Introduction
Chondrodysplasia punctata is a rare disorder characterised by midface hypoplasia, abnormal cartilage calcification, and brachytelephalangism, which is occasionally complicated by CHD, including peripheral pulmonary artery stenosis. Reference Fourie1 The degree of stenosis varies, Reference Cancela, Laizé, Conceição, Kempfe and Murshed2 and severe bilateral peripheral pulmonary artery stenoses can result in a fatal course. Reference Trowitzsch, Richter, Eisenberg and Kallferz3 There are no reports detailing the course of treatment of peripheral pulmonary artery stenosis. Herein, we report a case of a 2-month-old girl with chondrodysplasia punctata who underwent successful transcatheter balloon angioplasty for bilateral peripheral pulmonary artery stenoses.
Case report
The present female patient was born at 41 weeks of gestation with a birth weight of 3,230 g. The Apgar scores at 1 and 5 minutes were 5 and 8 points, respectively. External malformations were present, including a low nose bridge, short thumbs, and a continuous murmur of Levine grade 3/6 heard at the left upper sternal border. Cyanosis was present due to nasal narrowing, and the percutaneous arterial oxygen saturation was 87% during sleep. Echocardiography revealed bilateral stenoses in the segments distal to the pulmonary artery bifurcation, and the blood flow velocity measured using continuous-wave Doppler was 3.3 m/s at the stenotic sites. The short-axis of left ventricle view showed the shape of the interventricular septum was flat. The foramen ovale was patent with a left-to-right shunt. We diagnosed peripheral pulmonary artery stenosis as the cause of the heart murmur and started follow-up.
Whole-body skeletal X-rays and MRI of the head and neck were performed as a survey for systemic diseases. The X-rays revealed abnormal punctate calcification in multiple bones and cartilage as well as shortened distal phalanges, suggesting a diagnosis of chondrodysplasia punctata. MRI of the neck revealed stenosis of the cervical spinal cord due to atlantoaxial hypoplasia, and the patient was placed in a cervical collar to prevent injury to the spinal cord (Supplementary Figure S1).
Genetic testing was performed after informed consent was obtained from the patient’s parents. The Sanger method was used to search for loss-of-function mutations in the gene encoding the matrix Gla protein that is responsible for the aetiology of Keutel syndrome, which is included in chondrodysplasia punctata and is associated with peripheral pulmonary artery stenosis. No pathogenic variants were detected, and the parents declined to provide consent for further genetic testing.
At approximately one month of age, the patient presented with tachycardia and tachypnoea. The patient was treated with high-flow nasal cannula therapy (6 L/min, FiO2:0.21) for nasal narrowing, and the percutaneous arterial oxygen saturation was 97% at this time. Echocardiography at the age of 55 days revealed progression of peripheral pulmonary artery stenoses, and blood flow velocity measured by continuous-wave Doppler was 4.0 m/s at bilateral stenotic sites. The short-axis ventricle view showed a “D”-shaped left ventricle, which is characteristic of severe right ventricular pressure overload (Figure 1). The foramen ovale was narrowing. The left ventricle end-diastolic diameter was 15.2 mm, which is 73% of the normal diameter based on body surface area.
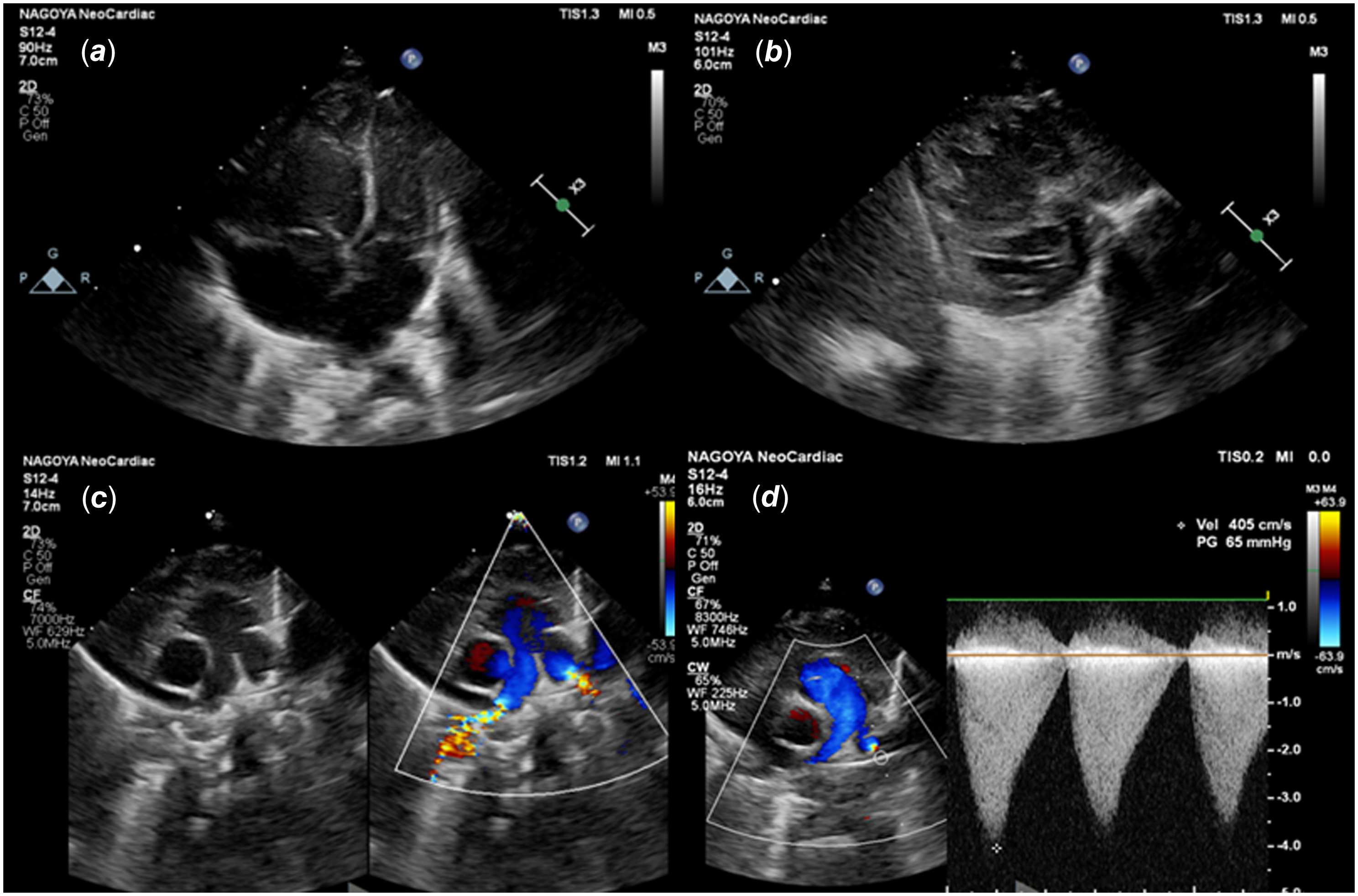
Figure 1. Echocardiographic findings prior to the intervention. (a) Four-chamber view shows dilation of the right ventricle. (b) LV short-axis view shows flattening of the interventricular septum and a “D”-shaped left ventricle. (c) Severe stenoses distal to the bilateral pulmonary artery (PA) bifurcation. (d) Blood flow velocity at the stenotic site in the left PA is 4.0 m/s.
We determined that the tachycardia and tachypnoea are symptoms of low cardiac output syndrome due to the progression of pulmonary artery stenoses and reduced preload to the left ventricular system. Therefore, cardiac catheterisation was performed under general anaesthesia at age 64 days. Intubation was performed under the guidance of a bronchial fibrescope to avoid the risk of spinal cord injury in head-tilt/chin-lift intubation. The right ventricle/left ventricle pressure ratio was 1.20. Pulmonary angiography revealed severe constriction of bilateral pulmonary arteries distal to the bifurcation, and the stenoses were localised. The narrowest diameters of the right and left pulmonary arteries were 1.3 mm and 1.1 mm, respectively. The distal reference diameters of the right and left pulmonary arteries were 3.8 mm and 3.7 mm, respectively (Figure 2). Pressure gradients of 40 mmHg or more were observed in the narrowest portions of both pulmonary arteries. Considering the patient’s general condition, balloon angioplasty was selected as the least invasive treatment method. Stent implantation was also a potential treatment option, but because the patient was still small, we considered it a second choice, given the patient’s future physical growth in stature.
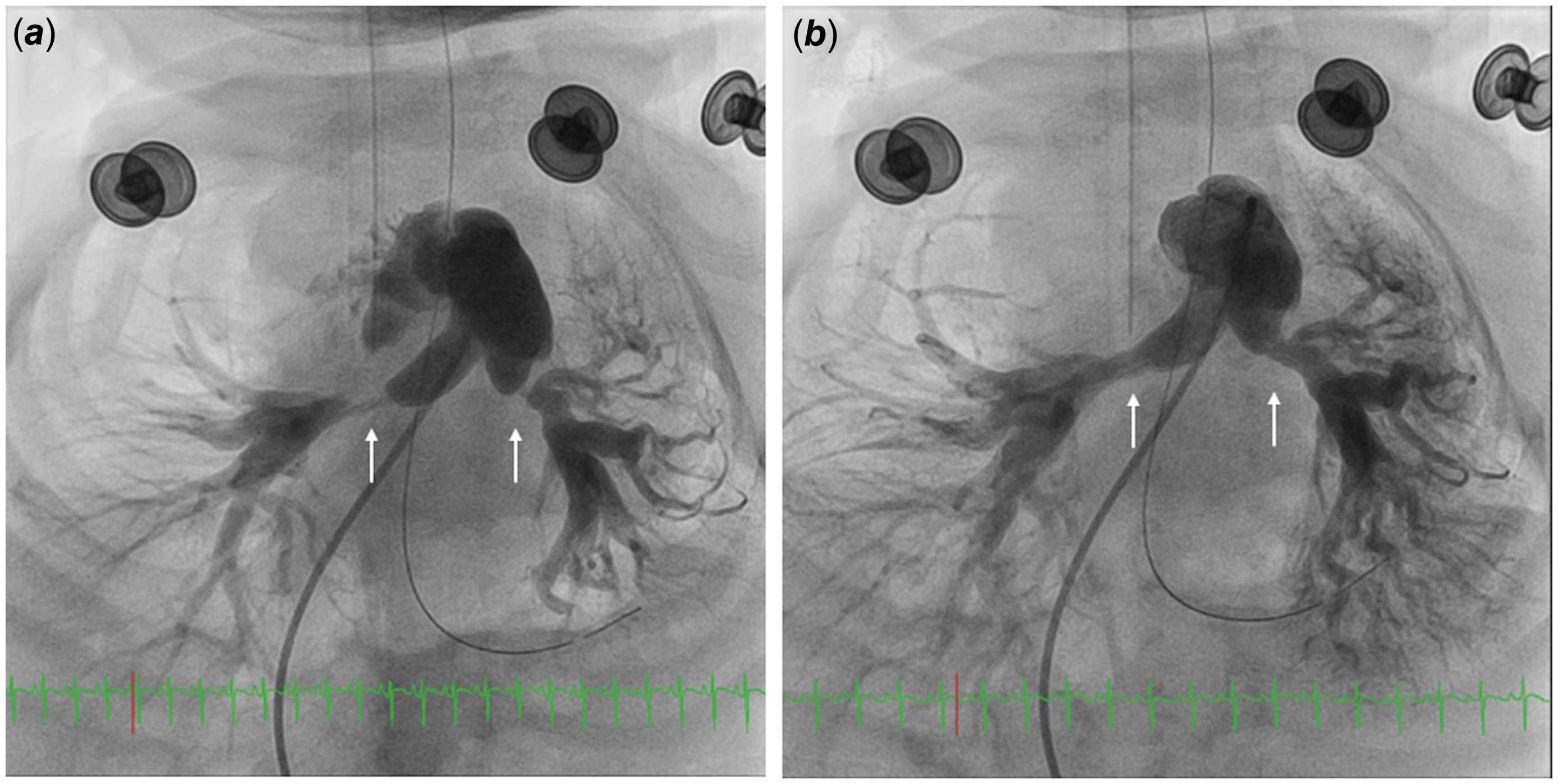
Figure 2. Pulmonary angiograms demonstrate the severity of stenoses before BAP and the improvement after BAP. White arrows indicate the stenotic sites.(a) The diameters of the right and left pulmonary arteries at the stenotic sites are 1.3 mm and 1.1 mm, respectively. The distal reference diameters of the right and left pulmonary arteries are 3.8 mm and 3.7 mm, respectively. (b) After BAP, the diameters expand to 3.9 mm and 3.6 mm in the right and left pulmonary arteries, respectively. BAP = Balloon angioplasty.
Despite initial dilation using a CoyoteTM OTW 2.0 mm balloon dilation catheter (Boston Scientific Corporation, Natick, MA, USA) at 14 atm, bilateral pulmonary artery stenoses persisted. Subsequent dilation with a 4.0 mm Sterling balloon dilation catheter (Boston Scientific Corporation) at 14 atm for 40–60 s monitoring the systemic blood pressure resulted in sufficient dilation of the stenoses. After balloon angioplasty, the right ventricle/left ventricle pressure ratio dropped from 1.20 to 0.58 and the symptoms of heart failure observed prior to the intervention improved. At 12 months after the procedure, no restenosis of the peripheral pulmonary arteries was observed.
Discussion
In the present case, balloon angioplasty was effective for severe bilateral peripheral pulmonary artery stenosis associated with chondrodysplasia punctata. There are no detailed reports on balloon angioplasty for peripheral pulmonary artery stenosis in patients with chondrodysplasia punctata; the present case suggests that balloon angioplasty may be a suitable therapeutic option.
Severe isolated peripheral pulmonary artery stenosis is associated with several systemic diseases including Williams syndrome and Alagille syndrome. Reference Allen, Driscall, Shaddy and Feltes4 Peripheral pulmonary artery stenosis also occurs in some patients with chondrodysplasia punctata, Reference Fourie1 which is a rare group of diseases of skeletal dysplasia that include X-linked dominant chondrodysplasia Conradi-H FC;nermann type (CDPX2) and Keutel syndrome. Keutel syndrome is a rare autosomal recessive type of chondrodysplasia punctata with estimated prevalence of 1 in 1,000,000 births, almost all of which are associated with peripheral pulmonary artery stenosis. Reference Cancela, Laizé, Conceição, Kempfe and Murshed2 There are two case reports of CDPX2 complicated by peripheral pulmonary artery stenosis, one of which describes severe peripheral pulmonary artery stenosis in a patient who died six months after birth. Reference Trowitzsch, Richter, Eisenberg and Kallferz3 Although some adult cases of both syndromes have been reported, the natural history and optimal treatment of associated peripheral pulmonary artery stenosis remains unclear. Reference Khosroshahi, Sahin, Akyuz and Ede5,Reference Posey, Burrage and Campeau6
Peripheral pulmonary artery stenosis requires treatment in cases of severe bilateral or multiple stenoses leading to right ventricle pressure overload. The treatment options for peripheral pulmonary artery stenosis include both surgical repair and catheter intervention including balloon angioplasty and stent implantation. In our case, the initial balloon angioplasty was quite effective for peripheral pulmonary artery stenosis, and the restenosis has not occurred thereafter. Peripheral pulmonary artery stenosis is also associated with other systemic diseases such as Williams syndrome, it has been reported that the effectiveness of initial balloon angioplasty is approximately 50% and restenosis is frequently observed in Williams syndrome. Reference Geggel, Gauvreau and Lock7 The arteries in Williams syndrome are histologically characterised by diffuse wall thickening consisting of intimal proliferation and medial dysplasia with hypertrophy, fibrosis, and nonparallel mosaic arrangement of smooth muscle cells. Reference Zalzstein, Moes and Musewe8 These histological characteristics have been considered the basis for less successful pulmonary artery dilation in this syndrome. Although histological examination of the PAs was not performed in our patient, concentric arterial calcification in the area of the internal elastic plate of the PAs has been reported in patients with Keutel syndrome among chondrodysplasia punctata. Reference Cranenburg, Van Spaendonck-Zwarts and Bonafe9 These differences in histological characteristics may contribute to the contrasting efficacy of balloon angioplasty and restenosis rates between chondrodysplasia punctata and Williams syndrome. For severe and stiff pulmonary artery stenosis, sufficient dilation cannot often be achieved unless a non-compliant balloon is used. In our case, effective dilation was achieved using a semi-compliant balloon. This phenomenon also suggests that pulmonary artery stenosis in chondrodysplasia punctata is easily dilated by balloon angioplasty histologically. In Williams syndrome, diffuse stenoses involving large segments of the pulmonary arterial tree are frequently encountered, Reference Collins10 whereas in our case, the stenoses were short and limited to the bifurcations of the pulmonary arteries. The short extent of the stenosis may have contributed to the effectiveness of balloon angioplasty.
Because the general condition of the present patient was poor, we selected balloon angioplasty as a minimally invasive treatment. As the histological characteristics of the pulmonary artery in chondrodysplasia punctata and the risk of rupture and aneurysm formation were unknown. Therefore, we first performed dilation with a small-size balloon, followed by dilation with a balloon of approximately the same size as the reference pulmonary artery diameter. This allowed for effective dilation without vascular injury. Based on this case, a balloon with a size that is 3–3.5 times the diameter of the stenosis and is the same size as the reference artery can probably be used safely for dilation of peripheral pulmonary artery stenosis in chondrodysplasia punctata. Furthermore, we devised an intubation method for general anaesthesia that took into consideration the risk of injury to the spinal cord due to the instability of the cervical spine. Specifically, we avoided neck extension for intubation and performed the intubation under bronchial fibrescope guidance.
Based on the clinical course of our case, balloon angioplasty could be an effective treatment option for peripheral pulmonary artery stenosis associated with chondrodysplasia punctata. However, careful and long-term observation of restenosis is necessary, as long-term outcomes remain unknown and the specific histopathological findings of pulmonary artery stenosis in chondrodysplasia punctata are lacking. An accumulation of cases and pathological findings of peripheral pulmonary artery stenosis in chondrodysplasia punctata is necessary to clarify the long-term prognosis and optimal treatment for this condition.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1047951124036229.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Competing interests
All authors declare that they have no conflicts of interest to report regarding the present study.
Ethical standard
This report was conducted in accordance with the principles of the Declaration of Helsinki and the ethical guidelines issued by the Ministry of Health, Labour, and Welfare, Japan. Written informed consent for publication of this report was obtained from the patient’s parents.





