The bidirectional cavopulmonary shunt (the Glenn procedure) is the second of three-staged surgical procedures that have been utilised for palliating children with single ventricular anatomy and other complex CHDs. Reference Hopkins, Armstrong, Serwer, Peterson and Oldham1–Reference Petrucci, Khoury, Manning and Eghtesady5 Used prior to the total cavopulmonary connection (the Fontan procedure), the Glenn procedure has improved overall outcomes in these children. Reference Masuda, Kado and Shiokawa6,Reference Bridges, Jonas and Mayer7 While the mortality and failure rate for this interstage procedure is low, Reference Carlo, Carbery and Heinle8–Reference Alsoufi, Manlhiot and Awan13 there exists enough mortality and morbidity that risk factors should be delineated.
Previous researchers have identified possible risk factors associated with Glenn failure: ventricular dysfunction, atrioventricular valvular regurgitation (AVVR), elevated mean pulmonary artery pressure, elevated transpulmonary gradient, and heterotaxy. Reference Carlo, Carbery and Heinle8–Reference Alejos, Williams and Jarmakani15 This existing literature is limited by the lack of systematic long-term follow-up and assessment of potential risk factors for late adverse outcomes. Through the Western Canadian Complex Pediatric Therapies Follow-up Program (CPTFP) registry, we have a high rate of long-term follow-up (to age 2 years to determine detailed neurodevelopmental and functional outcomes) in survivors. Reference Robertson, Sauve and Joffe16 We aimed to report the experience of the CPTFP with the Glenn procedure done in infants with single ventricles during a recent surgical era. We hypothesised that there would be potentially modifiable risk factors for a complicated post-Glenn course. We also hypothesised that a complicated post-Glenn course would be an independent predictor of adverse neurodevelopmental and functional outcomes at age 2 years. The results were anticipated to inform timely intervention for patients to prevent a complicated Glenn course and thus lead to better decision-making to reduce morbidity and mortality.
Materials and methods
Study design
This was a prospective inception-cohort study that included all consecutive patients having the Glenn procedure at the Stollery Children’s Hospital (Edmonton, Alberta, Canada) from January 2012 to December 2017. The Stollery Children’s Hospital is a Western Canadian referral centre for complex paediatric cardiac surgery for multiple tertiary referral sites. Patients were identified at the time of complex cardiac surgery at which point consent was obtained and they were recruited for inclusion into the CPFTP registry. This study was approved by our university research ethics board (Pro00001030). Previously agreed upon demographic, pre-operative, intra-operative, and post-operative variables were collected prospectively. Reference Robertson, Sauve and Joffe16 Pre-operative anatomy and haemodynamic assessments were conducted using pre-operative echocardiogram and either pre-operative catheterisation or cardiac MRI. Use of catheterisation versus cardiac MRI was largely dependent on the referral centre. Long-term follow-up was performed at 2 years of age at one of the tertiary sites of origin. Follow-up at age 2 years was used to allow enough time for recovery after the Glenn procedure (and at least 6 months after any surgical procedure), but before the Fontan procedure. The follow-up study and database have been approved by each respective institutional health research ethics board.
Variables and definitions
Variables previously agreed upon had been collected prospectively in the CPTFP Registry (eTables 1 and 2). Additional pre-specified variables were collected by retrospective chart review: need for Glenn take down, cardiac catheterisation or cardiac MRI data (whichever was performed and allowed determination of ratio of pulmonary to systemic blood flow [Qp/Qs], presence of pulmonary artery [PA] or vein [PV] obstruction, or presence of restrictive atrial septal defect), pre-Glenn echocardiogram (ECHO) data (to assess for presence of at least moderate AVVR or at least moderate systemic ventricular dysfunction), presence of significant residual lesions on post-Glenn ECHO (defined as at least moderate ventricular dysfunction, at least moderate AVVR, decompressing collateral vessel(s), or residual anatomic obstruction [of PA, PV, or aortic arch]). Each finding was recorded as on the cardiac catheterisation, MRI, and ECHO report.
We defined a complicated Glenn Procedure (cGP) as any one of i) death by age 2 years, ii) cardiac transplant by age 2 years, iii) need for extracorporeal life support (ECLS, i.e., extracorporeal membrane oxygenation [ECMO] or ventricular assist device) during the Glenn hospitalisation, iv) need for Glenn take down during the hospitalisation, or v) prolonged mechanical ventilation after the Glenn procedure (defined as ≥90th percentile of post-operative ventilation duration in the cohort). There is no consistent definition of a cGP in the literature; the components used were decided by consensus of the authors to reflect what we believe clinicians and parents would want to know regarding an in-hospital complicated course (i.e., Glenn takedown, prolonged ventilation days, death, ECLS, transplant) and 2-year severe complications (i.e., death, transplant).
Certified paediatric psychologists obtained the results of the Adaptive Behavior Assessment System, 2nd Edition (ABAS-II) in the patient’s respective referral institutions. Adaptive functional outcomes were determined by the General Adaptive Composite (GAC) score from the ABAS-II. The GAC has a normative population mean of 100 and standard deviation (SD) of 15; higher scores indicate better performance, a score <85 is 1 SD below the mean (expected in 15.9% of the normative population), and a score <70 is 2 SD below the mean (expected in 2.27% of the normative population). Reference Harrison and Oakland17
Certified paediatric psychologists and psychometrists administered the Bayley Scales of Infant and Toddler Development-3rd Edition (Bayley-III) in their respective referral institutions. Corrected age was used up to 2 years as recommended. The Cognitive Scale includes non-verbal activities involving memory, problem solving, and manipulation of the physical world. The Language Scale includes Receptive and Expressive Communication subtests. The Motor Scale includes a Fine Motor (e.g., visual–motor integration, visual–spatial, and motor control skills in the hands) and Gross Motor (e.g., large body movements, mobility, and complex movements) subtests. The population norm score on these scales is 100, with SD 15. 18
Statistical analysis
We described variables and outcomes using proportions (percentages) for categorical variables and mean (SD) or median [interquartile range, IQR] for continuous variables.
The primary outcome was prediction of a cGP. Cox regression for univariate associations was performed for all predictor variables in eTables 1 and 2. A multiple Cox regression model was done including all variables with p-value <0.05 on univariate analysis, and after screening for multicollinearity. Associations are presented as Hazard Ratios (HR) with 95% confidence intervals (CI) and two-sided p-values. The potential predictor variables for a cGP were determined a priori. These included demographic, pre-operative, intra-operative, and day 1 post-operative (i.e., on day of operation) variables, and certain post-operative variables that occurred in at least 5% of patients, specifically the use of iNO and residual anatomic cardiac abnormalities (see eTables 1 and 2). Inotrope score post-operative day 1 and iNO use post-operatively were variables included that aimed to reflect clinician therapy in response to deteriorating patient condition.
We considered that clinicians and parents would want to know if survival after a cGP may be associated with adverse neurodevelopmental and functional outcomes. The secondary outcome was thus whether a cGP was an independent predictor of adverse neurodevelopmental and functional outcomes. Linear regression for univariate associations was performed for all predictor variables in eTables 1 and 2. All univariate variables with a p-value approaching significance at p ≤ 0.1 for association with the outcome were evaluated, after screening for multicollinearity, in a multiple variable linear regression model for each outcome. A priori we determined that two variables would be forced into each of these models, regardless of their univariate association: socioeconomic status (determined by the Blishen Index Reference Blishen, Carroll and Moore19 ) and cGP. Results are presented as effect sizes (ES) with 95% CI. A p-value <0.05 was used to determine statistical significance in the multivariable models.
We present results of univariate regressions that have a p-value ≤0.10, and of multiple variable regressions that have a p-value ≤0.05 or that were pre-specified to be forced into the regressions. Coefficients (effect sizes) and Hazard Ratios that have higher p-values are not presented because, given low prior probabilities in this exploratory research, their posterior probability of being a true association would be very low and likely misleading. Reference Nostedt and Joffe20
Some analyses were done post-hoc (i.e., not pre-specified) after obtaining our results for primary and secondary outcomes and are therefore exploratory. These explored associations of some variables, based on the above multiple regression results, potentially suggest what was driving the findings. These are described in the supplemental methods.
Results
Description of the cohort
During the 6-year study period, 171 patients had a Glenn procedure. Patients whose charts were not available were excluded (n = 2). Demographic, anatomic, haemodynamic, and acute-care variables are shown in eTables 1 and 2. Variables significantly associated with the outcome are provided in Table 1.
Table 1. Descriptive variables of significance for two-year outcome in 169 children having the Glenn procedure.

CPR: cardiopulmonary resuscitation; DHCA: deep hypothermic circulatory arrest; ECMO: extracorporeal membrane oxygenation; PA: pulmonary artery.
Overall, pre-op catheterisations occurred in 93 (55%) patients, pre-operative cardiac MRI in 77 (46%), both MRI and catheterisation in 12 (7%), Computed Tomography (CT) chest with angiography and catheterisation in 1 (0.6%), and none (of catheterisation, cardiac MRI or CT) in 11 (6.5%). Also, 92 (54.4%) were male, 77 (46%) underwent a Norwood/Sano as their initial procedure, the median age at Glenn was 6.4 [2.8, 10] months, the median days of ventilation was 1 [0, 2] days, and the median length of hospital stay was 10 [7, 18] days. Four patients (2%) died within 30 days of the Glenn procedure (three of whom died during the Glenn procedure hospitalisation).
The outcomes in survivors are shown in eTable 3. Growth was within normal range, but 22% required the use of a G-tube. Survivors experienced several re-hospitalisations (mean 2, SD 3) and remained on pulmonary and cardiac medications (mean 2, SD 1.5) at 2 years of age.
Complicated Glenn procedure
Of the 169 patients, 27 (16%) met criteria for a cGP (Table 2). The reasons for being classified as a cGP are given in Table 2. The Kaplan–Meier curve for survival without meeting the definition of a cGP is shown in Figure 1.
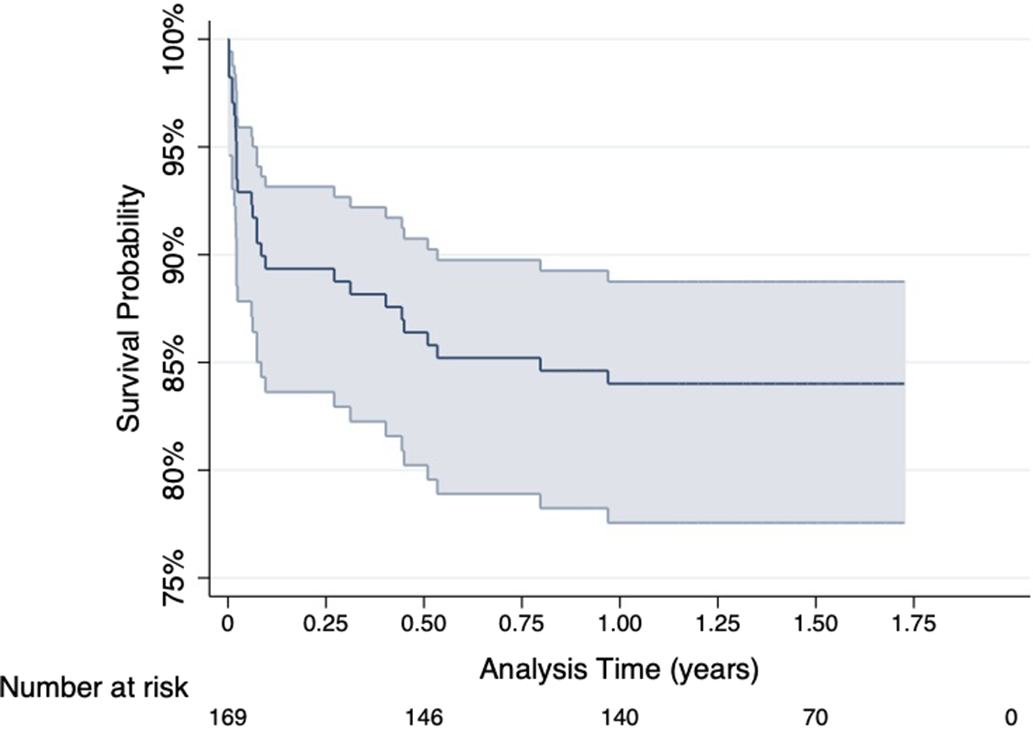
Figure 1. Kaplan-Meier Survival curve for survival without meeting the definition of a complicated Glenn Procedure. This curve shows the probability over time of survival without having a complicated Glenn procedure; at 2 years of age this probability was 84%.
Table 2. Description of components of the complicated Glenn procedure composite outcome.
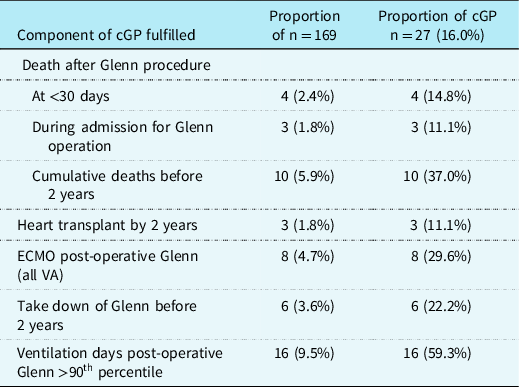
None had use of ventricular assist device used post-operative Glenn. Of Glenn takedowns, 0 had transplant or death; of ECMO post-operative Glenn, 1 had transplant, and 3 died.
cGP: complicated Glenn procedure; ECMO: extracorporeal membrane oxygenation; VA: veno-arterial.
Demographic, anatomic, and haemodynamic variables were compared between cGP and non-cGP patients. Results of univariate (for all variables from eTables 1 and 2 having a p-value ≤ 0.05) and multiple variable Cox regression are shown in Table 3. The inotrope score on post-operative day 1 (HR 1.04 (1.01, 1.06) p = 0.010) and use of iNO post-operatively (HR 7.31 (3.19, 16.76) p < 0.001) were associated with cGP. Post-hoc exploratory analyses for associations with the use of iNO and day 1 inotrope score are in the supplemental results and shown in eTable 4. Post-hoc exploratory analyses for association of highest CVP and a surrogate for transpulmonary gradient are in the supplemental results.
Table 3. Predictors on univariate and multiple-variable Cox regressions of a Complicated Glenn Procedure in 169 children.

Variables not statistically significant on univariate analysis included: maximum CVP d1-5; fluid balance d1; at least moderate AVVR on ECHO pre-operatively; PA obstruction or restrictive atrial septal defect on catheterization or MRI pre-operatively; residual at least moderate AVVR on ECHO post-operatively.
Variables statistically significant on univariate, but not included due to too few patients having the finding (<5% of cohort): two transfusions d1 (2.4%), positive blood culture sepsis (4.1%), CPR post-operatively (2.4%), dialysis post-operatively (2.4%), re-CPB during Glenn operation (4.7%), pre-operative ECHO at least moderate ventricular dysfunction (4.7%), residual PV obstruction on post-operative ECHO (2.4%), and re-opening of sternum post-operatively (4.1%). The lowest Qp:Qs pre-operatively was only available in 85 (60%) of non-cGP 1.02 (0.65) and 14 (52%) cGP 1.42 (2.07) for a univariate HR 1.45 (1.00, 2.09) p = 0.049.
cGP: complicated Glenn Procedure; CPB: cardiopulmonary bypass; ECHO: echocardiogram; ECMO: extra-corporeal membrane oxygenation; iNO: inhaled nitric oxide.
a Inotrope score calculated as: (100)(epinephrine + norepinephrine) + (dopamine + dobutamine) + (10)(milrinone), with each of the vasoactive agents dose in mcg/kg/min. Reference Martin, Jonker and Joffe30
b Additional procedures: aortic arch repair 13, ventriculo-arterial valve repair/replacement 11, atrio-ventricular valve repair/replacement 12, pulmonary artery plasty 45, atrial septectomy 21, pulmonary artery band removal 7, DKS 10, pulmonary band 2.
Neurodevelopmental and functional outcomes
Of the 159 patients who survived to 2 years, 3 refused follow-up, leaving 156 (98%) having full neurodevelopmental outcome assessments. Follow-up was done at a mean of 22.9 (SD 4.6) and median of 22 (IQR 20–24) months of age, in all cases prior to the Fontan operation. Neurodevelopmental and functional outcomes were within population norms, though shifted to the left. A delay in these scores (i.e., score < 70 is > 2SD below the population norms) occurred in 10–20% of survivors, higher than the expected 2.27% of the normative population (eTable 3).
The results of univariate (for all variables having a p-value approaching statistical significance, p ≤ 0.10) and multiple variable linear regression for each Bayley-III outcome are shown in Tables 4 and 5. A cGP was statistically significantly independently associated with adverse Bayley-III Cognitive (ES −10.60, 95% CI −17.09, −4.11; p = 0.002) and Language (ES −11.43, 95% CI −19.25, −3.60; p = 0.004) scores, but not with the Motor score. Other variables independently associated with better outcomes on at least two of the Bayley-III scores included higher socioeconomic status, fewer ventilator days at neonatal operation, use of deep hypothermic circulatory arrest (DHCA) at the Glenn procedure, and PA obstruction present prior to the Glenn operation.
Table 4. Univariate linear regressions for Bayley-III Scores in 156 children surviving to 2 years of age after having the Glenn procedure.

Of 169 patients included, 10 died by age 2 years, and 3 refused follow-up, giving 156 for these outcomes.
CPR: cardiopulmonary resuscitation; DHCA: deep hypothermic circulatory arrest; ECHO: echocardiogram; ECMO: extracorporeal membrane oxygenation; PA: pulmonary artery; PICU: pediatric ICU.
Table 5. Multiple variable linear regressions for Bayley-III Scores in 156 children surviving to 2 years of age after having the Glenn procedure.
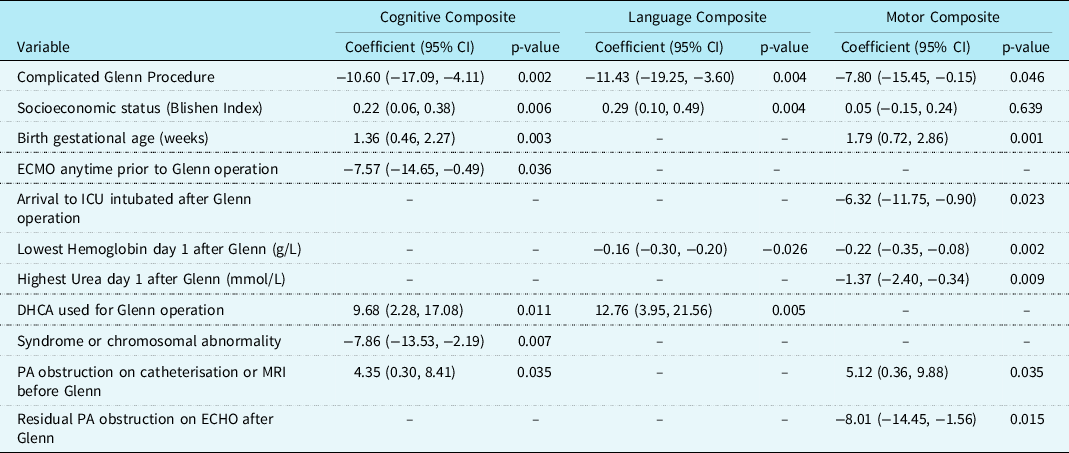
Of 169 patients included, 10 died by age 2 years, and 3 refused follow-up, giving 156 for these outcomes. Note that day 1 lowest haemoglobin after Glenn and day 1 lowest PaO2 after Glenn had low correlation of r = 0.10. In multiple variable linear regressions including only the n = 122 who had neonatal operation, ventilator days at neonatal operation was independently associated with Cognitive composite score (Coefficient −0.39 (95% CI −0.66, −0.12) p = 0.005) and Motor composite score (Coefficient −0.58 (−0.92, −0.24) p = 0.001), and CPR at time of neonatal operation was independently associated with Cognitive composite score (Coefficient −7.35 (−13.54, −1.17) p = 0.020).
CPR: cardiopulmonary resuscitation; DHCA: deep hypothermic circulatory arrest; ECHO: echocardiogram; PA: pulmonary artery.
The results of univariate (for all variables having a p-value ≤ 0.10) and multiple variable linear regression for the GAC score are shown in Table 6. A cGP was statistically significantly independently associated with adverse GAC score (ES −14.89, 95% CI −22.86, −6.92; p < 0.001). Other variables independently associated with adverse GAC score included longer ventilator days at the neonatal operation, cardiopulmonary resuscitation at the time of neonatal operation and having a chromosomal abnormality.
Table 6. Univariate and multiple variable linear regression for general adaptive composite score in 156 children surviving to 2 years of age after having the Glenn procedure.
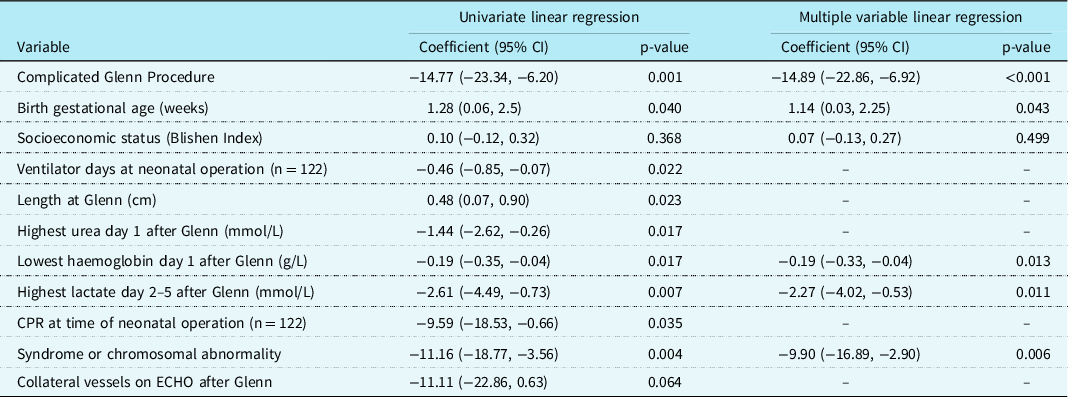
Of 169 patients included, 10 died by age 2 years, and 3 refused follow-up, giving 156 for these outcomes. In multiple variable linear regressions including only n = 122 who had neonatal operation, ventilator days at neonatal operation was independently associated with GAC (Coefficient −0.43 (−0.80, −0.06) p = 0.022), and CPR at time of neonatal operation was independently associated with GAC (coefficient −8.81 (−17.18, −0.44) p = 0.039).
CPR: cardiopulmonary resuscitation; ECHO: echocardiogram.
Discussion
We report the outcomes of 169 patients having a Glenn procedure at a Western Canadian referral centre for complex paediatric cardiac surgery over a recent 6-year period. The main findings of this study are highlighted. First, 27 (16%) patients met our definition of a cGP, including 10 (6%) who died by age 2 years. Second, higher inotrope score on the first post-operative day of the Glenn procedure and the use of iNO post-operatively were identified as independent risk factors for a cGP. Whether these predictors are modifiable requires future study. Third, a cGP was an independent predictor of adverse Bayley-III outcomes on cognitive and language scores and GAC outcome, with ES that were close to 1 SD of the population norms. In addition to the variables peri and post the Stage-1 surgery that impact long-term outcomes, Reference Ohye, Sleeper and Mahony21 these findings emphasise that events at the time of the Glenn procedure have the potential to impact these long-term outcomes as well. Indeed, the 14-month neurodevelopmental outcomes from the single ventricle reconstruction trial were deemed to be more dependent on the innate patient factors and patient morbidities in the first year than the specific Stage-1 operative strategies. Reference Newberger, Sleeper and Bellinger22 We describe here unrecognised morbidities and risk factors during the Glenn procedure that may contribute to these findings noted in the single ventricle reconstruction trial.
The early mortality after the Glenn procedure (defined as death <30 days after the Glenn procedure, rate of 2%) and rates of cGP (16%) in this study are comparable to those reported by other investigators. Reference Petrucci, Khoury, Manning and Eghtesady5–Reference Scheurer, Hill and Vasuki9,Reference Kogon, Plattner, Leong, Simsic, Kirshbom and Kanter11 In contrast to previous studies, some risk factors, including pre-operative ventricular dysfunction and AVVR, were not statistically significantly associated with a cGP outcome - potentially explainable by different definitions for a complicated post-Glenn course. Reference Reddy, McElhinney, Moore, Haas and Hanley4–Reference Kogon, Plattner, Leong, Simsic, Kirshbom and Kanter11 These risk factors were previously identified in populations with predominantly Hypoplastic Left Heart Syndrome (accounting for only 32.5% of the diagnoses in our population). In our population, 46% had a Norwood-Sano procedure as their first operation. Our institutional preference for the Norwood/Sano procedure (as opposed to the classical Norwood procedure) may mitigate some of these risks, as we previously reported a survival and neurodevelopmental benefit at age 2 years during the Sano era versus the modified BT shunt era at our institution, Reference Atallah, Dinu and Joffe23 which we acknowledge may differ from the experience of other centers. Reference Ohye, Sleeper and Mahony21
On univariate analysis, some variables that may be associated with these previously identified risk factors were associated with a cGP (Table 3), including severity of illness on the first post-operative day, existence of collateral vessels, and moderate to severe ventricular dysfunction on echocardiogram post-operatively. However, most of these variables were not independent predictors; only higher inotrope score on the first post-operative day and use of iNO post-operatively were statistically significantly associated with a cGP. Of note, higher inotrope score could relate to post-operative ventricular dysfunction. Also, identification of use of iNO has not been previously identified as a risk factor. Reference Carlo, Carbery and Heinle8–Reference Alejos, Williams and Jarmakani15
We do not have a protocol for starting nor weaning iNO. Inhaled nitric oxide was likely used by clinicians to manage refractory hypoxemia or low cardiac output; potentially to reduce elevated pulmonary vascular resistance and thus improve effective pulmonary blood flow. Many have reported a reduction in central venous pressure (i.e., Glenn pressure) and hence the transpulmonary pressure gradient with use of iNO in patients immediately after the Glenn procedure. Reference Agarwal, Churchwell and Doyle24–Reference Georgiev, Latcheva, Pilossoff, Lazarov and Mitev26 However, these physiological changes may not consistently translate to an improvement in systemic oxygenation - especially in patients with residual anatomic obstruction. Reference Adatia, Atz and Wessel27 The use of this therapy in the post-operative period may therefore indicate a failing circulation that, in the absence of other investigations and/or interventions, may confer risk for a cGP and the attendant neurodevelopment sequelae. This explanation is consistent with our finding of statistically significant associations between the use of iNO and post-operative day 1 and 2–5 lactates and PaO2, day 2–5 inotrope score, and number of transfusions on post-operative day 1. Similarly, the association of higher post-operative inotrope score with cGP likely reflects higher doses of vasoactive medications being used when there is a failing circulation resulting in hypoxia and low cardiac output. Again, this is consistent with our finding of statistically significant associations between day 1 inotrope score and post-operative day 1 and day 2–5 lactates and PaO2. Overall, we believe that the need for iNO post-operatively and/or higher inotropes should trigger important clinical decisions, including cardiac catheterisation, looking for potentially treatable residual lesions; this requires further study.
As far as we are aware, this is the first study to find a strong association between a cGP and adverse long-term neurodevelopmental and functional outcomes. The CPTFP achieved longitudinal follow-up to 2 years of age in 156/159 (98%) of survivors after a Glenn procedure. We were able to show that a cGP was a statistically significant independent predictor of adverse neurodevelopmental and functional outcomes as determined by the Bayley-III and GAC scores, with effect size being clinically significant (between ½ to 1 SD of the population norms of the scores). Only the motor score on Bayley-III was not statistically significantly associated with a cGP. These findings of adverse neurodevelopmental and functional outcomes may reflect the effects of hypoxia and low cardiac output that are components of the definition of a cGP: requiring heart transplant, extra-corporeal life support, Glenn take-down, or prolonged ventilation to achieve survival.
After multivariable logistic regression, DHCA used during the Glenn procedure was independently associated with higher Bayley-III Cognitive and Language scores. After multivariable logistic regression, the presence of pre-Glenn PA obstruction was unexpectedly independently associated with higher cognitive and motor scores on the Bayley-III. As we explored many relationships, it is possible that these associations with neurodevelopmental outcomes were false positives. In addition, the p-values for these findings can be considered only suggestive, and confirmation in future studies is required. Further discussion of these associations can be found in the supplemental discussion.
This study has limitations. First, this was a single centre study and may reflect local practice patterns and surgical techniques resulting in limited generalisability. Even so, during the period of this study, we had 4 paediatric cardiac surgeons operating and 11 cardiac intensivists; clinical practice was at their discretion. A second limitation is that some of the variables were collected retrospectively resulting in a risk of information bias. The retrospectively collected variables were objective measurements reported in the medical charts from cardiac catheterisation, echocardiogram, and MRI, potentially mitigating this limitation. In addition, we did not include some variables that may have improved prediction, including pulmonary artery pressures and detailed anatomic abnormalities (e.g., aortic atresia). A previous study by our group found no difference in Bayley-III scores at age 2 years between patients with HLHS and non-HLHS having a Norwood-Sano operation. Reference Martin, Jonker and Joffe30
This was an observational study and cannot prove cause and effect, and there may be unmeasured variables that confound the results. The findings should therefore be considered hypothesis generating and warrant confirmation, particularly the suggestion that inotrope score and use of iNO may be modifiable. Finally, a cGP is a composite outcome, and each component is not necessarily mutually exclusive (e.g., prolonged ventilation may occur in those requiring ECMO) nor temporally related. It is possible that some variables would predict one component and not another. Further, it is possible that certain components of the definition for a cGP (e.g., need for ECLS, transplantation, prolonged ventilation) may be independent risk factors for poor neurodevelopmental outcomes. Given the sample size, we did not explore these possibilities because we would likely obtain spurious findings due to multiple testing.
Strengths of this study include the large cohort, the prospective collection of most variables, and the very high rate of completed long-term follow-up. Further, we include variables across time, and were able to show that some variables associated with neurodevelopmental outcome reflect illness severity during the first surgery (i.e., ventilator days and need for cardiopulmonary resuscitation), chromosomal or syndromic diagnosis, and socioeconomic status of the parents, while others reflect severity of illness during the Glenn procedure. This emphasises that patients have exposure to many different risks over time and a focus on all potentially modifiable variables (e.g., improving social determinants of health) has the potential to improve long-term outcomes.
Conclusion
In 169 single ventricle patients having a Glenn procedure from a large Canadian cohort, higher inotrope score and iNO use post-operatively were independently statistically significantly associated with a cGP. Further study is required to explain the relationship of iNO use with cGP. In addition, a cGP was associated with adverse neurodevelopmental and functional outcomes at 2 years of age and should be added to the list of risk factors that increase the need for surveillance for adverse neurodevelopment. Reference Wernovsky and Licht31 Whether earlier identification of patients at risk for a cGP can allow interventions, such as early post-operative cardiac catheterisation, that prevent long-term morbidity and mortality warrants further study.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S104795112200261X
Financial support
The Western Canadian Complex Pediatric Therapies Follow-up Program has been supported over the years by contributions from the following: Alberta Health, Stollery Children’s Hospital, Women and Children’s Health Research Institute, referral-site follow-up clinics (Saskatoon and Regina SK, Winnipeg MB, Calgary AB, Vancouver BC), and the Glenrose Rehabilitation Hospital Research Trust, with ongoing funding by the Glenrose Rehabilitation Hospital. These funding agencies had no role in the design and conduct of the study; collection, analysis, or interpretation of the data; preparation, writing, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Conflicts of interest
None.
HREB Number for CPFTP Registry
Pro00001030 (Approved yearly, last October 19, 2020). This number comes from our local research ethics board.
Consent statement
Patients were identified at the time of complex cardiac surgery at which point consent was obtained and they were recruited for inclusion into the Western Canadian Complex Pediatric Therapies Follow-up Program (CPFTP) registry.










