INTRODUCTION
Ischemic heart disease (IHD) was the leading cause of death globally in 2012, with an increasing trend over the past decade. In 2012 alone, IHD claimed 7.4 million deaths, accounting for 13.2% of global deaths. 1 Large scale registries investigating acute myocardial infarction (AMI), such as the National Registry of Myocardial Infarction and the National Cardiovascular Data Registry in the United States, the Vienna ST segment elevation myocardial infarction (STEMI) network and the Belgian STEMI registry in Europe, have been established in recent years to improve patient outcomes from AMI. Similarly, in Singapore, the Singapore Myocardial Infarction Registry (SMIR) was established in 2007 to understand AMI trends. IHD is ranked third in the principal causes of death in Singapore, according to the Ministry of Health in 2013. 2 The average number of AMI episodes in Singapore between 2007 and 2013 was 7829 per year, of which approximately 30% were STEMI cases. 3
Early reperfusion therapy in the treatment of STEMI patients can improve outcomes. To shorten the door to reperfusion time, measures such as prehospital electrocardiogram (ECG) transmission in the field to the emergency departments (EDs) were adopted nationwide in Singapore in 2008.Reference Ong, Wong and Seet 4 Ambulance protocols indicate that ECGs are to be performed on patients presenting with chest pain, breathlessness, and diaphoresis. Other atypical symptoms that ambulance crews are to observe include jaw pain, shoulder pain, and so forth. However, there exists a subgroup of STEMI patients without complaints of any form of pain.
A search on PubMed shows a paucity of literature on painless STEMI. A study by Cho et al. of the Korea Acute Myocardial Infarction Registry data showed that painless STEMI was associated with higher rates of in-hospital mortality and 1-year major adverse cardiac events.Reference Cho, Jeong and Ahn 5 In a study conducted in the United States, Coronado et al. found that AMI patients who presented to the ED without pain had a lower rate of admission to the critical care unit than similar patients who presented with pain; a higher mortality rate was also seen in patients with painless acute ischemia.Reference Coronado, Pope and Griffith 6 Silent myocardial infarction is associated with poor prognosis, but little is known about its effect on treatment delays.Reference Raby, Goldman and Cook 7
Hence, we aimed to characterize STEMI patients presenting to EDs in Singapore without complaints of pain, and examine its association with delays in treatment and mortality.
MATERIALS AND METHODS
Setting
Singapore is a highly urbanized city-state spanning over 718.3 square kilometers of land mass and with a population of 5.3 million. 8 At the time of the study, there were six major public hospitals and seven private hospitals equipped with modern EDs.Reference Wen, Venkataraman and Sullivan 9 The National Registry of Diseases Act was enacted in Singapore in 2007, 10 and it mandates that all AMI cases from both the public and private hospitals (mandatory notification for only private hospitals started in 2012) are to be sent to the SMIR, under the National Registry of Diseases Office (NRDO). This includes AMI deaths that occur at home and are certified by a medical practitioner (although the numbers are small). 11
Study population
De-identified data of all STEMI cases presenting to the public and private hospitals between January 2010 and December 2012 were requested from the SMIR and analysed. Patients who suffered out-of-hospital or in-hospital cardiac arrest were transferred from an external facility, and those who developed STEMI only during hospital admission were excluded from the analysis. The rationale for the exclusion was that these patients would have different processes of care.
Data collection
The SMIR used several methods in their data collection process, namely abstraction from medical claims, inpatient hospital discharge summaries and physical case notes, cardiac markers laboratory results, death certificates, and necropsy information. Identification of STEMI cases by the registry coordinators was through the International Classification of Diseases 9th and 10th Revision Codes recorded by attending emergency physicians in the case records. Quality assurance measures include a logic check for dates and categorical data, and range check for numeric data. Illogical data and out of range values were flagged to the registry coordinators for verification.
The data were categorized into two groups: painless and painful STEMI. Painless STEMI was defined as the absence of complaints of pain in the chest, jaw, shoulder, epigastric, and back during the entire ED presentation. Painful STEMI was defined as complaint of pain in any of these locations.
Outcomes
The primary outcome was door-to-balloon time (D2B), defined as the earliest time that the patient arrived in the ED to balloon inflation. Secondary outcomes were 1-month and 1-year mortality rates and occurrence of adverse events such as cardiogenic shock, reinfarction, acute renal failure, heart failure, complete heart block, cerebrovascular accident, and left ventricular systolic dysfunction.
Statistical analysis plan
Data entry was performed using an electronic platform: the National Disease Registries System. Stata version 11 (StataCorp LP, College Station, Texas) was used for data analysis. Missing data were excluded from analysis.
Categorical variables were presented as frequency with percentage and chi-square tests used to determine whether their distributions differed by STEMI pain type (p<0.05). Continuous variables were presented as a median with range, and the Mann-Whitney U test was used to determine whether they differed by STEMI pain type (p<0.05).
Multivariate logistic regression analysis was used to identify independent predictors of D2B >60 minutes; odds ratios with 95% confidence intervals are presented. We used 60 minutes as the cut-off, because both the Global Use of Strategies to Open Occluded Arteries in Acute Coronary Syndromes (GUSTO-IIb)Reference Berger, Ellis and Holmes 12 and NRMIReference Cannon, Gibson and Lambrew 13 trials have shown that the lowest mortality rates were achieved when percutaneous coronary intervention (PCI) was performed within 60 minutes of presentation at the ED. Survival outcomes (1 month and 1 year from admission date) were estimated using a Kaplan-Meier survival analysis; a log-rank test was used to test the survival difference between the painless group and the group with pain. Statistical significance was set at p<0.05. For the Kaplan-Meier survival analysis, the survival time for those who died within 1 month and 1 year was defined as the days from the date of ED admission to the date of death. A Cox proportional hazards regression analysis was used to determine the hazard ratio of painless STEMI on 1-month and 1-year mortality rates. The confounders included in the model were based on both statistical and clinical significance. Survival time was censored at 30 days and 365 days if there was no mortality during the 1-month and 1-year follow-up for both the Kaplan-Meier survival and Cox proportional hazards regression analyses.
Ethics approval
The Central Institutional Review Board granted approval for this research project with a waiver of patient consent, as the data used in this study were de-identified registry data.
RESULTS
Figure 1 shows the patient flow diagram. A total of 6412 STEMI patients were enrolled by the SMIR between January 2010 and December 2012. Patients totalling 1745 were excluded from analysis; 383 were transfer cases, 756 were inpatient STEMI cases, and 797 were cardiac arrest cases, leaving 4667 cases eligible for analysis.
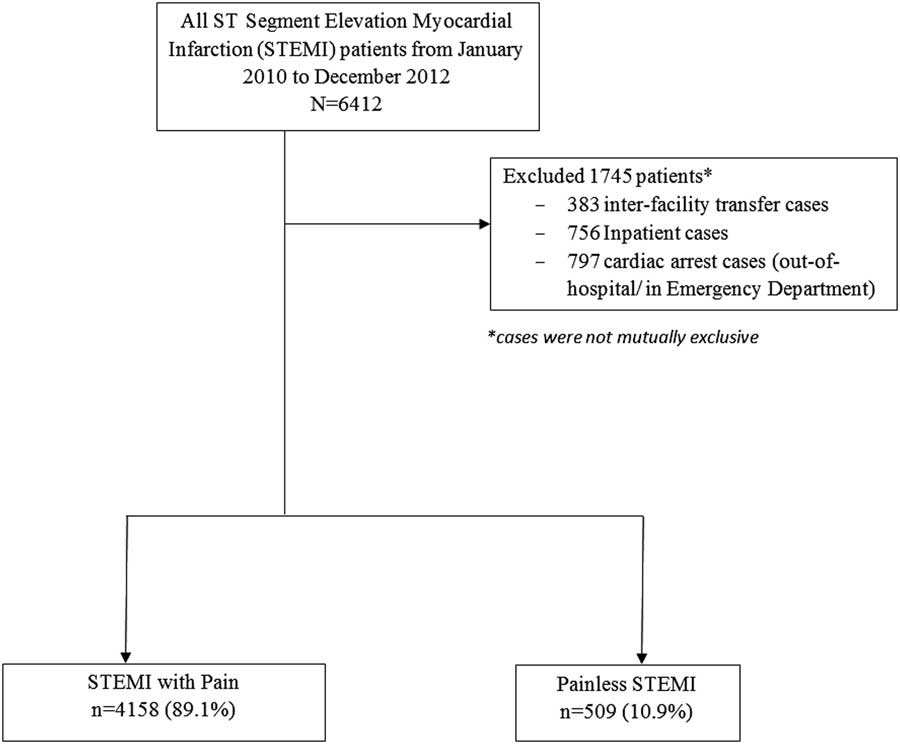
Figure 1 Patient flow diagram.
STEMI patients totalling 4158 presented with pain, and 509 patients presented without any pain to the EDs. Table 1 shows patients’ baseline characteristics. Painless STEMI patients were older (median age=75 v. 58 years old, p<0.001), more likely to be female (39.9% v. 16.1%, p<0.001), and of Chinese ethnicity (74.9% v. 62.7%). They also tended to have higher rates of past medical history of diseases such as hypertension (71.1% v. 54.6%, p<0.001), diabetes mellitus (48.6% v. 37.0%, p<0.001), and AMI (20.0% v. 12.3%, p<0.001), but lower rates of history of dyslipidemia (55.3% v. 62.6%, p<0.01) and PCI (6.1% v. 9.9%, p<0.01). The majority of painless STEMI patients had never smoked before (60.7% v. 37.5%, p<0.001) and also had a higher body mass index (BMI) than the painful STEMI patients (24.5 v. 22.1, p<0.001). Painless STEMI patients were more likely to present with syncope (6.7% v. 1.9%, p<0.001) than diaphoresis (19.8% v. 68.8%, p<0.001) compared to the group with pain. Painless STEMI patients were more likely to present with heart failure (Killip class 2 to 4), compared to painful STEMI patients.
Table 1 Baseline characteristics of patients

CK=creatine kinase; CK-MB=creatinine kinase–muscle/brain isomer; STEMI=ST segment elevation myocardial infarction.
*Statistically significant (p<0.05).
† Defined as registration time other than Mondays to Fridays, between 0800 and 1700.
Table 2 shows the process-of-care timings and patient outcomes. Painless STEMI patients had longer D2B time (80.5 v. 63 minutes, p<0.001). In terms of adverse outcomes, painless STEMI patients were more likely to suffer cardiogenic shock (11.8% v. 4.1%, p<0.001), heart failure (22.4% v. 10.1%, p<0.001), complete heart block (4.9% v. 3.3%, p<0.05), acute renal failure (14.9% v. 4.8%, p<0.001), and death within 30 days (38.4% v. 5.7%, p<0.001) and 1 year from admission (47.3% v. 8.5%, p<0.001). The group with pain was more likely to have left ventricular systolic dysfunction (69.8% v. 62.3%, p<0.001) as an adverse outcome. Using the Kaplan-Meier survival analysis and log-rank test, we found that survival outcomes were significantly poorer in the painless group (68.5%, 95% CI 64.2 - 72.4, p<0.001) than the group with pain at 1 month (96.1%, 95% CI 95.5 - 96.6, p<0.001) and similarly at 1 year from admission (54.8%, 95% CI 50.3 - 59.0, p<0.001 v. 92.4%, 95% CI 91.6 - 93.2, p<0.001) (Figure 2). In a multivariate Cox proportional hazards regression analysis, age, race (Indian and Malay), past medical history of diabetes mellitus and AMI, smoker, ex-smoker, Killip class 2 to 4, and painless presentation were significantly associated with a higher risk of mortality outcomes at 1 month and 1 year. Painless STEMI patients were 2.9 and 2.5 times more likely than the group with pain to die from any cause during the 1-month (HR 2.85, 95% CI 2.21 - 3.68) and 1-year follow-up (adjusted HR 2.46, 95% CI 2.03 - 2.99).
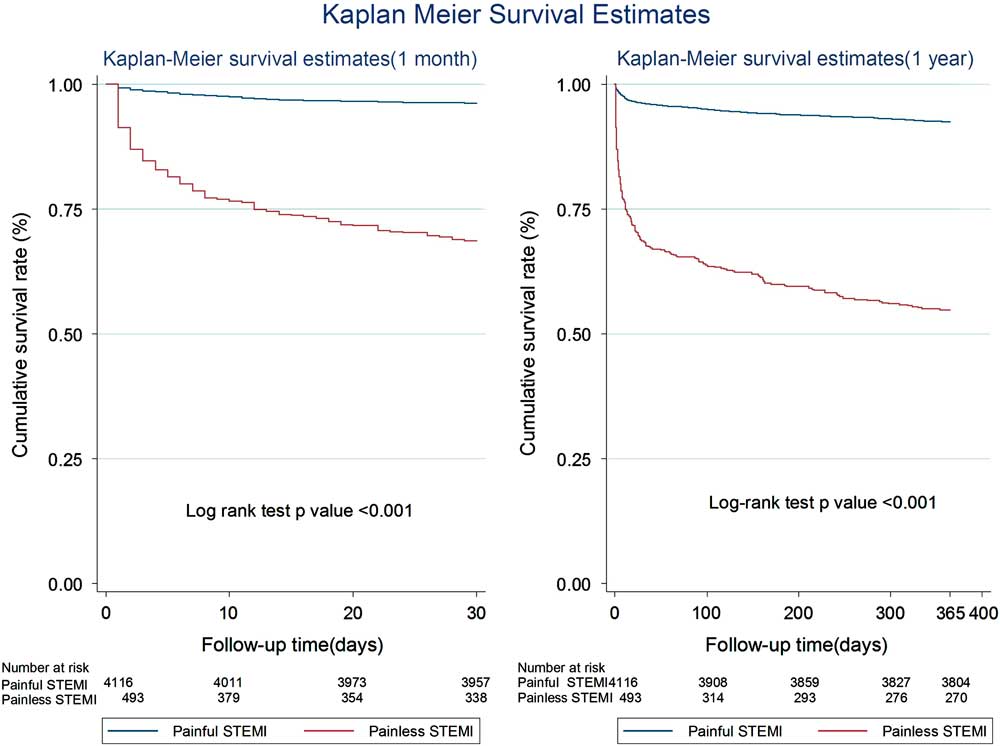
Figure 2 Kaplan-Meier survival analysis at 1 year from date of admission. STEMI=ST segment elevation myocardial infarction.
Table 2 Process-of-care timings and patient outcomes
*Statistically significant (p<0.05).
PCI=percutaneous coronary intervention; PTCA=percutaneous transluminal coronary angioplasty; STEMI=ST segment elevation myocardial infarction.
Table 3 shows the multivariate model for independent predictors of D2B >60 minutes. After multivariate analysis, painless presentation of STEMI remained an independent predictor for D2B >60 minutes (OR 1.89, 95% CI 1.12 - 3.20, p=0.02). In addition, other independent predictors identified were female gender, past medical history of coronary artery bypass grafting surgery, private transport utilization, after-office-hours presentation, and Killip classes 3 and 4.
Table 3 Independent predictors of door-to-balloon (D2B) time more than 60 minutes
*Statistically significant (p<0.05).
Variables that were found to be significant in the univariate analysis (age, female gender, history of CABG, Killip class, painless STEMI, after office hours presentation, and private transport) and other variables (history of PCI and AMI) known to impact process-of-care time intervals were included in the model.
STEMI=ST segment elevation myocardial infarction.
DISCUSSION
The present study shows that about 11% of STEMI patients who presented to the ED had no complaints of pain and that painless STEMI patients had different clinical profiles from the group with pain. This group of patients tended to be sicker upon presentation at the ED (higher Killip score) and was also more likely to suffer poorer outcomes. Painless STEMI was associated with longer D2B time even after adjusting for other predictors of reperfusion delay in the multivariate analysis. From the study, we observed that the mortality rates at 1 month and 1 year for painless STEMI patients were extremely high, at almost 40% and 50%, respectively, that is, 4-5 out of every 10 painless STEMI patients will die. Compared to the group with pain, painless STEMI patients were 2.9 and 2.5 times more likely to experience 1-month and 1-year mortality rates.
Our study mirrors the findings of the Korea Acute Myocardial Infarction Registry study.Reference Cho, Jeong and Ahn 5 Cho et al. similarly found that 11% of the STEMI patients in their study presented without pain to the hospitals. In congruence to our study, Cho et al. observed that painless STEMI patients were older, more likely to be females, and had higher rates of history of diabetes but lower rates of dyslipidemia. Their study also showed that painless STEMI patients had longer D2B times, were less likely to be offered PCI, and had higher mortality rates (in-hospital and at 1-year post admission).
Previous studies have shown that a longer D2B time was associated with increased mortality and morbidity.Reference McNamara, Wang and Herrin 14 - Reference Brennan, Andrianopoulos and Duffy 16 Hence, a longer D2B time seen in the painless STEMI group (painless group had a D2B of 80.5 minutes, whereas the group with pain had a D2B of 63 minutes) could be one of the contributing factors to their poorer outcomes. A longer D2B time is likely due to a delay in acquiring ECGs, mis-triaging (lower triage priority), and so forth, because of the lack of painful symptoms in this group of patients. The most common presenting symptom amongst painless STEMI patients was breathlessness (56.6%), followed by diaphoresis (19.8%) and syncope (6.7%).
Recent studies have suggested that symptom-to-door (S2D) and symptom-to-balloon (S2B) times are better indicators of outcomes in STEMI patients.Reference De Luca, Suryapranata and Zijlstra 17 - Reference Afilalo, Piazza and Tremblay 19 However, for the painless group, S2D and S2B times may not be the best indicators of outcomes. As we noted in our study that, although the S2D and S2B times of the painless STEMI group were shorter as compared to the group with pain, outcomes were poorer. We postulated, however, that ischemia might be more likely to have begun in the painless group before the development of any symptoms. One indicator of long ischemia time in the painless group is that a larger proportion of these patients presented with higher Killip classes at the EDs (see Table 1). Hence, poorer outcomes of this group of patients could possibly be explained by their longer total ischemic time.
STRENGTHS AND LIMITATIONS
The strength of this study was the usage of the national registry data, which represented all AMI cases reported from both public and private hospitals in Singapore. One of the limitations of a registry study is that the associations observed are not causative, that is, treatment delays and poorer outcomes may be due to other confounders apart from painless presentation. We found, however, in the multivariate analysis, that painless presentation independently predicted longer D2B time and 1-month and 1-year mortality rates.
We also note that the distribution of sample size between the painless group and the group with pain was not equal, with the sample ratio at approximately 1:8. However, this study is a population-based one rather than a sample-based study and thus gives a true reflection of the STEMI population in Singapore. Moreover, there was minimal selection-bias because the patients in each group were categorized according to their presenting symptoms; presenting symptoms were extracted by registry coordinators who were independent from the study. Future studies, however, could explore a study design involving matched controls to circumvent this issue.
Cho et al.Reference Cho, Jeong and Ahn 5 posited that the higher frequency of the presence of Q waves on the ECGs of painless STEMI patients in their study was indicative of the longer ischemia time of this group of patients. However, in our study, we did not collect detailed ECG readings and thus are not able to offer additional support for our conjecture that the painless STEMI patients in our study had longer ischemia time.
Additionally, we did not collect other pertinent information such as triage priority and other processes of care timings (e.g., time ECG was acquired) in our study. Such information would help elucidate the reasons for treatment delays in the painless STEMI group.
FUTURE PLANS
Triage nurses and clinicians could be made aware of the profile of this subgroup of patients and instructed to order timely ECG for patients who present with diaphoresis, breathlessness, and syncope, despite the absence of pain complaints. Public educational efforts are also needed to educate the public to seek early treatment when they encounter such symptoms and especially so if they have a past medical history of diseases such as diabetes, hypertension, and AMI. Future studies can also collect and analyse information such as processes of care timings, detailed ECG recordings, and so forth, of painless STEMI patients to further elucidate the cause of treatment delays and poorer outcomes in this group of patients. This will help in developing plans for improvement of patient care for these patients.
CONCLUSIONS
A small proportion of STEMI patients presented without any pain to the ED. They tended to have higher D2B times and higher risks of mortality. Targeted effort is required to improve diagnostic and treatment efficiency in this group.
Competing interests: None declared.







