with many citing a responsibility or duty to help any person in need. In an interview study carried out in 2000 of volunteer bystanders, Axelsson et al. noted that humanitarian values, expressed as a wish to save a life or the wish to help another person, constituted the foundation of the bystander’s actions.Reference Axelsson, Herlitz and Fridlund 7 Our results suggest that this concept similarly underscores much of Canadians’ reported willingness to perform bystander CPR. Moreover, our logistic regression suggests that females are significantly more likely to increase their willingness based on the shift in the guidelines compared to males. In concert, these two findings suggest that Canadian CPR training initiatives should continue to promote a simpler, CCO technique, leverage the influence of humanitarian values, and perhaps consider gender differences in both the development and delivery.
Our results provide important insights that could help inform interventions to improve bystander CPR rates; however, it is not without limitations. First, a larger sample size would have been required to compare responses by region. Second, we sampled the population using online panels of individuals who had consented and registered with a survey company. This format offered a significant advantage in terms of the size and range of respondents sampled; however, Web-based surveys have inherent selection bias in that specific groups in the populations may be under-represented due to less Internet access. Furthermore, recruitment of participants tends to be based on self-selection. Both under-coverage and self-selection may lead to biased estimates,Reference Bethlehem 56 although the direction and magnitude are difficult to estimate given the increasingly wide availability of the Internet. Despite the potential bias, we feel that this was the most feasible approach for achieving a larger sample of members of the Canadian general public. We were not able to offer the survey in other languages due to limitations in our ability to analyse non-English narrative responses; however, given that the 2011 census indicated that 75% of the Canadian population reported English as their first language and 63.5% of the population whose mother tongue was neither English nor French reported speaking English at home, 57 we feel that this still can be viewed as a nationally representative survey. Finally, participants were asked to report their behavioural intentions in hypothetical scenarios related to bystander CPR. Although intentions are a predictor of actual behaviour, it is unclear whether reported intentions would be completely concordant with actual behaviour in real-life OHCA situations.Reference Ajzen, Brown and Carvajal 58 , Reference Ajzen and Fishbein 59
Conclusion
Our findings provide important insight into the Canadian perspective on cardiac arrest and resuscitation that has not existed previously. This research revealed that Canadians are more willing to provide CCO-CPR. Of equal significance, this research revealed serious and fundamental gaps in knowledge about CPR on the part of the lay people that may contribute to bystander inaction at the scene of a cardiac arrest. Barriers and facilitators included fear of litigation and lack of skill confidence. Future work in this area should apply this information to tailor and redesign future educational initiatives and strategies.
Financial support: This project was funded by the University of Toronto’s Department of Emergency Medicine, the Heart and Stroke Foundation of Canada (and the Canadian Association of Emergency Physicians.
Competing interests: The National Institutes of Health (NIH) and the Resuscitation Outcomes Consortium supported this research through its career development awards. This research was also supported by the American Heart Association and Heart and Stroke Foundation of Canada through grants.
Supplementary Material
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/cem.2015.113








