Introduction
The importance of sexual expression across the lifespan has been well documented. Research consistently highlights associations between sexual activity and improved health (Bauer et al., Reference Bauer, Haesler and Fetherstonhaugh2015; Lee et al., Reference Lee, Nazroo, O’Connor, Blake and Pendleton2016; Lindau et al., Reference Lindau, Schumm, Laumann, Levinson, O’Muircheartaigh and Waite2007), greater enjoyment of life, and overall well-being (Steptoe et al., Reference Steptoe, Deaton and Stone2015). Contrary to stereotypes that position older adults as asexual, positive sexual outcomes are not the exclusive domain of the young. Accumulating evidence, including findings from large population-based studies, shows that older adults not only remain sexually active (Beckman et al., Reference Beckman, Waern, Östling, Sundh and Skoog2014; Traeen et al., Reference Traeen, Štulhofer, Janssen, Carvalheira, Hald, Lange and Graham2019), they also consistently identify continued sexual activity and opportunities for sexual expression as a central factor impacting their quality of life (Lindau et al., Reference Lindau, Schumm, Laumann, Levinson, O’Muircheartaigh and Waite2007).
Despite the reported benefits, sexual expression in long-term care (LTC) homes remains largely overlooked and poorly understood (Dyer & das Nair, Reference Dyer and das Nair2013). This is problematic given that baby boomers tend to hold more positive sexual attitudes and place more importance on sexuality and intimacy than previous cohorts (Fisher, Reference Fisher2010), and many expect to maintain a higher level of sexual interest and frequency of sexual activity in their later years (Das et al., Reference Das, Waite, Laumann, Carpenter and DeLamater2012; Hillman, Reference Hillman2012). Moreover, once in care, they want to be able to access the same sexual health services (e.g., referral to sexual health professionals), sexual aids (e.g., vibrators, condoms, lubricants), and erotic materials as their community-dwelling counterparts (Rahn et al., Reference Rahn, Jones, Bennett and Lykins2020). This study was designed to assess the perceived preparedness of Ontario’s LTC homes in addressing the sexuality needs of LTC residents, and to identify the existing supports, barriers, and key priorities necessary to uphold residents’ rights to sexual expression.
In 2017, the global population of adults aged 60 years and older totalled approximately 962 million, and that number is expected to double by the year 2050, reaching nearly 2.1 billion (United Nations Department of Economic and Social Affairs Population Division, 2015). In Canada, it is estimated that by 2030, baby boomers, people born between 1946 and 1964, will constitute approximately 22% of the population (Statistics Canada, 2023). In the Western world, this cohort is viewed as instrumental in bringing about a profound sociocultural shift in the way sexuality is perceived and expressed, gradually moving from a view of sex for procreation to sex as recreation (Twenge et al., Reference Twenge, Sherman and Wells2015). Baby boomers have enjoyed more liberal and diverse sexual lives than previous generations, and are thus even more likely to consider sexuality as an integral part of their identities and central to healthy aging (Rahn et al., Reference Rahn, Jones, Bennett and Lykins2020). Further, given that sexual identity and sexual attitudes have been shown to remain consistent throughout adulthood (Das et al., Reference Das, Waite, Laumann, Carpenter and DeLamater2012), baby boomers are likely to experience continuity in their perception of Self as sexual and are expected to assert their right to remain sexually active (Das et al., Reference Das, Waite, Laumann, Carpenter and DeLamater2012; Rowntree, Reference Rowntree2014).
As the average age of the population increases, the demand for LTC services is expected to swell reaching 606,000 individuals by 2031, representing a 59.5% increase from 2019 (Canadian Medical Association, 2021). However, following a review of existing documentation, including policy literature (e.g., Government of Ontario, 2022; Ministry of Health and Long-term Care, 2007), working group reports (e.g., Brassolotto & Howard, Reference Brassolotto and Howard2018) and discussion and research papers (e.g., Lester et al., Reference Lester, Kohen, Stefanacci and Feuerman2016; Sussman et al., Reference Sussman, Brotman, MacIntosh, Chamberland, MacDonnell, Daley, Dumas and Churchill2018; Syme et al., Reference Syme, Lichtenberg and Moye2016), it remains unclear whether LTC homes are prepared to meet the shifting needs and expectations of the baby boomer cohort.
Barriers to residents’ sexual expression
Accumulated research confirms that older adults, including those who reside in LTC homes, maintain sexual desire and engage in sexually expressive behaviour even in the presence of cognitive decline (Bauer et al., Reference Bauer, Fetherstonhaugh, Tarzia, Nay, Wellman and Beattie2013; Delamater & Moorman, Reference DeLamater and Moorman2007; Kuhn, Reference Kuhn2002). Yet, a number of challenges hindering sexual expression within the LTC context have been identified. Reported barriers include biological and physical limitations, restrictive staff and family attitudes, and institutional barriers, such as limited privacy, inadequate training, and an absence of specific policies and guidelines informing the facilitation of healthy sexual expression (Bauer et al., Reference Bauer, Fetherstonhaugh, Tarzia, Nay, Wellman and Beattie2013; Elias & Ryan, Reference Elias and Ryan2011; McAuliffe et al., Reference McAuliffe, Bauer and Nay2007).
While expressions of sexuality and intimacy are generally considered to be private, sexual expression becomes increasingly more public within the LTC context. Howard et al. (Reference Howard, Brassolotto and Manduca-Barone2020) highlight how the dichotomous nature of LTC homes; functioning as both a home and a public workspace, creates an ambiguous boundary between private and public space. They observed how behaviours generally considered appropriate for one’s living space (e.g., viewing pornography) may be perceived as inappropriate in a workspace, and competing needs of residents and care staff (e.g., ease of access, patient monitoring) can lead to prioritization of organizational efficiency over residents’ personal needs. Compounding this issue, privacy is limited due to outdated designs favouring communal space (McAuliffe et al., Reference McAuliffe, Bauer and Nay2007). It is generally acknowledged that baby boomers place a much higher value on personal choice and independence and are more actively engaged in their care than previous generations (Gill & Cameron, Reference Gill and Cameron2022; Kahana & Kahana, Reference Kahana and Kahana2014). In fact, researchers suggest that baby boomers are more likely to demand individualized care that meets their specific needs and standards (Gill & Cameron, Reference Gill and Cameron2022).
Negative or restrictive staff attitudes and lack of training have also been shown to hinder residents’ expressions of sexuality (Howard et al., Reference Howard, Brassolotto and Manduca-Barone2020). Staff responses to sexual expression differ according to organizational culture (Tzeng et al., Reference Tzeng, Lin, Shyr and Wen2009), and a range of residents’ characteristics, including the level of cognitive functioning (Villar et al., Reference Villar, Celdrán, Fabà and Serrat2014), gender and sexual orientation (Hinrichs & Vacha-Haase, Reference Hinrichs and Vacha-Haase2010), and the specific nature of the sexual behaviour being expressed (Villar et al., Reference Villar, Serrat, Celdrán and Fabà2016). Moreover, LTC staff hail from diverse cultural and religious backgrounds and some may experience residents’ sexual expression as morally or religiously offensive (Bouman et al., Reference Bouman, Arcelus and Benbow2007); whereas others view supporting later-life sexuality as being outside of their scope of practice (Haesler et al., Reference Haesler, Bauer and Fetherstonhaugh2016). Despite findings indicating that knowledge and training can attenuate negative sexual attitudes (Mahieu et al., Reference Mahieu, Van Elssen and Gastmans2011), a systematic review examining health professionals’ perceptions of later-life sexuality indicated that staff often lack knowledge and perspective, and opportunities for training remain significantly limited (Haesler et al., Reference Haesler, Bauer and Fetherstonhaugh2016).
Another challenge contributing to discomfort within the LTC context is sexual expression in persons with dementia (Doll, Reference Doll2013; Syme et al., Reference Syme, Lichtenberg and Moye2016). Yet, despite cognitive decline individuals with dementia continue to engage in meaningful forms of sexual expression and maintain satisfying sexual relationships. In fact, findings indicate that 70% of couples with at least one partner experiencing dementia-related cognitive decline report continued sexual activity (Davies et al., Reference Davies, Sridhar, Newkirk, Beaudreau and O’Hara2012). The confluence of sexuality and dementia continues to pose a unique set of challenges in the LTC context. The capacity to consent remains a contentious issue, both in terms of public opinion and among staff responsible for providing care (Syme et al., Reference Syme, Lichtenberg and Moye2016). This issue is insufficiently addressed in both the research and policy development contexts.
Despite notable advancements in sexual and gender rights and freedoms in North America, evidence suggests that discrimination and marginalization continue to impede sexual and gender minority elders’ access to necessary health and social services (Dune et al., Reference Dune, Ullman, Ferfolja, Thepsourinthone, Garga and Mengesha2020; Stinchcombe et al., Reference Stinchcombe, Smallbone, Wilson and Kortes-Miller2017) including in the LTC context (City of Toronto & Long-Term Care Homes and Services, 2022; Hinrichs & Vacha-Haase, Reference Hinrichs and Vacha-Haase2010; Sussman et al., Reference Sussman, Brotman, MacIntosh, Chamberland, MacDonnell, Daley, Dumas and Churchill2018). It has been suggested that sexual minority elders are five times less likely to access LTC services than their heterosexual counterparts (Toronto Long-Term Care Homes & Services, 2008) despite increased risk of requiring formalized care due to higher instances of social isolation (e.g., smaller family networks, lack of financial security), and marginalization (Fredriksen-Goldsen et al., Reference Fredriksen-Goldsen, Kim, Emlet, Muraco, Erosheva, Hoy-Ellis, Goldsen and Petry2011; Lowers, Reference Lowers2017).
Multilevel challenges include fear of prejudice or reprisal, exclusion from health policies and practices, lack of knowledge among service providers, and perceptions of inequity in care (City of Toronto & Long-Term Care Homes and Services, 2022; Dune et al., Reference Dune, Ullman, Ferfolja, Thepsourinthone, Garga and Mengesha2020; Kortes-Miller et al., Reference Kortes-Miller, Boulé, Wilson and Stinchcombe2018). Many gender and sexual minority individuals have expressed fear of being compelled to conceal their identity in order to receive quality LTC care (Services & Advocacy for GLBT Elders et al., 2021; Wilson et al., Reference Wilson, Kortes-Miller and Stinchcombe2018). Queer (non-cisgender), bisexual, and transgender residents face even greater risk, as they may experience both discrimination from heterosexual communities and rejection from gay and lesbian communities (Brotman et al., Reference Brotman, Ferrer, Sussman, Ryan, Richard, Orel and Fruhauf2015). Moreover, transgender elders’ ability to choose to disclose, or not, their queer identity becomes compromised in the LTC context, as they will inevitably be outed to staff during personal hygiene and physical care activities (Brotman et al., Reference Brotman, Ferrer, Sussman, Ryan, Richard, Orel and Fruhauf2015).
Facilitators of residents’ sexual expression
LTC administrators and managers generally report positive attitudes towards residents’ sexuality, including those living with dementia (Shuttleworth et al., Reference Shuttleworth, Russell, Weerakoon and Dune2010; Syme et al., Reference Syme, Lichtenberg and Moye2016). Further, LTC administrators’ engagement in cultural change activities supportive of residents’ sexuality has been shown to influence expressions of sexuality among residents (Bentrott, Reference Bentrott2012). These findings align with accumulated research on organizational management, which indicates that leaders’ attitudes, perceptions, and approaches in the workplace (e.g., demonstrating strong values, providing a clear vision, initiating and empowering followers to implement change) can impact organizational outcomes and employee variables, including organizational commitment, morale and performance, behaviours and attitudes, and investment in their work (e.g., Chin et al., Reference Chin, Lok and Kong2019; Loi et al., Reference Loi, Lai and Lam2012).
While care staff may be the first point of contact for residents addressing sexuality-related issues, it falls to LTC administrators to interpret policy, navigate residents’ demands for support and services, respond to family concerns, and manage employee responses while also considering the specific needs and characteristics of the institutional setting (Bentrott & Margrett, Reference Bentrott and Margrett2011). As representatives of their respective homes, LTC administrators are optimally positioned to model appropriate attitudes and responses to residents’ sexually expressive behaviours. Research indicates that they are more likely to recognize residents’ sexuality needs and perceive a greater need for training as compared to direct care staff (Villar et al., Reference Villar, Serrat, Celdrán, Fabà, Martínez and Twisk2020). It stands to reason that this influence would extend to creating more positive environments for residents’ sexual expression, including employees’ willingness to proactively and openly address residents’ sexual and intimacy-related needs.
LTC policies and procedures
In North America, there has been a notable lack of guidance for LTC administrators seeking support to manage issues related to residents’ sexual expression (Lester et al., Reference Lester, Kohen, Stefanacci and Feuerman2016; Syme et al., Reference Syme, Lichtenberg and Moye2016). LTC facilities in Canada are licensed and regulated at the provincial and territorial levels; however, the definition of LTC varies across jurisdictions. In Ontario, LTC homes are overseen by the Ministry of Health and Long-term Care and include residences providing 24-hour nursing and personal care for individuals with complex needs. Until recently, the Long-term Care Homes Act, 2007 (LTCHA), and the associated Residents’ Bill of Rights, served as the sole legislation governing Ontario LTC homes. While the LTCHA was designed to ensure that residents receive a high level of care that upholds their right to live safely, comfortably, and with dignity in an environment that meets their diverse needs (Ministry of Health and Long-Term Care, 2007), review of the LTCHA revealed a significant lack of specific guidelines pertaining to the management of residents’ sexuality needs and related privacy rights.
Shortcomings in the translation of the standards outlined in the LTCHA were recently brought to light, informed in large part by the impact of the COVID-19 pandemic, sparking a vigorous public discourse on upholding seniors’ rights in the LTC context. In April 2022, a decision was made to replace the LTCHA with the Fixing Long-Term Care Act, 2021 (FLTCA). The FLTCA expands on the previous legislation and introduces new provisions aimed at enhancing residents’ safety through increased transparency and accountability and implementing changes in staffing and provision of care, regulation enforcement, and licensing (Government of Ontario, 2022; Ontario Association of Residents’ Councils, 2022). This new legislation represents a positive step towards the provision of quality LTC care that is resident-centered and safe; however, the management of residents’ sexuality needs and related privacy rights remain largely unaddressed.
A small selection of LTC homes and regional health authorities located in Australia, New Zealand, and to a smaller extent, North America, have previously addressed a lack of guidance by developing their own practice guidelines (e.g., River Spring Health, 2000/2017; Vancouver Coastal Health Authority, 2009) or adapting sample policies from other agencies to address specific sexuality-related issues (e.g., Lanark, Leeds, & Grenville Long-Term Care Working Group, 2007; Schindel Martin, Reference Schindel Martin2002), including delivery of culturally competent services for sexually and gender diverse residents (e.g., City of Toronto & Long-Term Care Homes and Services, 2022; Toronto Long-term Care Homes and Services, 2008). However, despite these important initiatives, research continues to underscore a need for province-wide, resident-centred standards of practice (Brassolotto & Howard, Reference Brassolotto and Howard2018; Howard et al., Reference Howard, Brassolotto and Manduca-Barone2020).
Study objectives
Directors and administrators of LTC are uniquely positioned to not only influence the development of policy agendas but also to ensure their implementation at all levels of care. This study draws upon the collective knowledge of LTC professionals in Ontario to explore organizational supports and barriers to the fulfillment of current and future LTC residents’ sexuality-related needs. This research was guided by three research questions:
-
1. What are the attitudes of LTC administrators/Directors of Care regarding later-life sexuality?
-
2. How do LTC administrators/Directors of Care evaluate their LTC home regarding preparedness to receive a new generation of baby boomer residents?
-
3. What key priorities must be met for LTC homes in Ontario to meet the sexual and intimacy needs of LTC residents?
Method
Sampling and procedures
A total of 150 LTC administrators and Directors of Care from Ontario completed the survey. Potential participants were first identified via the Ontario Ministry of Health and Long-Term Care website. A total of 620 invitations to participate were forwarded via email, which included a weblink to the study hosted by Qualtrics©, a web-based survey platform. To broaden our reach, we also placed an invitation to participate in the Ontario Long-term Care Association’s (OLTCA) online digital newsletter. The OLTCA membership represents approximately 70% of the LTC homes in Ontario including private, not-for-profit, and municipal homes (Ontario Long Term Care Association, n.d.). When possible, email delivery failures were resolved through further internet searches, and follow-up emails were sent two weeks later to encourage those who had not yet responded. As an incentive, all respondents were given the opportunity to enter a draw to win a Visa gift card valued at $100. Ethics approval for this study was granted by the authors’ University Research Ethics Bureau.
Measures
Aging sexual knowledge and attitude scale, attitudinal subscale (White, Reference White1982)
The Aging Sexual Knowledge and Attitude Scale (ASKAS) is a 61-item standardized self-report measure designed to assess individuals’ knowledge and attitudes regarding later-life sexuality. The attitudinal subscale consists of 26 items assessing participants’ age-related sexual conservatism/permissiveness (e.g., I would support sex education courses for the staff of nursing homes; An aged person who shows sexual interest brings disgrace to herself/himself.). Respondents were asked to indicate on a 5-point Likert-type scale the degree to which they agree (1) or disagree (5) with each statement. Negatively worded items were reverse scored, and then all items were summed in order to derive a total ranging from 26 to 130. A lower score reflects a more permissive attitude.
The ASKAS has demonstrated satisfactory psychometric properties in diverse samples including older adults and their family members, nurses, students in health-related fields, and aged care staff (e.g., Bouman et al., Reference Bouman, Arcelus and Benbow2007; Chen et al., Reference Chen, Jones and Osborne2017; Cybulski et al., Reference Cybulski, Cybulski, Krajewska-Kulak, Orzechowska, Cwalina and Jasinski2018; White & Catania, Reference White and Catania1983). The ASKAS has demonstrated content and criterion validity. Split-half, internal consistency, and test-retest reliability have been reported in the range of 0.72–0.96 for the attitudinal subscale (White, Reference White1982). In the present study, reliability was satisfactory as demonstrated by a Cronbach’s alpha of 0.78.
Staff attitudes about intimacy and dementia scale (Kuhn, Reference Kuhn2002)
As the ASKAS measure does not assess attitudes specific to sexuality among LTC residents living with dementia, the Staff Attitudes about Intimacy and Dementia scale (SAID) was included. This 20-item self-report measure utilizes a 5-point Likert response scale ranging from agree (1) to disagree (5). It was developed to assist care staff in recognizing their personal attitudes about sexuality in the context of dementia (e.g., Residents who have dementia are not capable of making sound decisions regarding participation in sexual relationships.). Consistent with previous studies focusing on sexuality in the context of dementia (Bauer et al., Reference Bauer, Fetherstonhaugh, Tarzia, Nay, Wellman and Beattie2013; Chen et al., Reference Chen, Jones and Osborne2017) a subset of items (10 of 20) were included in the study questionnaire. Negatively worded items were reverse scored and all items were summed in order to derive a total attitudinal score ranging from 10 to 50. A lower score reflects a higher level of permissiveness.
Socio-demographic questionnaire
Participants were asked to provide demographic information about themselves and their respective LTC home including information related to the participant’s gender and years of experience, ownership of the LTC home (e.g., public, private), relevant cultural and/or religious affiliations, as well as the geographical location of the LTC home.
Baby boomers, sexuality, and intimacy: The Ontario LTC preparedness survey
To address the absence of an instrument to measure LTC professionals’ experiences and perspectives on current and future supports and barriers to residents’ sexual expression, it was necessary to develop some additional survey items. To inform this portion of the survey, we interviewed 5 aged-care stakeholders including senior-level LTC professionals and a representative from a senior pride organization dedicated to enhancing older adults’ quality of life. Their insights, together with knowledge gained from an in-depth literature review, informed the development of questionnaire items related to LTC residents’ sexuality needs. Before distribution, study consultants reviewed the overall content, focus, and clarity of the questionnaire content and adjustments were made accordingly.
This portion of the study questionnaire consists of 20 yes/no, multiple response, rank order and Likert-type scale items. Yes/no questions query respondents’ knowledge or experience of a specific matter or event (e.g., Does your LTC facility currently have a written best practices policy or procedural manual that specifically addresses the care and management of sexually related matters?); whereas, multiple response questions (e.g., In your opinion, which of the following factors currently represent a barrier to meeting residents’ sexual and intimacy needs and expectations within your LTC facility?), rank order questions (e.g., Which of the following barriers that you previously identified would you consider to be top priorities in need of attention? Please rank your responses in order of importance.), and Likert-type questions (e.g., How would you rate the adequacy of your sexual health training with regards to aging sexuality?) capture more detailed information about respondents’ opinions and perceptions on such matters. Throughout the survey, respondents are regularly encouraged to provide additional clarifying information in the form of qualitative responses.
Finally, as completion of this survey may, in and of itself, have an effect on respondents’ perception of their LTC home’s level of preparedness, respondents are asked their opinion on this matter both at the beginning and directly following completion of the survey. Respondents were asked to indicate their answer on a 4-point scale ranging from very prepared (1) to not at all prepared (4).
Data analysis
Study data were analyzed using SPSS, version 22. Usual data screening and cleaning methods were employed. Descriptive statistics and t-tests were used to describe participant and facility characteristics and to assess differences in pre and post-survey perceptions of preparedness. Pearson correlations and multiple regression analysis were conducted to examine relationships among participant characteristics and the two attitudinal measures.
Results
Sample characteristics
Study participants identified predominantly as female (81.3%, n = 122) and Caucasian (73.3%, n = 110). Total number of years working in the LTC industry ranged from 4 to 50 years (M = 21.7, SD = 9.45). Total number of years as LTC administrator/Director of Care ranged from 1 to 40 years (M = 9.81, SD = 7.40). Although the exact number of eligible participants who received the invitation to participate cannot be known, we estimated a conservative response rate of 24% by dividing the total number of valid responses by the total number of LTC homes in Ontario at the time of data collection – during the latter half of 2018. The resulting response rate is modest but is keeping with other research assessing attitudes and perceptions of health care providers (e.g., Doll, Reference Doll2013; Hughes & Wittmann, Reference Hughes and Wittmann2015).
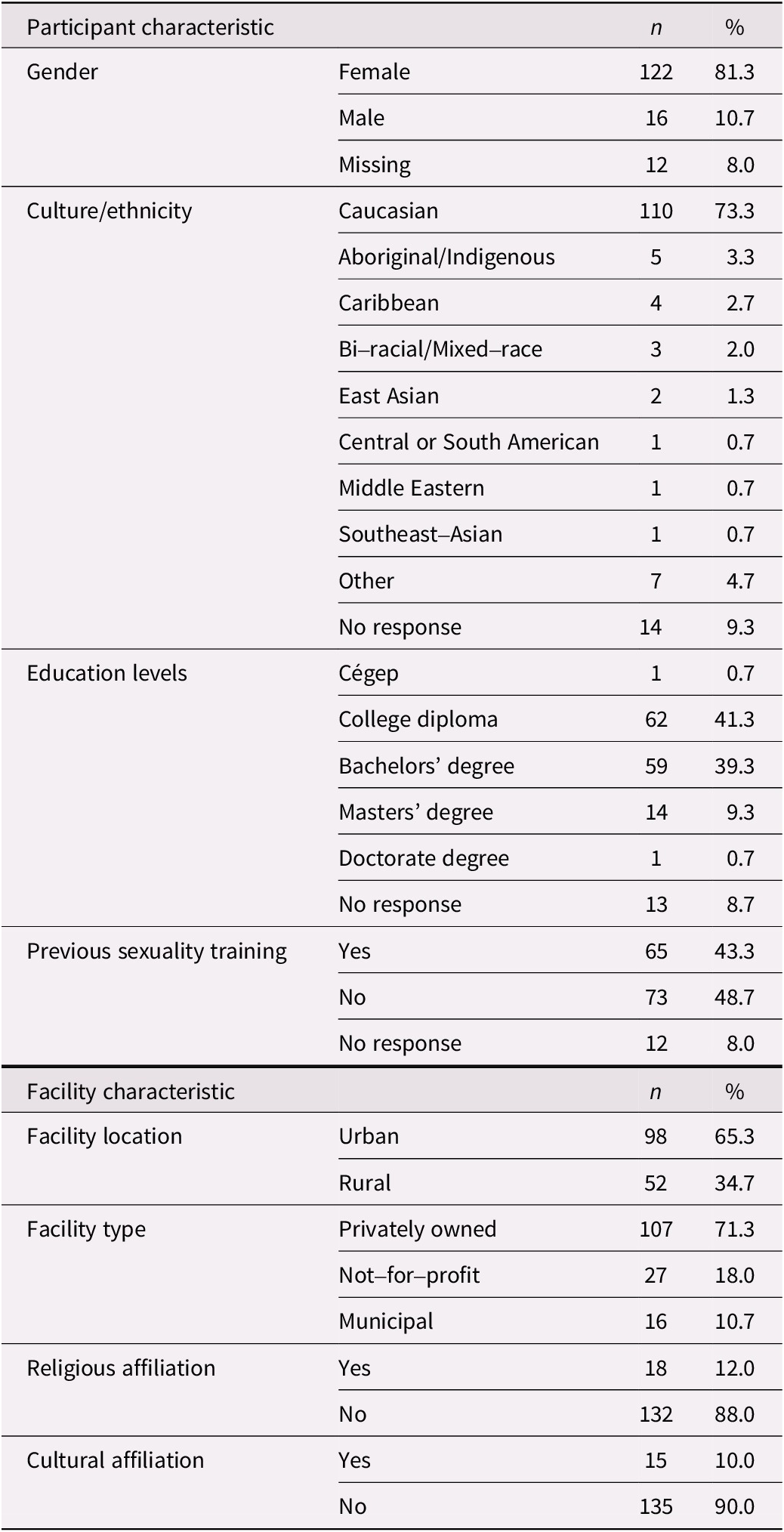
The distribution of participants was comparable to the distribution of LTC homes in Ontario regarding ownership status (i.e., public, for-profit, and not-for-profit). Nearly half of the participants (48.7%) reported no training in sexuality-related issues. In keeping with this, a majority of respondents rated their level of training as inadequate (46.7%) or highly inadequate (12.6%). Regarding self-evaluated knowledge of older adult sexuality, nearly half of the participants rated their knowledge as inadequate (41.6%) or highly inadequate (5.1%). A summary of survey respondents’ characteristics is presented in Table 1.
Table 1. Participant and facility characteristics (n = 150)
Certain characteristics were associated with settings that were more proactive regarding sexuality. Results from correlational analyses indicated settings that had written policies addressing sexuality-related concerns tended to be located in urban settings, r(145) = −0.20, p = 0.015 (2-tailed), have a spiritual or religious affiliation, r(145) = 0.166, p = 0.045 (2-tailed), and include assessment of sexuality-related topics during admission, r(144)= 0.299, p < 0.001 (2-tailed). Table 2 provides information regarding the relationship between facility characteristics and variables associated with the management of sexuality-related issues.
Table 2. Summary of means, standard deviations, and correlations of facility characteristics
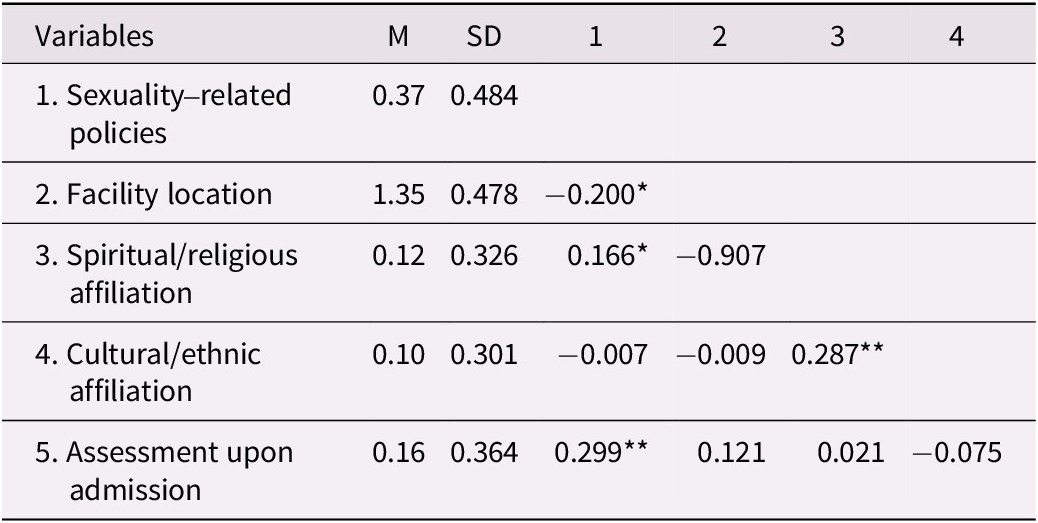
** Correlation is significant at the 0.01 level (2-tailed).
* Correlation is significant at the 0.05 level (2-tailed).
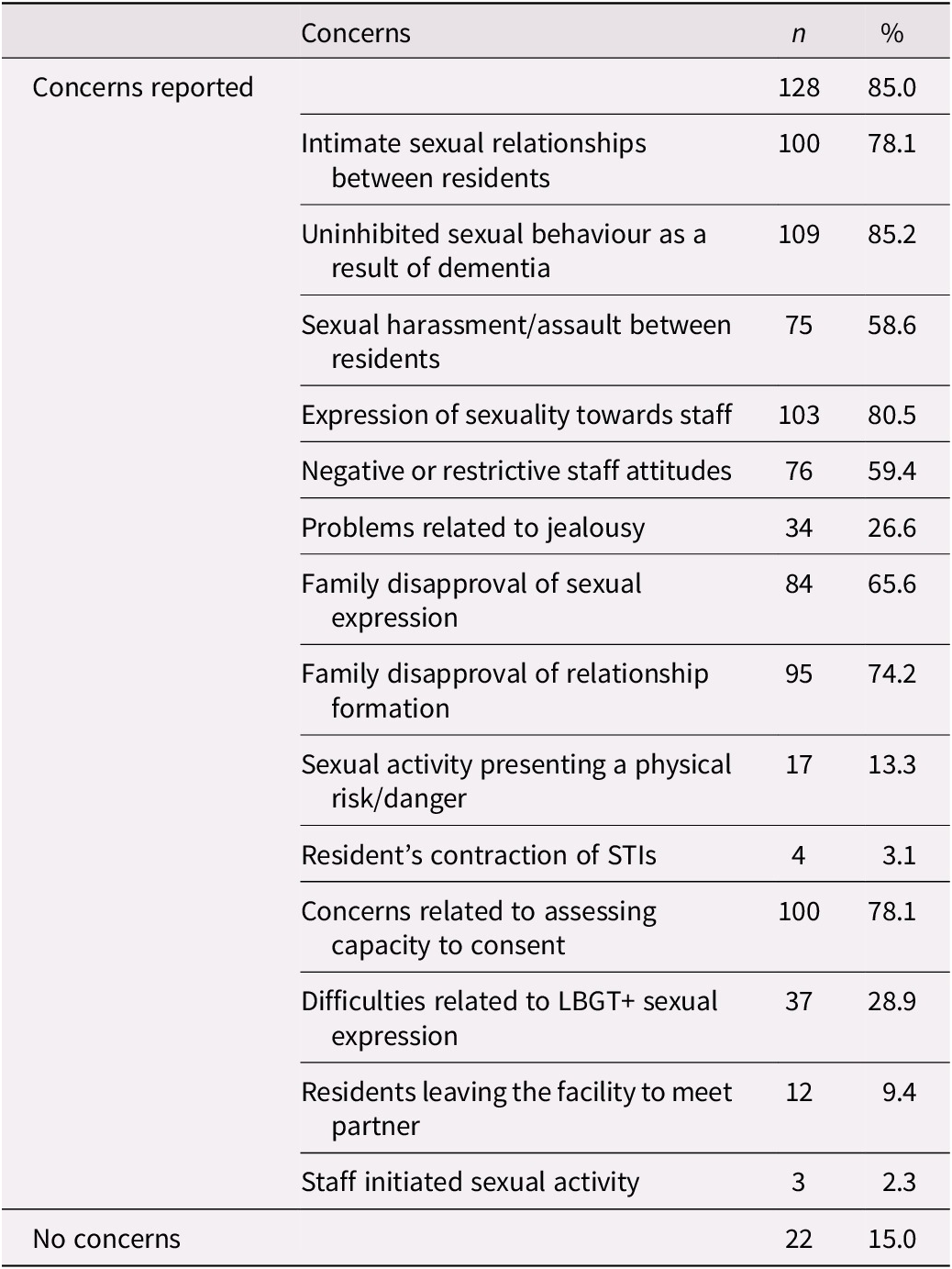
Thirty-seven percent of respondents indicated that their LTC setting has written procedural manuals with specific policies addressing sexuality-related topics. These policies commonly addressed the assessment of capacity to consent, residents’ right to privacy and sexual expression, and sexual abuse. The topics covered in manuals are summarized in Table 3. A minority of respondents (15.5%) reported assessment of sexuality and intimacy needs during admission, with sexual identity and recent changes in sexual behaviour being areas of primary focus. Specific topics addressed during the assessment process are summarized in Table 4. In the day-to-day operations of the LTC homes, however, sexuality-related concerns were reported by 85% of respondents. Table 5 summarizes the range of concerns endorsed. The most frequently (85%) reported concern was demonstrations of ‘uninhibited sexual behaviour as a result of dementia (e.g., public masturbation)’; but a wide range of other sexuality-related issues were also deemed significant by a majority of participants.
Table 3. Sexuality-related issues addressed by policy and procedure manual (n = 147)
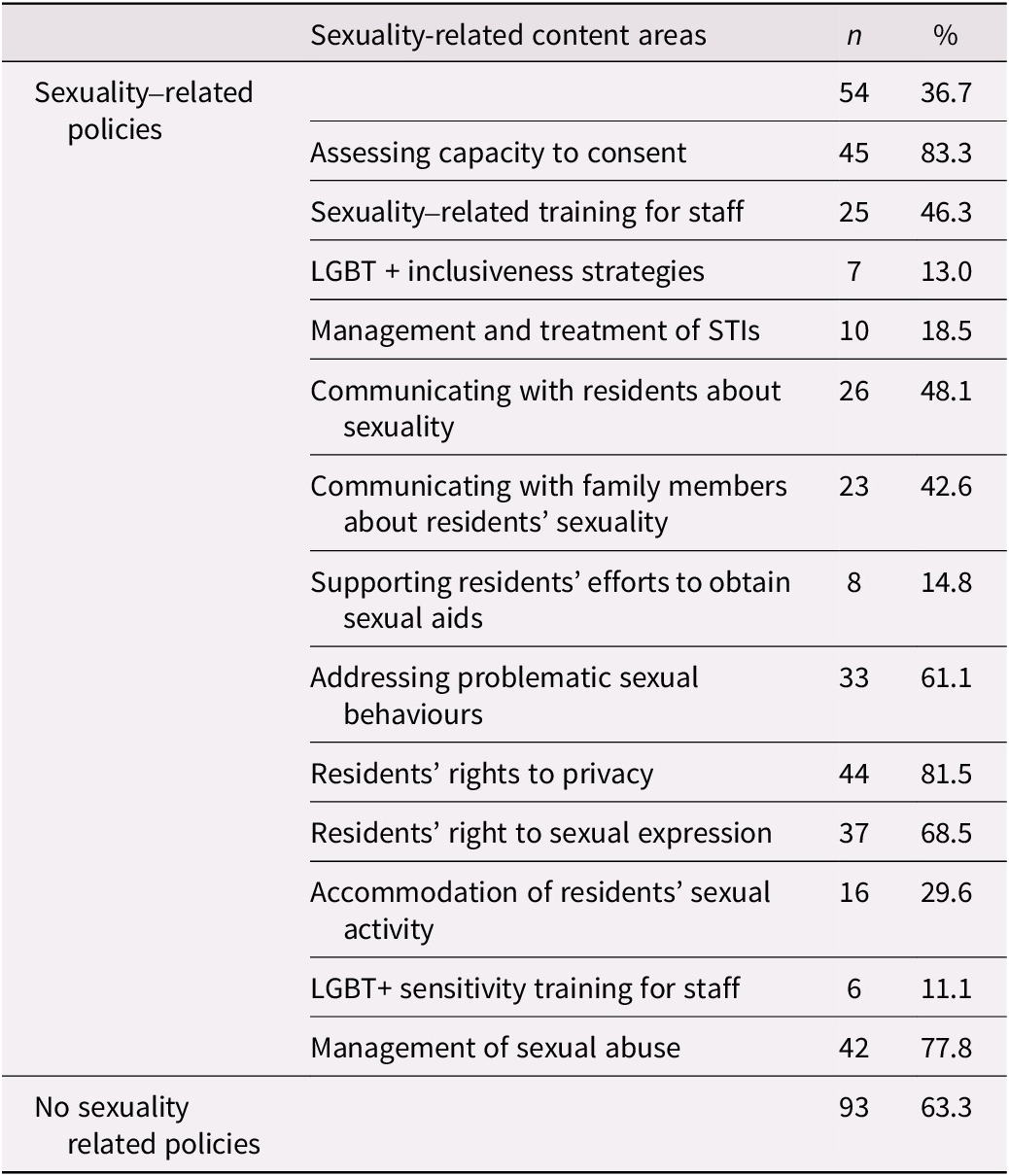
Table 4. Sexuality-related topical areas assessed during the admission process (n = 148)
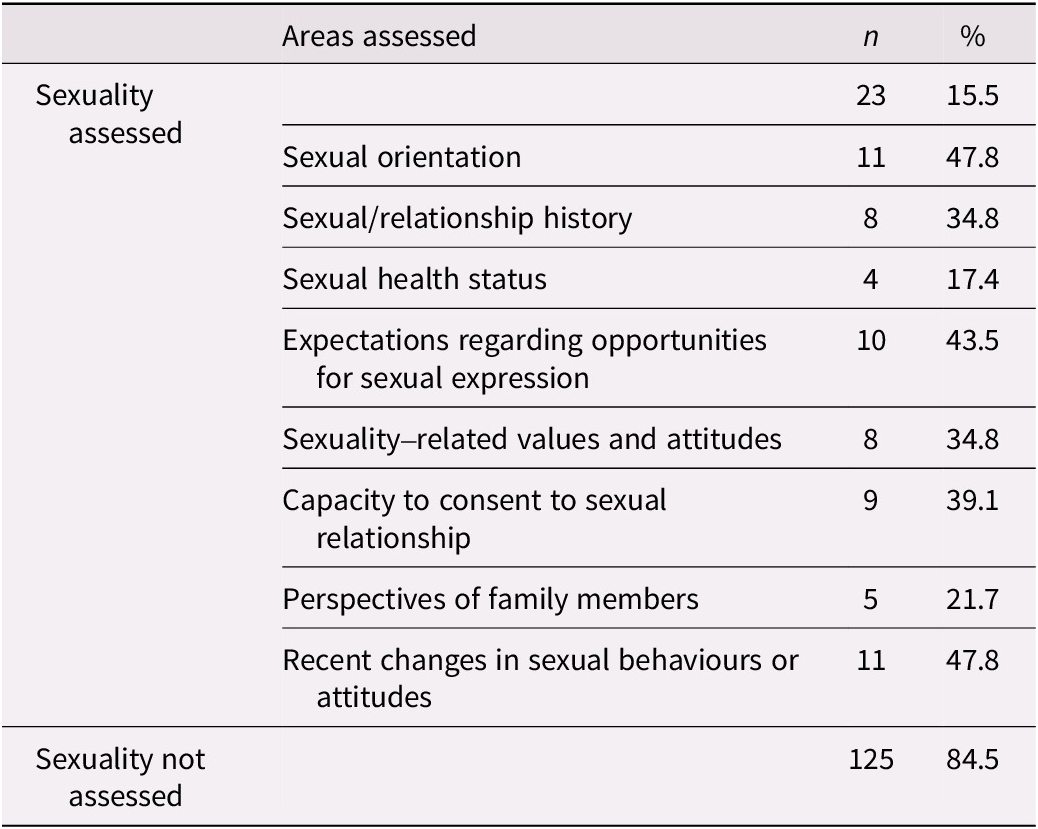
Table 5. Reports of sexually expressive behaviours occurring among residents (n = 150)
Sexual attitudes and associated characteristics
The ASKAS was used to evaluate sexuality-related attitudes; scores ranged from 27 to 73 of a possible 130. Sexually related attitudes regarding residents with dementia specifically were evaluated by the SAID; scores ranged from 14 to 41 of a possible 50. Overall, LTC administrators reported a moderately high (M = 39.59, SD =9.28) level of sexual permissiveness on the ASKAS attitudinal measure, and a moderate (M = 25.41, SD = 6.55) level of sexual permissiveness on the SAID attitudinal measure. Correlational analysis was used to explore the relationship between sexual permissiveness and participant characteristics (see Table 6). Factors associated with more positive and permissive attitudes regarding residents’ sexuality on the ASKAS included having more experience working in the LTC context, r(136) = −0.196, p = 0.033 (2-tailed); and having received training about later-life sexuality, r(136) = −0.214, p = 0.012 (2-tailed). Correlational results also suggested a strong relationship between the two attitudinal measures, r(138) = 0.509, p < 0.001 (2-tailed), however, no association between scores on the SAID attitudinal measure and training or work experience was observed.
Table 6. Summary of means, standard deviations, and correlations of ASKAS, SAID, and participant characteristics
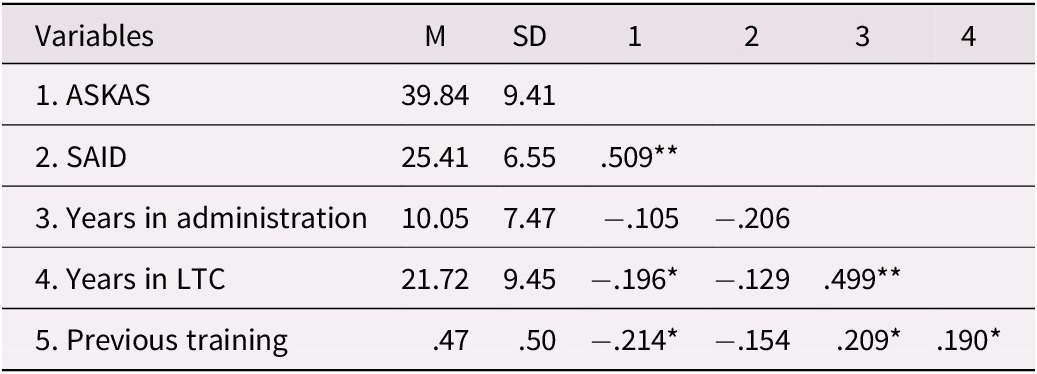
Note: To address issues of non-normality, ASKAS attitudinal scores and years in administration. were normalized using the Thompson two-step method to normality, **p < 0.01 level (2-tailed), *p < 0.05 level (2-tailed).
A multiple linear regression analysis was conducted to examine whether training and years in LTC significantly predicted respondents’ sexual attitudes on the ASKAS attitudinal scale. The results indicated that the model explained 7.1% of the variance (r 2 = 0.071, F(2,135) = 5.15, p = 0.007). However, when the individual predictors were examined, only training significantly contributed to the model (β = −0.183, p = 0.032), accounting for 3.24% of the variance.
Perception of facility preparedness
We anticipated that completion of this survey may prompt some participants to re-evaluate their original assessment of their home’s level of preparedness. We asked respondents their opinion both at the beginning and directly following completion of the survey. Participants’ responses ranged from very prepared (1) to not at all prepared (4). Results of a paired sample t-test indicated a significant difference in respondents’ perception of their home’s level of preparedness before (M = 2.74, SD = 0.863) and after completing the survey (M = 3.05, SD = 0.798), t(136)= −5.46, p = 0.01. These results suggest that there was an effect of survey completion on administrators’ ratings of their facility’s level of preparedness, with administrators reporting less certainty following completion of the survey. Cohen’s effect size value (d = 0.37) suggests a small to medium effect.
Supports and barriers to sexual expression
Descriptive statistics and correlational analyses were used to understand current knowledge and practice with respect to the accommodation of residents’ sexuality needs and to determine the degree of consensus among LTC professionals regarding perceived supports and barriers to meeting future residents’ sexuality-related needs. While a majority of participants endorsed the presence of barriers to residents’ sexual expression, it is noteworthy that 7% indicated that no current barriers exist at their setting. Regarding anticipated future barriers, 11% of respondents believed there would be no significant barriers to meeting future residents’ sexuality needs and expectations. Table 7 provides a summary of current and anticipated future barriers to sexual expression including the specific barriers that respondents prioritized for attention.
Table 7. Current and future barriers and barriers considered top priority (n = 150)

Note: n(%) = frequency and percentage of participants who endorsed the item as being a significant barrier to sexual expression. n(%) priority = frequency and percentage of participants who ranked the item as the top priority requiring attention. M = the mean ranking of each item.
In line with our goal to assess the preparedness of Ontario’s LTC homes to meet current and future residents’ sexual and intimacy needs, we also queried LTC administrators about existing supports. Specifically, we asked them to identify which sexuality-related supports and resources are currently available within their LTC home, which supports and resources they would like to have access to, and which they considered to be top priorities. Existing, desired, and top priority supports and resources are summarized in Table 8.
Table 8. Frequency and percentage endorsement of existing, desired, and top priority supports and resources (n = 150)

Note: n (%) = frequency and percentage of participants who endorsed the item as being an existing or desired support. n (%) priority = frequency and percentage of participants who ranked the item as the top priority requiring attention. M = the mean ranking of each item.
Discussion
The objective of this study was to assess the perceived preparedness of Ontario’s LTC homes to meet the sexuality needs of LTC residents, as well as identify existing supports, barriers, and key priorities necessary to upholding residents’ rights to sexual expression, Study findings highlighted multiple barriers to sexual expression and sexuality-related concerns were reported by a majority (85%) of participants/settings. Similar to findings from other North American studies (i.e., Lester et al., Reference Lester, Kohen, Stefanacci and Feuerman2016; Shuttleworth et al., Reference Shuttleworth, Russell, Weerakoon and Dune2010), Ontario’s LTC homes lack clear policies guiding staff responses to residents’ expressions of sexuality and very few regularly assess or address sexuality-related concerns upon admission. On the positive side, a majority of LTC administrators reported positive and permissive attitudes about older adults’ sexuality and topics related to dementia and sexuality. As positive attitudes are related to creating a more positive environment regarding sexuality (Bentrott, Reference Bentrott2012), these results may be indicative of willingness to adapt current LTC practices to the baby boomer generation.
Settings with written policies tended to be situated in urban settings, have a spiritual or religious affiliation, and include assessment of sexuality-related issues during admission. This aligns with findings from Lee and Quam (Reference Lee and Quam2013) that sexual minority elders in urban settings tend to be more open about their sexual orientation as compared to their rural counterparts. Finally, considering the strong influence of religion on norms for sexual behaviour, informing not only when sex is appropriate but also how and with whom one may engage (Iveniuk & O’Muircheartaigh, Reference Iveniuk and O’Muircheartaigh2016), it is possible that religiously affiliated LTC homes are more likely to emphasize policies that affirm their own sexuality-related values and beliefs than their non-religious counterparts.
Existing policies regarding sexuality in LTC appear to be largely aspirational at this point. While both the LTCHA and its recent successor, the FLTCA, acknowledge residents’ right to privacy, in practice, implementation often falls short. For example, residents commonly share rooms and staff access may be prioritized over providing private space (Frankowski & Clark, Reference Frankowski and Clark2009; Howard et al., Reference Howard, Brassolotto and Manduca-Barone2020). The translation of general policy into respectful practice is a complex issue and may be applied variably across settings. In this study, LTC administrators identified existing legislation (i.e., the LTCHA) as the most pressing barrier requiring attention, both presently and in the future. Developing clear standards and guidelines could facilitate residents’ rights to express sexuality and provide them with the freedom to choose the time and setting (Iveniuk & O’Muurcheartaigh, Reference Iveniuk and O’Muircheartaigh2016).
Thirty-seven percent of settings have policies pertaining to some aspects of residents’ sexuality. However, such policies focus predominately on challenges that may have legal and ethical ramifications for LTC homes, such as the assessment of capacity to consent, residents’ rights to privacy, and the response to instances of sexual abuse or harassment. Very few provide explicit information on balancing support for residents’ sexuality needs with safeguards to prevent negative outcomes. Moreover, guidelines relevant to the accommodation of residents’ diverse sexuality needs, such as the provision of training for care staff (e.g., gender and sexual diversity, sexuality, and aging), inclusivity practices, and management of sexually transmitted infections (STIs), are conspicuously absent. Previous research suggests that in the absence of clear guidelines, decisions regarding residents’ sexuality may be made inconsistently. Staff responses may be informed by personal values and attitudes, and when cognitive decline is present, risk restriction may be prioritized over respecting residents’ autonomy and quality of life (Di Napoli et al., Reference Di Napoli, Breland and Allen2013). Researchers have highlighted various staff reactions in the presence of cognitive decline, ranging from ignoring sexuality needs and behaviours to implementing restrictive measures and admonishing residents for sexually expressive behaviour (Villar et al., Reference Villar, Celdrán, Serrat, Fabà and Martinez2018).
Older adults may present with a variety of sexuality-related concerns, ranging from accessing sexual aids (e.g., condoms, lubricants, sex toys, medication to treat age-related sexual dysfunction) to more complex matters such as facilitation of sex for persons with ability issues or accessing adequate healthcare for transgender persons. Restrictive and paternalistic responses will discourage residents from being proactive. Further, in the context of rising numbers of STIs among older adults (Centre for Communicable Diseases and Infection Control, 2017), an ad hoc approach to managing residents’ sexuality will not be sufficient. Current policies must be updated to reflect residents’ changing needs. Such guidelines should include specific information regarding how to foster an inclusive, sex positive, and safe environment, and assist residents who need help accessing sexual aids or preparing for sexual expression.
Enhanced knowledge of later-life sexuality at all levels of care is essential for fostering open communication about sexuality needs and recognizing problematic sexual situations (e.g., harassment, consent issues). Yet, when asked to reflect on their own ability to respond to residents’ sexuality, LTC administrators were not assured of their competence. Nearly half evaluated their sexuality-related knowledge as insufficient and a majority considered their level of training to be inadequate. Previous research has identified a relationship between perceived adequacy of sexuality-related knowledge and training, and staff responses. Mellor et al. (Reference Mellor, Greenfield, Dowswell, Sheppard, Quinn and McManus2013) found that health professionals who perceived themselves to have limited knowledge were more likely to consider sexuality-related issues to be beyond their scope of practice. In other studies, health care staff were hesitant to initiate conversations regarding sexuality due to discomfort with the topic, a perceived lack of knowledge or training, or a belief that sexuality was outside of their responsibility (Haesler et al., Reference Haesler, Bauer and Fetherstonhaugh2016; Hayward et al., Reference Hayward, Robertson and Knight2013). These findings reinforce the assertion that training should not only emphasize knowledge acquisition but also increase comfort and confidence in dealing with older adults’ sexual health related issues. Such training is particularly relevant for LTC administrators, given that they are uniquely positioned to influence workplace culture through the modelling of sex-positive attitudes and the implementation of facility-level procedures that are respectful and supportive of residents’ diverse sexuality needs.
While previous findings indicate that attitudes towards later-life sexuality vary widely among health care professionals, our results align with findings that LTC professionals in supervisory positions report relatively positive and permissive attitudes (e.g., Bouman et al., Reference Bouman, Arcelus and Benbow2007). Factors associated with more positive attitudes in this study included having more work experience and prior training. Research has consistently demonstrated that access to sexuality-related training, even interventions of relatively short duration, is generally predictive of more permissive attitudes (e.g., Bauer et al., Reference Bauer, McAuliffe, Nay and Chenco2012, Reference Bauer, Fetherstonhaugh, Tarzia, Nay, Wellman and Beattie2013). Our findings were no different; however, it should be noted that while training significantly predicted permissiveness on its own, experience in LTC did not. This finding is not surprising given that more experience working with older people has previously been associated with both more permissive (Bouman et al., Reference Bouman, Arcelus and Benbow2007) and more restrictive sexual attitudes (Di Napoli et al., Reference Di Napoli, Breland and Allen2013). Moreover, Helmes and Chapman (Reference Helmes and Chapman2012) found that no participant characteristics were significant in predicting sexuality-related attitudes. Taken together, these findings suggest that, except for training, our understanding of the impact of personal characteristics on sexual attitudes is not well understood and therefore warrants further investigation.
In the context of cognitive decline, no participant characteristics were found to predict attitudes towards later-life sexuality. Inspection of responses to the SAID survey indicated that when expressions of sexuality among persons with dementia diverged from traditional norms (e.g., married resident having sex with another resident, multiple partners), or went against family members’ wishes, respondents’ attitudes tended to be more negative and restrictive. This may imply that LTC administrators find it particularly challenging to make decisions about the appropriateness of sexually expressive behaviours that could result in negative ramifications for their facility (e.g., displeasing family members, legal, ethical consequences). In fact, family interference and difficulty assessing capacity to consent were two of the most commonly noted barriers to residents’ sexual expression reported in this study. To mitigate this, educational interventions recognizing respect and autonomy in the context of care needs and acknowledging the complexity of diversity and changing attitudes regarding relationships (e.g., polyamory, non-monogamy, open relationships) would be important as future cohorts of LTC residents are expected to be more varied in their expressions of sexuality.
When asked explicitly regarding their perception of barriers to residents’ sexual expression, LTC administrators identified several current and anticipated future barriers. Assessing capacity to consent, accessing private space, family interference, and staff education/training topped the list of existing barriers. Interestingly, while respondents recognized the lack of staff training as a current problem, responses indicate that they anticipated this problem may be exacerbated in the future. This makes sense when viewed in the context of younger baby boomers with more liberal sexual attitudes moving to LTC and the specific staffing challenges in LTC. Unregulated care workers (e.g., Personal Support Workers, Nursing Assistants), with comparatively less formal training and professional organizational oversight, are increasingly providing the direct care work that was once carried out by nursing staff in Canada (Afzal et al., Reference Afzal, Stolee, Heckman, Boscart and Sanyal2018) and internationally, across a wide range of healthcare settings (Blay & Roche, Reference Blay and Roche2020; Roche et al., Reference Roche, Friedman, Duffield, Twigg and Cook2017).
LTC administrators reported few existing supports specific to residents’ expressions of sexuality; 75% of respondents indicated that their home provided residents with ongoing opportunities to socialize. However, socialization was communal; only 37% of respondents indicated that residents have access to private space. Not surprisingly, respondents recognized the need for privacy and identified this as one of the most pressing issues requiring priority attention. Even fewer existing supports were reported regarding gender and sexual minorities. The most commonly cited support, endorsed by 9% of respondents, was the provision of inclusivity training for staff. Only 5% of respondents believed that their LTC home provided a welcoming environment and a mere 3% indicated inclusive language was used in facility documents. Given this reality, it is perhaps not surprising that 57% of respondents endorsed inclusivity training as one of their most desired supports. While there have been advances made in recent years to promote the health and well-being of sexual minorities and address gaps in culturally competent care for gender and sexually diverse persons, these findings highlight that much more work is needed to prepare Canadian LTC homes to meet the needs of these populations.
Overall, study findings suggest that Ontario’s LTC administrators/Directors of Care are highly cognizant of issues pertaining to residents’ sexuality, yet they lack confidence in their own ability to respond to older adults’ changing sexuality needs and expectations. They are provided with few supports and guidelines to help navigate the complexity and diversity of older adults’ sexuality within the LTC setting. As a result, the majority believe that their LTC home is currently unprepared to meet the sexuality and intimacy needs and expectations of the next generation of LTC residents. In fact, analysis of pre and post survey responses indicates that LTC administrators demonstrated even less certainty after completing our study.
Limitations
There are limitations associated with this study that should be noted. Although our findings align with previous studies that indicate that LTC administrators generally report permissive sexual attitudes, selection bias may affect the results of this study. Given that participation was voluntary, it is possible that only those with more liberal attitudes towards later-life sexuality participated in the study and the perspectives and experiences of more conservative LTC staff are excluded from this sample. The lack of an existing measure to assess LTC professionals’ experiences and perceptions regarding residents’ sexuality made it necessary to develop some additional survey items. Despite our attempt to mitigate problems by having stakeholders review and provide feedback, non-validated survey items may be subject to measurement error (e.g., question order effects). The effect sizes of the results from quantitative measures in this study were small. It is likely that there are additional factors affecting sexual attitudes and knowledge that were not captured in the current study. In addition, stakeholder feedback regarding time to complete the survey prompted us to shorten it; consequently, an objective measure of participants’ aging sexual knowledge (i.e., ASKAS aging sexual knowledge subscale) cannot be determined from the findings.
Study implications and future research
The findings of this study provide an important first snapshot of institutional barriers and support to residents’ sexual expression in a diverse sample of Ontario LTC homes. At this time, LTC settings appear to be in the trenches of adjusting to the changing sexuality needs of baby boomers. Generally, the leadership of LTC homes in Ontario appears motivated to move forward with perspective, respect, and positivity. However, existing policies are lacking in detail and specific direction. As a result, challenges to developing and implementing operational policies in LTC homes continue to rest with individual facilities and substantive training needs for LTC professionals remain unmet. These findings, together with previous research on challenges to sexual expression in LTC homes (e.g., Schubert & Pope, Reference Schubert and Pope2020; Syme et al., Reference Syme, Lichtenberg and Moye2016; Villar et al., Reference Villar, Celdrán, Fabà and Serrat2014), should be used to inform further research and to develop collaborative initiatives with a broader contingent of stakeholders to ascertain their perspectives on the priorities that have been identified herewith. Given the complexity of this issue, active collaboration among stakeholders at all levels, including policy advisors and compliance officers, LTC executives and staff, aged care associations (e.g. OLTCA), advocates, researchers, and current and future LTC residents, is imperative.
As Syme et al. (Reference Syme, Lichtenberg and Moye2016) point out, existing tools developed by consulting experts and working groups can serve as a foundation for developing more targeted guidelines that can be adapted to meet the diverse sexuality needs of LTC residents. Of note, two such recent initiatives are the National Standards of Canada for LTC published by the Canadian Standards Association Group (2022) and the Health Standards Organization (2023). These complimentary standards address various topics including aspects of LTC home design and operation, safety practices, and the provision of evidence-based and resident-centered care. While the scope of the standards is broad, the inclusion of benchmarks pertaining to sexual expression management, the accommodation of residents’ sexual health and intimacy needs, and gender and sexual inclusivity is very promising.
Finally, the development and ongoing provision of sexual management education and inclusivity training for LTC staff at all levels must be prioritized. Effective leadership in LTC is more vital now than it ever was. LTC administrators are uniquely positioned to promote and support residents’ sexuality and advocate for sex-affirming policies. However, they must do so while navigating organizational needs in a space that functions as both a home and a workspace. This will not be an easy feat; relevant and discerning training tailored to specific professional roles and responsibilities will be necessary. LTC administrators themselves will require a specific set of skills including the ability to assert positive influence and challenge outdated sexual beliefs and a historically patronizing approach towards sexual expression. In order to inform this process, additional research investigating the relationship between leadership characteristics, aging sexual knowledge and attitudes, and procedural outcomes is indicated.
Competing interest
The authors have no conflict of interest to disclose.











