Direct carotid-cavernous sinus fistulas (dCCFs) are high-flow connections between the internal carotid artery (ICA) and the cavernous sinus. Reference Ellis, Goldstein, Connolly and Meyers1,Reference Barrow, Spector, Braun, Landman, Tindall and Tindall2 The majority (75%–80%) of dCCFs are post-traumatic. Reference Ellis, Goldstein, Connolly and Meyers1,Reference Lewis, Tomsick and Tew3 Other causes of dCCF include cavernous carotid aneurysm rupture which can directly decompress into the cavernous sinus. Reference Lewis, Tomsick and Tew3 Classically, these patients present with pulsatile exophthalmos, chemosis, and orbital bruit. Reference Ellis, Goldstein, Connolly and Meyers1,Reference Barrow, Spector, Braun, Landman, Tindall and Tindall2 Here, we report a case of bilateral post-traumatic dCCFs presenting with cerebellar symptoms due to severe posterior fossa congestion. Both CCFs were successfully treated by trans-arterial coiling embolization using an endovascular approach.
A middle-aged patient was involved in a motor vehicle collision that resulted in facial and orbital fractures, a left ICA dissection, and cerebral microhemorrhages that were conservatively managed. There was no evidence of injury to the right ICA. The patient underwent multiple orthopedic surgeries for extremity fractures and was subsequently transferred to a rehabilitation facility.
Six weeks later, the patient presented to the neurosurgical service with a three-day history of difficulty with coordination, worsening diplopia and blurry vision, and severe nausea and vomiting. She also described a three-week history of progressive right-sided intracranial bruit.
On physical exam, the left pupil measured 4 mm and was briskly reactive. The right pupil was 5 mm and slower to react. There was right-eye proptosis, mild conjunctival injection, and a cranial nerve VI palsy. There was also bilateral horizontal gaze nystagmus. The uncorrected visual acuity was 20/50 OD and 20/30–2 OS. There were no ocular bruits. Right-sided dysmetria was noted but no focal motor or sensory abnormality. The patient’s injuries precluded a gait examination.
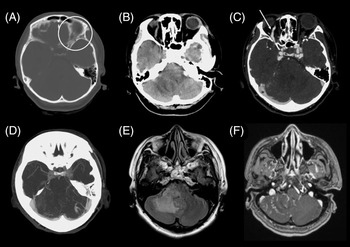
The CT head revealed an area of hypodensity in the right cerebellum and cerebellar peduncle with mass effect and effacement of the fourth ventricle (Figure 1B). CT angiography suggested a right dCCF with arterialization and fullness of the cavernous sinuses bilaterally. Both superior ophthalmic veins (SOVs) were dilated. There was arterialization of the right petrosal sinuses with cortical venous reflux resulting in numerous abnormally dilated and serpiginous vessels in the right cerebellum.

Figure 1: (A–D) CT and (E–F) MR head imaging demonstrates bilateral carotid-cavernous fistulas (CCFs) prior to endovascular intervention. (A) Left orbital and anterior cranial fossa fractures were sustained from a motor vehicle collision six weeks prior to the presentation. (B, E) Edema is noted in the right cerebellum and cerebellar peduncle on CT and MRI, suggestive of congestion. (C) Bilateral direct CCFs were visualized on CT angiography with engorgement of the right (white arrow) and left (not included on slice) superior ophthalmic veins (SOV). (D) Engorgement of bilateral cavernous sinuses and (D, F) distended cerebellar veins are seen on CT and MR angiography.
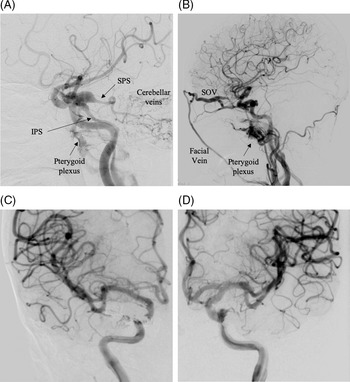
Diagnostic cerebral angiography demonstrated bilateral dCCFs, with the right being more severe than the left (Figure 2A,B). The right CCF drained predominantly via the superior and inferior petrosal sinuses (SPS, IPS). The left CCF drained mainly through the left SOV.

Figure 2: Diagnostic cerebral angiogram with bilateral common carotid injections (A, B) pre- and (C, D) post-coil embolization demonstrate: (A) Right ICA injection demonstrates a direct CCF with early shunting in the jugular vein and venous drainage via the petrosal sinuses, pterygoid plexus, and distension of cerebellar veins. (B) Left ICA injection demonstrates a left CCF with drainage into a distended SOV and superficial facial draining vein. (C, D) Successful treatment of bilateral direct CCFs via endovascular coil embolization and obliteration of the venous pathway. (IPS: inferior petrosal sinus, SOV: superior ophthalmic vein, SPS: superior petrosal sinus.)
Both CCFs were successfully treated by endovascular trans-arterial coil embolization. By the following day, the patient’s visual acuity improved to 20/20 OD and 20/30 OS. At time of discharge a few days later, the right-sided intracranial bruit resolved completely. The patient’s right proptosis and conjunctivitis improved significantly, although the cranial nerve VI palsy remained unchanged. The patient’s cerebellar symptoms, including dysmetria and incoordination, improved, and the symptoms of nausea and vomiting resolved. At the three-month follow-up, the patient’s proptosis and conjunctivitis had resolved completely. She did still have mild residual cranial nerve VI palsy resulting in diplopia with right lateral gaze and was about to follow up with ocular rehab.
Patients with CCFs present with symptoms that relate to their venous drainage patterns. Reference Suh, Lee and Kim4,Reference Aralasmak, Karaali and Cevikol5 Suh et al. examined 58 patients with cavernous sinus dural arteriovenous fistulae and described four drainage patterns that corresponded to clinical presentation. Reference Suh, Lee and Kim4 Orbital symptoms of chemosis, exophthalmos, periorbital pain, and swelling were associated with SOV retrograde flow. Reference Suh, Lee and Kim4 IPS and posterior fossa venous drainage were associated with cavernous symptoms, which consisted of cranial nerve deficits, ptosis, diplopia, anisocoria, and ophthalmoplegia. Reference Suh, Lee and Kim4 Cerebral symptoms were linked to petrosal vein reflux into perimescencephalic or cerebellar veins. Reference Suh, Lee and Kim4 Ocular symptoms, including decreased vision, increased intraocular pressure, pain, glaucoma, and retinal hemorrhage were related to increased venous pressure in the eye. Reference Suh, Lee and Kim4
Our case exhibited two distinct venous drainage patterns on each side. The right fistula drained posteriorly via the petrosal sinuses, which resulted in the dilation of the cerebellar veins and cerebellar symptoms. The patient also exhibited right-sided orbital and cavernous symptoms, and accordingly both CT and MR studies demonstrated bilateral SOV dilation. However, cerebral angiography did not show flow through the right SOV. These findings suggest possible spontaneous thrombosis of the right SOV, a feature that is a high risk for hemorrhage (Figure 2A). The patient’s only left-sided symptom was decreased visual acuity, consistent with congestion of the SOV (Figure 2B).
dCCFs rarely present with cerebellar symptoms secondary to edema from cerebellar venous congestion. The few reports of cortical venous congestion in dCCFs have predominantly described brainstem congestion. Reference Ract, Drier and Leclercq6 To our knowledge, there have been three reported cases of cerebellar edema and hemorrhage resulting from dCCFs: one case was post-traumatic in etiology, one was iatrogenic, and another occurred after a carotid artery aneurysm rupture. Reference Iampreechakul, Tanpun, Lertbusayanukul and Siriwimonmas7 In many cases of cortical venous congestion, there were underlying anatomical abnormalities, such as a non-patent SPS or hypoplasia of the basal vein of Rosenthal. Reference Ract, Drier and Leclercq6 Angiography did not identify any anatomical abnormalities in our patient.
Cortical venous reflux is an uncommon and high-risk feature of CCFs that predicts the risk of hemorrhage. Cerebellar congestion itself is a rare complication. Our case is unique in exhibiting two distinct venous drainage patterns from bilateral CCFs including cerebellar venous congestion without hemorrhage in a patient with a dCCF.
Disclosures
The authors have no conflicts of interest to declare.
Statement of Authorship
All the authors were involved in the conception of the project. CG, MdeLB, and NM drafted the manuscript, and JMO, MAA, and JHW were involved in editing.