Introduction
Traumatic brain injury (TBI) is a significant health concern worldwide, presenting on a spectrum from mild to severe, which can lead to short or long-term disability and reduced quality of life. Reference Carroll, Cassidy and Peloso1 Approximately 80% of all TBI is classified as mild and is frequently referred to as a concussion. Reference Scholten, Haagsma and Andriessen2 In Canada, the incidence of concussions is steadily increasing. Reference Rao, McFaull, Thompson and Jayaraman3 According to the Canadian Community Health Survey, the annual incidence of self-reported concussion increased from 1.9% in 2009 to 3.2% in 2014. Reference Rao, McFaull, Thompson and Jayaraman4 Increasing trends in incidence were also observed by analyzing Ontario physician billing codes for concussion from 2008 to 2016. Reference Langer, Levy and Bayley5 These trends likely reflect a growing awareness of concussions among the public as well as healthcare providers, Reference Rao, McFaull, Thompson and Jayaraman3 in part due to a growing understanding of the long-term consequences of head injuries. Reference Manley, Gardner and Schneider6,Reference Finkbeiner, Max, Longman and Debert7
While most adults who experience a concussion will see a resolution of symptoms within 10–14 d, between 20% and 40% will experience symptoms more than 3 months post-injury. Reference Hou, Moss-Morris, Peveler, Mogg, Bradley and Belli8,Reference Sigurdardottir, Andelic, Roe, Jerstad and Schanke9 When symptoms persist beyond expected recovery, patients may be diagnosed with post-concussional syndrome (PCS). Reference Voormolen, Cnossen, Polinder, Von Steinbuechel, Vos and Haagsma10 According to the International Classification of Disease-10 (ICD-10) PCS criteria, PCS is a syndrome that describes the constellation of persistent symptoms that develop following a concussion, including headaches, dizziness, fatigue, irritability, difficulty concentrating and performing mental tasks, impairment of memory, insomnia, and reduced tolerance to stress, emotional excitement, or alcohol. 11 In the past, some studies have used the term PCS to refer to the acute symptoms in the weeks following concussion; therefore, there has been a shift toward using the term persistent post-concussion symptoms (PPCS) in more recent research. For the purpose of this study, we will use the term PPCS for greater clarity on the persistent nature of the condition experienced by our study cohort.
PPCS can be difficult to treat, as many symptoms are nonspecific, can be present in non-TBI populations, and also overlap with the symptoms of common mental health disorders. Reference Voormolen, Cnossen and Polinder12 Associated musculoskeletal injuries at the time of concussion, especially whiplash-type injuries, can also prolong recovery if inadequately diagnosed and treated. Reference McCrory, Meeuwisse and Dvořák13 Given its complexity, the Ontario Neurotrauma Foundation Guidelines for the treatment of concussion/mild TBI and persistent symptoms recommend a comprehensive, multidisciplinary approach to patient-centered care. Reference Rytter, Westenbaek, Henriksen, Christiansen and Humle14,Reference Jaber, Hartwell and Radel15
The persistence of post-concussion symptoms can have a great impact on work, school, and social relationships leading to reduced health-related quality of life (HRQOL). Reference Scholten, Haagsma and Andriessen2 In other chronic conditions where clinical presentations and the extent of recovery are variable, HRQOL is an important patient-reported outcome that can guide rehabilitation goals. Reference Von Steinbüchel, Wilson and Gibbons16 HRQOL is defined as “a person’s perspective on [their] subjective health condition, functioning, and well-being in the domains of physical, psychological, social, and daily life” Reference Von Steinbüchel, Wilson and Gibbons16 and can provide valuable information about the success of interventions. The relationship between PPCS and HRQOL is an emerging area of interest. A recent large cohort study found that 6 months post-injury, adult patients with PPCS reported significantly lower HRQOL than patients with concussion who did not develop PPCS following their injury. Reference Voormolen, Polinder, von Steinbuechel, Vos, Cnossen and Haagsma17 Mental health may be an important contributor to HRQOL, as a recent study found that high depression and anxiety scores were related to poorer HRQOL. Reference Doroszkiewicz, Gold, Green, Tartaglia, Ma and Tator18 However, most of the research investigating predictive factors for reduced HRQOL has been conducted in pediatric populations, Reference Plourde, Yeates and Brooks19,Reference McGuine, Pfaller and Kliethermes20 or in samples of highly specialized elite and professional athletes. Reference Kerr, Marshall, Harding and Guskiewicz21,Reference Rice, Parker, Rosenbaum, Bailey, Mawren and Purcell22 While sport-related concussions have been critical to accelerating research in the field, other mechanisms such as falls and motor vehicle accidents account for a greater proportion of adult concussion than sport or recreation. Reference Feigin, Theadom and Barker-Collo23
Factors such as older age, female gender, history of prior head injuries, and premorbid mental health conditions have been linked to the development of greater post-concussion symptom burden. Reference Iverson, Gardner and Terry24 Previous studies have also shown that in patients with PPCS, there is a relatively high prevalence of psychiatric disorders (31%), depression (9%), anxiety (9%), and fatigue (32%). Reference Stulemeijer, Van Der Werf, Bleijenberg, Biert, Brauer and vos25,Reference Bryant, O’Donnell, Creamer, McFarlane, Clark and Silove26 It is unclear whether these or other factors influence self-reported HRQOL. As such, there is a substantial need for research examining the experiences of adults with PPCS and what factors impact the quality of life. The primary objective of this study was to examine how patient demographics, injury characteristics, and clinical outcome measures of specific post-concussion symptoms (fatigue, depression, anxiety) are related to HRQOL in adults with PPCS. We hypothesize mood disorders and fatigue substantially influence HRQOL, and therefore the second objective of the study was to determine the relationship between depressive symptoms at the time of clinic visit and patient characteristics.
Materials and Methods
We examined a cohort of adult patients with PPCS presenting to a specialized brain injury clinic in Calgary, Alberta, Canada. This study was nested in a larger study exploring the relationship between growth hormone deficiency and clinical outcomes in patients with PPCS and was approved by the Conjoint Research Ethics Board at the University of Calgary (REB19-0663). As this was a retrospective cohort study, informed consent was not required. Prior to being seen in the clinic, individuals were asked to complete a series of clinical questionnaires, including the Quality of Life after Brain Injury (QOLIBRI), Reference Von Steinbüchel, Wilson and Gibbons16 Rivermead Post-Concussion Symptoms Questionnaire (RPQ), Reference King, Crawford, Wenden, Moss and Wade27 Patient Health Questionnaire-9 (PHQ-9), Reference Fann, Bombardier and Dikmen28 Generalized Anxiety Disorder Scale-7 (GAD-7), Reference Spitzer, Kroenke, Williams and Löwe29 and the Fatigue Severity Scale (FSS). Reference Krupp, Larocca, Muir Nash and Steinberg30 Data were collected prior to their first visit to the clinic and stored on an online platform (Research Electronic Data Capture (REDCap) database) requiring multifactor authentication. A research assistant was available for assistance via phone or email to aid in the completion of the survey.
Participants
Data collection occurred between April 2018 and March 2020. Inclusion criteria were (1) aged 18 and above; (2) diagnosis of concussion (meeting the American Congress of Rehabilitation diagnostic Criteria for mild TBI) Reference Kay, Harrington and Adams31 and meeting ICD-10 criteria for PCS 11 ; (3) 3 months–5 years since the concussion; and (4) completion of all clinical questionnaires. Self-reported patient and injury characteristics were collected including age, sex, level of education, employment status, months since injury, mechanism of injury, whether there was loss of consciousness at time of injury, and total number of self-reported previous concussions. Past psychiatric history (depression, anxiety, post-traumatic stress disorder (PTSD), substance use disorder, bipolar disorder, and psychotic disorders) was extracted from the medical records at the initial visit to the brain injury clinic. Participants were excluded if the clinical outcome questionnaires were not completed or they had a previous moderate/severe TBI or other acquired brain injury.
Clinical Outcome Measures
Quality of Life After Brain Injury (QOLIBRI)
The QOLIBRI was developed to assess HRQOL in patients who have sustained a TBI. Reference Von Steinbüchel, Wilson and Gibbons16 This 37-item questionnaire consists of 6 subscales (cognition, self, daily life and autonomy, social relationships, emotions, and physical problems). Each subscale is scored out of 5, which is then converted to a total score of 100, with higher scores reflecting better HRQOL. Reference Von Steinbüchel, Wilson and Gibbons16
Rivermead Post-Concussion Symptoms Questionnaire (RPQ)
The RPQ is a frequently used measure of symptom burden in PCS research. Reference King, Crawford, Wenden, Moss and Wade27 It is a 16-item measure of commonly reported post-concussion symptoms with each item scored from 0 to 4. A total score is calculated out of 64 with higher scores indicating higher levels of symptom burden.
Patient Health Questionnaire (PHQ-9)
The PHQ-9 Reference Kroenke, Spitzer and Williams32 is a commonly used assessment tool to screen for depression following concussion. Reference Fann, Bombardier and Dikmen28 It is a 9-item questionnaire that is scored out of 27 points. Depression scores are classified as mild (5–9 points), moderate (10–14 points), moderately-severe (15–19 points), and severe (20–27 points). Clinically, a score of 10 or greater suggests a need for treatment intervention. Reference Kroenke, Spitzer and Williams32 Due to the clinical relevance of this cutoff, we have dichotomized scores <10 as none to mild depression and scores ≥10 as moderate or greater depression.
Generalized Anxiety Disorder Scale (GAD-7)
The GAD-7 is a brief validated measure of generalized anxiety disorder. Reference Spitzer, Kroenke, Williams and Löwe29 This is a 7-item questionnaire scored out of a total of 21 points. Anxiety scores are classified as mild (5–9 points), moderate (10–14 points), and severe (15–21 points).
Fatigue Severity Scale (FSS)
The FSS is a 9-item measure assessing the level of fatigue using a 7-point Likert scale with a total score ranging from 9 to 63 points. Reference Krupp, Larocca, Muir Nash and Steinberg30 Higher scores indicate greater fatigue.
Statistical Analysis
Descriptive statistics were used to assess demographic and injury characteristics. Stepwise hierarchical multiple regression was used to analyze the associations between the QOLIBRI score (dependent variable) and the independent variables, including the number of previous concussions, presence of past psychiatric history, RPQ, PHQ-9, GAD-7, and FSS scores. The model was adjusted controlling for sex, age, and months since injury. Further analysis of the PHQ-9 was completed with a binomial logistic regression controlling for age, sex, and months since injury. Statistical significance was defined as p < 0.05. All analyses were performed using SPSS 26 for Mac. 33
Results
Participant selection is presented in Figure 1. Between April 2018 and March 2020, approximately 848 new patients presented to the outpatient brain injury clinic in Calgary, Alberta, Canada. Of these, 325 completed the intake questionnaires and were screened for eligibility with 209 participants presenting with a concussion. Overall, 125 participants met the inclusion criteria. Of those screened for eligibility, reasons for exclusion included alternative diagnosis than a concussion, having incomplete primary outcome measures, or not meeting the criteria for PPCS. Eligible participants were excluded if forms were incomplete. Common reasons for this included time constraints, administration difficulties, and patient decline. Demographic and injury characteristics are presented in Table 1.
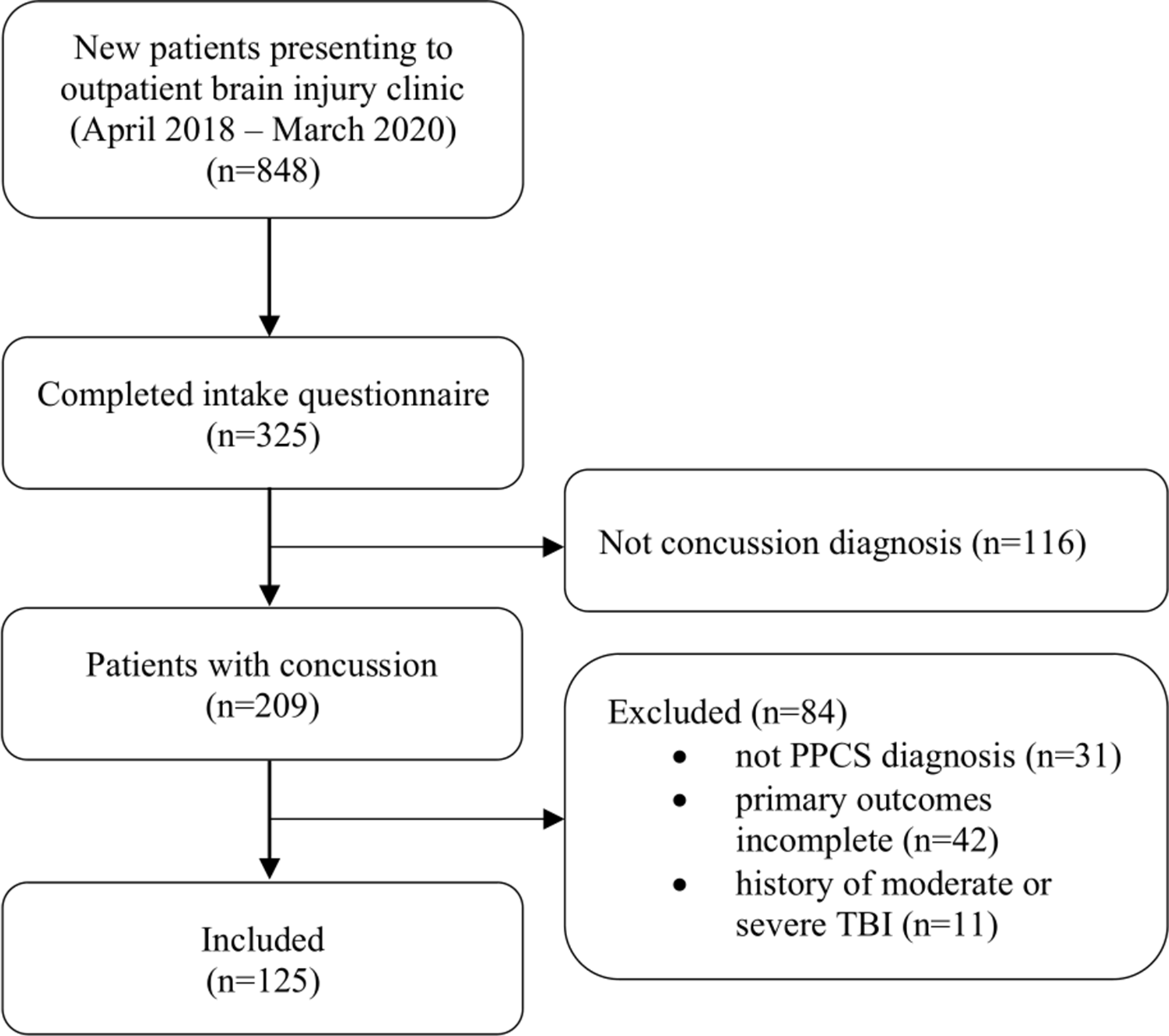
Figure 1. Participant selection with reasons for inclusion and exclusion.
Table 1: Participant demographics and injury characteristics

M = mean; n = number; SD = standard deviation.
Clinical outcome questionnaires are presented in Table 2. Using the PHQ-9 screening tool, 72.8% of participants scored ≥ 10, which is categorized as having moderate or greater depression. On the GAD-7, 55.2% of participants had scores ≥ 10, which is categorized as having moderate or greater anxiety. Further, the average (±SD) PHQ-9, GAD-7, FSS, and RPQ scores were 13.3 ± 5.6, 10.54 ± 5.8, 43.18 ± 12.8, and 37.25 ± 11.9, respectively. The average (±SD) QOLIBRI score was 41.83 ± 17.4.
Table 2: Clinical outcome measures

FSS = Fatigue Severity Scale; GAD-7 = Generalized Anxiety Disorder 7-item; M = mean; n = number;; PHQ-9 = Patient Health Questionnaire 9-item; RPQ = Rivermead Post-Concussion Symptoms Questionnaire; SD = standard deviation; QOLIBRI = Quality of Life after Brain Injury.
Premorbid psychiatric history was prevalent: 41.6% of participants reported a pre-injury history of mental illness: 28.8% depression, 25.6% anxiety, 9.6% PTSD, and 4.0% substance use disorder. There were no participants with a history of bipolar or psychotic disorders. Of the 52 participants reporting a past history of psychiatric illness, 26 (50%) reported having 2 or more mental health diagnoses.
The relationship between clinical outcome measures and QOLIBRI scores is presented as scatterplots in Figure 2. The PHQ-9 had the strongest correlation (r(123) = −.685, p < .001), followed by the GAD-7 (r(123) = −.489, p < .001), the FSS (r(123) = −.438, p < .001), and the RPQ (r(123) = −.392, p < 0.001). Next, a set of clinically relevant potential predictors were chosen, including the number of previous concussions, past psychiatric history, RPQ, FSS, PHQ-9, and GAD-7. Using stepwise hierarchical multiple regression controlling for age at assessment, sex, and months since injury, the PHQ-9, FSS, and GAD-7 were significant predictors of QOLBRI in the model. Together, they accounted for 48.1% of the variance in QOLIBRI scores (R2 = .481, p < .001). The PHQ-9 was associated with 42.0% of the variance (B = −1.305, s.e.(B) = .305, t = −4.281, p < .001), FSS scores with 3.5% of the variance (B = −.252, s.e.(B) = .103, t = −2.450, p = .016). and the GAD-7 was associated with 2.6% of the variance in QOLIBRI scores (B = −.582, s.e.(B) = .267, t = −2.184, p = .31). Demographic factors, past psychiatric history, and injury characteristics were not significant predictors of QOLIBRI scores.

Figure 2. Scatterplots of clinical outcome measures compared to QOLIBRI scores. All four measures were significantly correlated to QOLIBRI scores. Abbreviations: QOLIBRI = Quality of Life after Brain Injury; RPQ = Rivermead Post Concussion Symptoms Questionnaire; FSS = Fatigue Severity Scale; PHQ-9 = Patient Health Questionnaire 9-item; GAD-7 = Generalized Anxiety Disorder 7-item.
We further analyzed the PHQ-9 by dichotomizing scores based on the clinically relevant threshold of ≥10 representing moderate or greater depression, Reference Kroenke, Spitzer and Williams32 using binomial logistic regression controlling for age, sex, and months since injury. Number of prior concussions and GAD-7 scores were significantly associated with scoring ≥ 10 on the PHQ-9. For every 1-point increase in GAD-7 scores, participants were 1.38 times more likely to score ≥ 10 on the PHQ-9 (OR 1.380; 95% CI: 1.131–1.682, p = .001). For every additional previous concussion, participants were 2.23 times more likely to score ≥ 10 on the PHQ-9 (OR 2.234; 95% CI: 1.059–4.716, p = 0.035). While these measures were statistically significant, given the small odds ratios, these results are unlikely to be clinically significant. Age, sex, months since injury, loss of consciousness, past psychiatric history, RPQ score, and FSS score were not significant factors differentiating participants with depression scores ≥ 10 on the PHQ-9.
Discussion
The primary objective of this study was to identify factors influencing HRQOL in adults with PPCS. We found measures of depression, fatigue, and anxiety combined to significantly predict HRQOL in patients with PPCS. Age, sex, months since injury, number of previous concussions, past psychiatric history, and RPQ scores did not. Depression scores were the most significant predictor of HRQOL, accounting for 42% of the variance in QOLIBRI scores. The secondary aim of the study was to determine if the severity of depression was influenced by patient characteristics, past psychiatric history, injury characteristics, or specific measures of symptom burden. We found over 72.8% of the patients with PPCS in our cohort scored ≥ 10 on the PHQ-9 (moderate or greater depression) suggesting a need for treatment, and PHQ-9 scores were positively associated with a greater number of previous concussions and higher GAD-7 scores.
Health-related Quality of Life in Patients with PPCS
The Relationship between HRQOL and Depression
The vast majority of previous studies evaluating HRQOL following concussion have been conducted in pediatric and adolescent populations Reference Plourde, Yeates and Brooks19,Reference McGuine, Pfaller and Kliethermes20,Reference Novak, Aglipay and Barrowman34 or in elite athletes. Reference Manley, Gardner and Schneider6,Reference Vargas, Rabinowitz, Meyer and Arnett35 Prior research has also seldom focused on participants experiencing concussion symptoms months to years following their injury – well beyond the expected concussion recovery. Reference Chiang, Guo, Huang, Lee and Fan36 Of the few studies specifically assessing depression and quality of life in patients with PPCS, one was of military personnel at 6 months post-injury, Reference Schiehser, Twamley and Liu37 and the other included a mix of patients with PPCS and those whose PPCS had resolved. Reference Doroszkiewicz, Gold, Green, Tartaglia, Ma and Tator18 Both of these studies found higher depression scores were correlated to poorer HRQOL. Reference Doroszkiewicz, Gold, Green, Tartaglia, Ma and Tator18,Reference Schiehser, Twamley and Liu37 This is in line with the findings in our study, as the PHQ-9 score emerged as the most significant predictor of QOLIBRI scores in an adjusted regression model. This is not surprising, given the well-established relationship between depression and quality of life in both healthy cohorts Reference Malhi and Mann38 and those with other chronic health conditions. Reference Carod-Artal and Egido39-Reference Prisnie, Sajobi and Wang41
The Relationship between HRQOL and Fatigue
In addition to depression scores, the second significant predictor of HRQOL was fatigue as measured by the FSS. Fatigue is one of the most frequently reported chronic symptoms in patients with PPCS, Reference Stulemeijer, Van Der Werf, Bleijenberg, Biert, Brauer and vos25 and it is also common in patients experiencing depression. Reference Schiehser, Twamley and Liu37 In one study, normative data for the FSS in a healthy population showed a mean score of 20.7, and a score of 36 was used to differentiate between healthy controls and patients with chronic diseases (systemic lupus erythematosus and multiple sclerosis). Reference Krupp, Larocca, Muir Nash and Steinberg30 In this study, 5% of healthy controls reported scores of 36 or greater, compared to 91% of patients with multiple sclerosis and 60% of patients with systemic lupus erythematous. Reference Krupp, Larocca, Muir Nash and Steinberg30 In our cohort, patients with PPCS experienced similar levels of fatigue with 73.6% of participants scoring 36 or greater. Similar to our results, a study on veterans with PPCS found both depression and fatigue to be significantly associated with poorer HRQOL at 6 months post-injury. Reference Schiehser, Twamley and Liu37
The Relationship between HRQOL and Anxiety
The relationship between anxiety and HRQOL in patients with PPCS has rarely been studied, but has been explored in other populations suffering from chronic disease. Reference Prisnie, Sajobi and Wang41 In our cohort, there were high levels of anxiety based on their GAD-7 scores at clinic assessment with 55.2% scoring in the moderate or greater categories, although anxiety only accounted for a small percentage of variance in HRQOL. A recent study that used the Depression and Anxiety Stress Scale-42 (DASS-42) in patients with PPCS similarly found that anxiety scores negatively impacted HRQOL. Reference Doroszkiewicz, Gold, Green, Tartaglia, Ma and Tator18 In further analysis, we found there was an association between anxiety and depression, as higher GAD-7 scores were a significant factor for scoring ≥ 10 on the PHQ-9. Given that anxiety and depression are commonly comorbid conditions, Reference Rice, Parker, Rosenbaum, Bailey, Mawren and Purcell22 this finding is not surprising and assessment for anxiety should be considered in patients with PPCS.
The Relationship between HRQOL and Concussion Symptoms
In this study, the RPQ, a general screen of concussion symptoms, was not a significant predictor of HRQOL. Current literature is mixed on this topic. For example, a study of patients with concussion 6 months post-injury reported an inverse relationship between RPQ and HRQOL with patients experiencing PPCS having a greater than a 20% reduction of HRQOL. Reference Voormolen, Polinder, von Steinbuechel, Vos, Cnossen and Haagsma17 As our study only included patients who met PPCS criteria, this may suggest that among those with PPCS other factors such as mental health are stronger contributors to HRQOL than the severity of symptom burden alone. Conversely, our findings support previous studies that have failed to elicit a significant predictive relationship between measures of post-concussion symptom burden and HRQOL. In a study of older adults (65 years and older), higher scores on the RPQ were associated with higher levels of disability at 6 months post-concussion, but were not predictive of HRQOL. Reference Asselstine, Kristman, Armstrong and Dewan42 Another study of middle-aged adults similarly found no relationship between symptom burden and HRQOL, and the only factor that contributed to poor HRQOL was unemployment at 1 month post-injury. Reference Chiang, Guo, Huang, Lee and Fan36 The inconsistency in the literature may be due to the heterogeneous nature of PPCS, and that one global symptom score, such as the RPQ, may be too general to capture the relationship between symptom clusters and HRQOL. Given that the PHQ-9, FSS, and GAD-7 scores were all significant predictors of QOLIBRI in the regression model, and RPQ was not, measures of individual post-concussion symptoms may be more clinically relevant than measures of overall symptom burden in the context of HRQOL.
The Relationship between Time since Injury and HRQOL
We found months since injury did not significantly influence HRQOL in patients with PPCS. Conversely, in a prospective longitudinal study of concussion outcomes in adults at 1, 6, and 12 months post-injury, HRQOL was different at 1 and 6 months post-injury. Reference Losoi, Silverberg and Wäljas43 However, the vast majority of participants achieved full recovery by 1 year and were indistinguishable from the orthopedic injury control group on both the RPQ and QOLIBRI. Reference Losoi, Silverberg and Wäljas43 Of those who experienced persistent symptoms and poor HRQOL at 1 year, the majority had a psychological risk factor (depression, traumatic stress, and/or low resilience) identified at 1 month post-injury. Reference Losoi, Silverberg and Wäljas43 Our cohort represents a subset of patients experiencing PPCS beyond the expected recovery timeline (average time since injury was 14.8 months) and may require a different treatment focus compared to those patients within a year of injury.
The Relationship between Age, Sex, and HRQOL
We found no relationship between age or sex and HRQOL in patients with PPCS. This differs from the findings of a study by Yousefzadeh-Chabok and colleagues, which found women and those of younger age Reference Doroszkiewicz, Gold, Green, Tartaglia, Ma and Tator18–Reference Vargas, Rabinowitz, Meyer and Arnett35 had significantly lower HRQOL scores 6 months post-concussion. Reference Yousefzadeh-Chabok, Kapourchali and Ramezani44 This study used a different measure of HRQOL, the Short Form-36, and it is possible that the difference in findings is due to different measurement tools. Additionally, this sample was recruited from patients who were admitted to hospital in Iran for their initial concussion, Reference Yousefzadeh-Chabok, Kapourchali and Ramezani44 in comparison to referral to a specialized outpatient concussion clinic in our study. Finally, Yousefzadeh-Chabok and colleagues’ data were collected at 6 months post-injury compared to our study in which the average participant was greater than 1-year post-injury, thus reflecting a more chronic condition that may not be influenced by age and sex.
Depression in Patients with PPCS
The Relationship between Depression and Clinical, Injury, and Demographic Characteristics in Patients with PPCS
It is believed that the development and duration of PPCS is the result of a complex interplay of social, physical, cognitive, and psychological factors, and that the perception of one’s injury may be influenced by co-occurring depression. Reference Malhi and Mann38 In Canada, the lifetime prevalence of depression is 11.2%, and is twice as high among women (14.0%) as it is among men (8.4%). Reference Knoll and Maclennan45 Previous literature suggests the prevalence of depression at 1-year post-concussion is approximately 9%, Reference Bryant, O’Donnell, Creamer, McFarlane, Clark and Silove26 however, this includes both patients who have recovered from their initial injury and those who experience PPCS. In our cohort, 28.8% of participants reported a pre-injury history of depression, although 72.8% of participants scored ≥ 10 on the PHQ-9 post-injury. This implies that even those without a depression history are still at risk of developing depressive symptoms when experiencing prolonged recovery from concussion and that multiple other factors may contribute.
This study found that higher GAD-7 scores and a greater number of prior concussions were factors significantly associated with a PHQ-9 score of ≥10. Similar to previous literature, we found anxiety was high in patients with PPCS Reference Bryant, O’Donnell, Creamer, McFarlane, Clark and Silove26 and was significantly related to depression. Though not specifically explored in patients with PPCS, other studies evaluating patients with chronic disease have found anxiety and depression are often comorbid conditions. Reference Prisnie, Sajobi and Wang41 We also found a greater number of prior concussions was significantly associated with depression severity in our cohort. A systematic review completed in 2007 suggests a potential dose-dependent response with regards to the number of head injuries and risk of developing depression. Reference Manley, Gardner and Schneider6 A recent study on patients with PPCS also found that a higher number of prior concussions was associated with elevated depression scores. Reference Doroszkiewicz, Gold, Green, Tartaglia, Ma and Tator18 Though not explored in this study, other important contributors to post-concussion depression severity include social support, coping skills, and access to specialized healthcare services. Reference Kenzie, Parks, Bigler, Lim, Chesnutt and Wakeland46 As depression has such a significant impact on HRQOL, clinicians working with patients who have PPCS should screen for depression, even if there is no past medical history of psychiatric illness.
We did not find a relationship between depression and age, sex, past psychiatric history, months since injury, loss of consciousness, RPQ scores, or FSS scores in patients with PPCS. Previous literature on this topic is mixed. In contrast to our study, Hart and colleagues found that sex and age were factors associated with depression after concussion, as female sex and younger age were associated with higher rates of depression than male sex or older age. Reference Hart, Brenner and Clark47 However, this study did not differentiate between patients who had recovered from their injury versus those with PPCS. Similar to our study, Iverson and colleagues found no sex or age differences in post-concussion depression rates, but in contrast to our study found pre-injury mental health history was significantly associated with the development of depression post-injury. Reference Iverson, Gardner and Terry24 Finally, a premorbid history of depression and anxiety has been associated with post-concussion depression and anxiety, Reference Hou, Moss-Morris, Peveler, Mogg, Bradley and Belli8,Reference Iverson, Gardner and Terry24,Reference Lange, Iverson and Rose48,Reference Iverson, Williams, Gardner and Terry49 however, we did not find a significant relationship between past psychiatric history and severity of post-injury depression. As well, previous studies have found a significant relationship between severity of PPCS (as measured by RPQ scores) and depression, whereas we did not. Reference Schiehser, Twamley and Liu37
Limitations
This study has limitations as it represents a cohort of participants at one time point (initial assessment at an outpatient brain injury clinic), does not examine changes in HRQOL across recovery, and does not have a healthy control group. These patients are a chronically symptomatic group who require specialized treatment for PPCS, and are not representative of all individuals who experience a concussion. Additionally, the results are based on self-reported tools and brief mental health screens (PHQ-9 and GAD-7). These tools reflect symptomatology, but in practice require further evaluation to make formal diagnoses like major depressive disorder or generalized anxiety disorder. There may also be gender and/or cultural differences in responding to certain items on these tools, such as tearfulness on the RPQ. Among the cohort, there was a significant level of mental health burden present with more than two-thirds reporting moderate or greater depression scores. Given depression scores were the most significant predictor of HRQOL in our cohort, our findings may be less helpful in addressing quality of life in patients with PPCS who are not experiencing mental health challenges. Finally, only self-reported concussion history was collected and no previous concussion characteristics were asked. In future studies, collecting concussion history characteristics or using a validated concussion history screening tool should be implemented.
Conclusion
Patients with PPCS are complex and require a multimodal approach to treatment. Our study found that in patients with PPCS, depression, fatigue, and anxiety were significant predictors of HRQOL, and that a history of concussion and anxiety may contribute to more severe depressive symptoms. This suggests a comprehensive approach that addresses the contribution of past medical history, mental health, and fatigue are vital to addressing HRQOL in patients with PPCS. The study provides new information to the existing literature, as we explored the relationship between HRQOL and symptoms in middle-aged adults with concussions due to varying causes. Compared to previous populations studied, this patient population is unique as they have different external stressors than those at either end of the age spectrum, such as work, family, and financial responsibilities. Loss of function and decline in quality of life has a substantial impact during this time of life to the individual as well as to the economy. The results from this study provide important knowledge to aid in targeted treatments to address quality of life in patients experiencing PPCS, and highlight the importance of mental health assessment in this population.
Acknowledgments
The authors acknowledge the Calgary Brain Injury Program (CBIP), specifically Dr. Christine McGovern, Dr. Rodney Li Pi Shan, Matt Machan, and Natalia Kruger for their help with data collection at CBIP. Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at the University of Calgary Clinical Research Unit. REDCap is a secure, web-based application designed to support data capture for research studies providing: (1) an intuitive interface for validated data entry; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for importing data from external sources.
Disclosures
The authors report no conflict of interest.
Statement of Authorship
NP, LJM, and CTD were involved in the conception of the project. RK and LJM assisted in data collection. TF and NP assisted in data analysis and interpretation. NP was primarily responsible for drafting the article. NP, LJM, CTD, RK, and TF all contributed to the critical revisions for submission.






