The coronavirus disease of 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first described in Wuhan, China in December, 2019 Reference Wu, Hao and Lau1 and by March, 2020, it had been declared a pandemic by the World Health Organization. 2 Nigeria recorded its first case of COVID-19 in March, 2020 3 and by the end of the same month, a lockdown had been declared in several states nationwide with a suspension of all interstate travel. COVID-19 is mainly characterised by a viral pneumonia with several systemic manifestations and complications described. Reference Wang, Hu and Hu4
Although the asymptomatic or minimally symptomatic nature of COVID-19 in children has been reported, Reference Dong, Mo, Hu, Qi, Jiang and Tong5 a Kawasaki disease-like toxic shock syndrome was documented among children presenting at a hospital in the United Kingdom Reference Riphagen, Gomez, Gonzalez-Martinez, Wilkinson and Theocharis6 and drew attention to the deleterious effect of this viral disease even in previously well children. Apart from the direct effects of COVID-19 on multiple body systems, the indirect effects of the pandemic are becoming more apparent as the days progress. Maternal and child health services in sub-Saharan African, which have previously been characterised by inadequacies in terms of quantity and quality have been further hampered by the consequences of the pandemic.
As is the case in many parts of the world, CHD when compared to acquired heart disease forms the bulk of paediatric cardiac defects in Nigeria. The prevalence of CHD among Nigerian children is estimated as 6.6 to 18.1 per 1000 from studies in three major cities in the west, north, and south of the country. Reference Ekure, Sokunbi and Kalu7
The coverage of paediatric cardiac services in sub-Saharan Africa has long been suboptimal to cater for the large number of children born yearly with CHD. The region’s paediatric CHD patients are majorly served by local paediatric cardiologists who provide medical care where possible with referrals to institutions abroad for surgery and follow-up care for these children is also provided locally on their return. Paediatric cardiac surgical care is sparsely provided with only several countries that are able to boast of few centres to offer this service. Many of the local centres function on a mission basis with expatriate teams comprised of surgeons, cardiac anaesthetists as well as operating room and intensive care unit (ICU) nurses who visit these countries on a regular schedule and perform batched surgeries on a predetermined list of children. There are few options for children requiring emergency cardiac surgery or who have complicated and/or complex heart defects and may be too ill to travel outside the country.
With restrictions on international travel and with global scarce resources for health care, paediatric cardiac services in Nigeria, and indeed sub-Saharan countries will need to take giant steps to rise to the occasion. While several other specialities may “scale down” services due to the ravaging pandemic; the previously sparsely utilised paediatric cardiac service in the developing world, especially in sub-Saharan Africa, will require a region-adapted guideline to “scale up” services to cater for the most needy while providing a safe environment for healthcare workers, patients, and their caregivers.
Such has been the case at the Babcock/Tristate Heart and Vascular Centre, Babcock University Teaching Hospital, Ilishan–Remo, Ogun State, Nigeria where the institution has had to maintain paediatric cardiac services despite the COVID-19 pandemic, including complex surgeries on children who would have otherwise been referred abroad to avail themselves of more advanced care.
The bar graph (Fig 1) shows the analysis of paediatric cardiac surgical evaluations and procedures in the preceding 12 months. This includes total visits, surgeries undertaken at the institution solely by the local on-site team, procedures performed with visiting teams, and cases considered complex and requiring more advanced care than that available locally. The bar graph shows the increase in the proportion of operated cases compared to total evaluations during the months of the pandemic with the highest number of monthly cases performed despite the pandemic; a likely consequence of compulsive utilisation of local expertise; a trend which may persist as the pandemic lingers. For example, the centre performed its first ever and successful neonatal arterial switch operation during this period. Without restriction on international travel, such children would have sought care outside the country; this is the occasion that indigenous teams must rise to.
Despite the increased demand, measures must be put in place to ensure the protection of patients and healthcare workers; judicious use of resources; appropriate triaging of patients to meet the needs of the majority and pre-, intra-, and post-operative care of patients using best practices in an environment that is safe for everyone.
Recommendations
All recommendations on the prevention of the transmission of COVID-19 stated by the World Health Organization 8 were enforced and adhered to by all clinical and allied health workers as well as patients and their relatives visiting the facility. Other recommendations such as that issued by the American Heart Association 9 were gleaned from the further guide care of patients with emergency conditions, cardiovascular diseases, and those requiring cardiopulmonary resuscitation. From the centre’s experience, we propose the following guidelines for various aspects of paediatric cardiac care.
Screening procedures
-
Screening checklists: The use of standardised screening questionnaires prior to admittance into the cardiac facility should be performed on arrival at the hospital. A simple but effective screening tool is advised to enable seamless traffic of patients and minimal contact time between patients and the interviewer. As the pandemic hits the phase of community transmission, checklists about travel history or contact with a recent traveller to a region with high transmission of COVID-19 may be grossly inadequate in assessing the likelihood of infection. Contact with any person with confirmed COVID-19 infection should constitute significant history. However, with the possibility of transmission by asymptomatic carriers, 10 the absence of symptoms should also not be misconstrued as “low” or “no” risk.
-
History of symptoms of ill health (especially respiratory and gastrointestinal symptoms) should be quickly assessed prior to entry to the facility and temperature reading using infra-red thermometers should be performed by a healthcare worker well kitted in appropriate Personal Protective Equipment (PPE) while maintaining physical distance as much as possible.
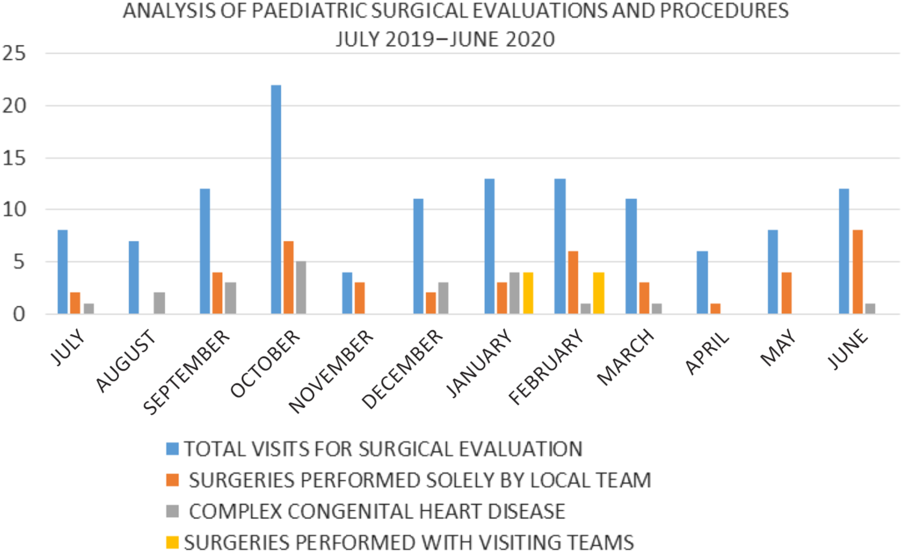
Figure 1. Paediatric cardiac surgical evaluations and procedures at the Babcock/Tristate Heart and Vascular Centre, Babcock University Teaching Hospital, Ilishan–Remo, Ogun State, Nigeria from July, 2019 to June, 2020.
Provision of a safe work environment
-
Materials for hand hygiene including sinks with running water, liquid soap, hand dryers, and alcohol-based sanitisers should be stationed at the entrance of the facility and at strategic points within to encourage frequent and stress less handwashing practice.
-
Waiting areas, consulting rooms, inpatient wards, operating theatres, and ICUs should be decongested where required and arranged to ensure proper ventilation and adjusted sitting and lying arrangements, respectively, to conform to recommended social distancing.
-
Information, communication, and education materials on COVID-19 including posters and recorded messages on the televisions and/or sound systems present in the facility should be placed and played, respectively, to provide continuous guidance to persons within the facility.
-
Cleanliness of the work environment should be top priority and this should be carried out in consulting spaces and waiting areas including work equipment such as scan and electrocardiography machines, floors, door handles, work surfaces, and swipe card readers.
-
Diaper hygiene before or during patient encounters as well as proper disposal should be paid attention to considering the reports of the possibility of faecal transmission of SARS-CoV-2. Reference Xiao, Tang, Zheng, Liu, Li and Shan11
Appropriate attires
-
Face masks should be worn by all persons within the facility according to WHO recommendation. 8
-
All healthcare workers should be appropriately dressed in disposable gowns, head covers, surgical masks, and face shields for all patient encounters.
-
In the emergency room and outpatient clinic, the use of N95 masks is encouraged for healthcare workers who will be first responders or who will inadvertently be in close contact with patients for prolonged periods such as during the performance of clinical examination, electrocardiography, or echocardiography. This is considered safer as most patients and relatives visiting the outpatient clinic or emergency room cannot be reliably categorised in terms of infectivity of or risk of transmission of COVID-19 and cardiac symptomatology such as cough, cyanosis, fast, and laboured breathing may overlap with respiratory features of COVID-19. The possibility of unanticipated aerosol production in these settings such as from violent coughing or crying from children or the need to provide oxygen, bag, and mask ventilation or suctioning cannot be disregarded.
Outpatient clinics
Outpatient clinics form the bulk of most paediatric cardiac facilities in the region and are mainly made up of patients awaiting interventions as well as children being followed up post-interventions. The large numbers of patients that characterise these clinics can serve as a “hot spot” for viral transmission if not properly organised. The following measures were adopted at the centre to ensure significantly decongested outpatient clinics while catering for the needs of all categories of patients and these are proposed:
-
Scheduling: All visits to the outpatient clinic must be scheduled. The daily patient load should be that which the facility can handle with reasonable physical distancing as well as with adequate provision for seamless patient flow.
-
New evaluations: First-time patients should be engaged via telephone, text messages, or e-mails to verify the clinical state of the child from the parents or caregivers. This should provide information to guide the timing of a scheduled visit or need for immediate presentation for medical attention. Parental anxiety should be considered noteworthy. Partial or total lockdowns as well as the false perception of a high likelihood of contracting the dreaded COVID-19 within the hospital environment may remarkably hamper presentation to the healthcare facility; thus caregivers who are willing to make this “sacrifice” should be given due attention.
-
Pre-operative follow-up: This usually forms a significant population in paediatric cardiology clinics in the developing world where the paucity of funds or facilities for interventions makes waiting lists extensive. Telephone calls, text messages, and e-mails can be utilised to verify a child’s clinical condition. In the absence of clinical deterioration of the patient, routine medications can be prescribed for caregivers to pick up without the child presenting to the health facility.
-
Post-operative follow-up: Tools for telemedicine as mentioned above should be utilised to assess the child’s well-being. However, it is advised that immediate post-operative patients (within the first 3 months of surgery or intervention) should maintain clinic visits according to standard institutional protocols for close monitoring.
Following a remote assessment of the patient’s welfare, the child is scheduled for an outpatient clinic appointment or directed to present at the emergency room as required.
Emergency services
-
Emergency room admissions should be maintained.
-
Triage areas for holding patients with a high index of suspicion of COVID-19 should be provided.
-
Protocols for quick testing should be put in place to enable the transition to an isolation ward or a regular ward as appropriate depending on the result of viral testing.
-
The features of COVID-19 have major overlaps with those of cardiac pathology; thus where possible all children presenting with any of the symptoms or signs of COVID-19 should have testing for SARS-CoV-2. This will ensure proper clinical management once a diagnosis is established.
Inpatient admissions
-
The inpatient admissions should constitute patients who have been certified COVID-19 negative where required or who have other confirmed diagnoses.
-
If the institution is certified for clinical management of COVID-19, this should be done in a designated ward separate from regular patients and with avoidance of cross rostering of staff to reduce the risk of transmission among staff and patients.
Cardiovascular investigations
-
A detailed statement on the guidelines for performance of echocardiography during the COVID-19 pandemic has been issued by the American Society of Echocardiography Reference Kirkpatrick, Mitchell, Taub, Kort, Hung and Swaminathan12 and a supplement document addresses peculiarities of the paediatric and fetal population requiring echocardiograms. Reference Barker, Lewin and Donofrio13 These comprehensive documents are recommended as they address several aspects of cardiovascular investigations including fetal, transthoracic, and transoesophageal echocardiography.
-
All elective cardiac investigations should be deferred. These investigations should be performed only when the results are required to establish a diagnosis or if findings obtained will alter the patient’s ongoing treatment regimen.
-
Investigations should be performed by the most skilled personnel available to reduce patient contact time both with the healthcare worker and within the facility; and complex echocardiograms should be reserved for highly skilled sonographers. This level of speed and accuracy is also required for smooth patient flow without compromising the accuracy of tests.
-
Point-of-care ultrasound sound (POCUS) may be utilised where appropriate, but it is more beneficial in long term to perform a comprehensive examination with archived images which will be reviewed remotely and measurements taken. This, however, may be limited by the sophistication of the available equipment.
-
The use of checklists is encouraged to ensure that no part of the examination is omitted as this will mean a repeat procedure with attendant wastage of time, non-judicious use of personal protective equipment, and increased risk associated with more patient–health worker encounters.
-
The use of disposable electrocardiography electrodes is advised to limit the transmission of infection by fomites.
-
Sedation is advised for young children to aid quick, detailed examinations and to avoid violent crying, salivation, coughing, and screaming all of which may be aerosol generating.
-
Transoesophageal echocardiogram should be avoided as much as possible as it carries a high risk of aerosol generation. Other less invasive modalities including computerised tomography and magnetic resonance imaging as appropriate should be utilised in its stead.
-
Echocardiography for paediatric cardiac patients with COVID-19 should be quick, accurate, and targeted. Covering of probes and machine consoles should be considered if this will not impede image quality or speed of examination, and thorough cleaning of the probe and machine with disinfecting substances should be followed according to the manufacturer’s guidelines. Reference Barker, Lewin and Donofrio13 Rarely, where possible a separate machine should be reserved for patients with COVID-19.
Cardiac catheterisation
As with non-invasive investigations, cardiac catheterisation procedures should be carried out only if considered “essential”.
-
Diagnostic procedures should be performed if this is considered necessary for surgical intervention or if surgery is to be done urgently. Non-invasive imaging such as computerised tomography and magnetic resonance imaging is preferred if the required information can be obtained using these modalities.
-
Interventional procedures should be undertaken if considered as urgent and life saving. Procedures such as balloon atrial septostomy, relief of critical pulmonary and aortic valve stenosis, and stenting of the arterial duct would likely be favoured above elective device closures.
Cardiac surgery
It is expected that there will be an upsurge in surgical cases in the pandemic and post-pandemic period. As international travel restrictions remain in place and till people feel more comfortable to travel outside their native abode, more patients are likely to seek cardiac surgical care locally.
Triaging/prioritising
-
It is recommended that emergency surgical procedures such as the creation of aortopulmonary shunts, repair of obstructed total anomalous pulmonary venous connection (TAPVC), coarctation repair, and relief of critical ventricular outflow obstructions not amenable to catheterisation will be prioritised above urgent procedures such as arterial switch operation, Norwood procedure, repair of unobstructed TAPVC, truncus arteriosus repair, superior cavopulmonary anastomosis, and pulmonary artery banding.
-
Infants with large shunt lesions, which can be planned on an elective basis should be adequately monitored and also be considered for surgical correction early enough to prevent the onset of pulmonary arterial hypertension and other complications. Guidelines for monitoring of waiting lists for cardiac programmes have been documented previously. Reference Sethuraman, Jeremiah and Ryo14
-
Elective cases should be deferred except in cases where surgical lists have been completely run and even then, the capacity to accommodate emergency and urgent cases must be reserved.
-
Complicated and high-risk cases should be undertaken with caution in resource-limited settings to minimise the inevitable pressure on resources (both staff and equipment) which comes with managing such children intra- and post-operatively.
Pre-operative screening and testing
-
Pre-operative microbiological testing for COVID-19 should be carried out on all patients and at least on one relative who will be allowed access into the ICU and the ward. It is advised to obtain direct viral testing using reverse transcription–polymerase chain reaction (RT-PCR) that has been shown to be the most reliable diagnostic test. Reference Benedetto, Goodwin, Kendall, Uppal and Akowuah15
-
The utility of antibody testing with high specificity and sensitivity Reference Benedetto, Goodwin, Kendall, Uppal and Akowuah15 is yet to be established as a reliable screening tool, but the usefulness in resource-constrained settings is still to be determined. Several developing countries have had to grapple with the cost and availability of RT-PCR testing even for the general population according to public health requirements. While it has been advocated to obtain reliable testing, the added cost of mandatory pre-operative testing in terms of added financial implication and delay in surgical intervention remains a factor in resource-constrained settings. Nevertheless, the added morbidity and risk of mortality of concomitant COVID-19 infection in the cardiac surgical patient cannot be overemphasised.
-
Regulating the movement of relatives in and out of the facility is essential and cautionary advice to patients’ relatives to practise adequate social distancing when outside the treatment facility should be reiterated to minimise the risk of acquiring a “new” onset COVID-19 infection even after an initial negative test.
Intra- and post-operative precautionary measures
-
It is recommended that personal protective equipment be utilised in the operating room and ICU, notwithstanding the COVID-19 status of operated patients. Reference Faraoni, Caplan and DiNardo16
-
Guidance for anaesthesia in paediatric heart programmes has been given previously Reference Faraoni, Caplan and DiNardo16 and while these are invaluable at this time; ultimately, region-specific guidelines would be essential to adapt best practices to available resources in each geographical location.
-
Bed spacing and rostering of staff in the ICU should be adequate to ensure optimisation of facility resources and engagement of fewer staff per shift, but sufficient to cater for the needs of admitted patients to avoid compromising outcomes.
The role of telemedicine
More than ever before, the role of virtual gathering in different system settings has been largely explored during the COVID-19 pandemic. Telemedicine has played a huge role in the continuity of healthcare delivery, especially on outpatient basis. Speciality consultations from experts in more advanced climes will be an invaluable resource for practitioners in developing countries. While some specialities such as cardiac surgery and interventional cardiology may be limited in their adaptability, other care areas such as intensive care and non-invasive investigations can benefit from virtual discussions and communications through conference calls with specialists who in some cases may have visited such centres but for the pandemic.
Challenges and measures taken
Despite the desire to provide high quality and affordable care to children with cardiac defects in these trying times, service provision is not without its constraints. Some of the limitations that were experienced as well as measures to tackle them, where possible, are highlighted below:
-
COVID-19 testing capabilities in low-and medium-income countries (LMICs) have been hampered by the restricted supply of testing kits, similar to several nations even in the developed world. As the feasibility of widespread testing remains challenging in both developed and developing countries, the utility of region adaptive measures such as screening checklists and serology testing for COVID-19 may still need to be given consideration in resource-limited settings.
-
Inadvertent utilisation of cardiac facilities for the management of patients with severe forms of COVID-19: Most cardiac centres in sub-Saharan countries are some of the most sophisticated healthcare institutions available in their native countries and by default may be recruited for the care of patients with COVID-19 requiring organ support. Indeed, the institution was legislated by the state government to withhold all non-emergency cardiac services for the first one month following the documentation of the index patient with COVID-19 in Nigeria. The aim was to make available critical care services and equipment for organ support for patients with critical COVID-19. However, two weeks into the lockdown, the dire need for cardiac services nationwide and the restriction on international travel necessitated the reopening and continued operation of the few centres providing this essential service. The re-commencement of services was preceded by meetings to reorganise service delivery and the institution of strict protective measures to ensure the safety of staff and patients within the hospital environment. This received the immense support of the government. The extent to which these legislations are “eased” in several regions will proportionately increase the reversion of cardiac facilities to service delivery as in the pre-COVID-19 era.
-
Increased workload and more frequent scheduling of staff despite reduced remuneration: The immense global economic crisis which occurred side by side the pandemic had some of the greatest impacts in LMICs and Nigeria was not left out. Pay cuts that were commonplace in many global establishments also became necessary at the institution. However, while most establishments experienced a commensurate reduction in work schedules, the staff at the institution had to work extra shifts and longer hours to cope with an increased patient load; as options for local paediatric cardiac surgical care were limited nationwide. Constant psychological support for staff, and careful attention to staff safety and welfare were some of the factors which contributed to sustained staff satisfaction. Testing for COVID-19 and permission was granted for self-isolation if necessary.
-
Performance of complex cardiac surgeries requiring highly specialised intensive care was a major challenge and this was tackled using a multi-pronged approach:
-
Emergency procedures such as arterial switch operation (ASO) were performed because the surgical skill was available to perform these procedures previously, although limitations in available facilities for intensive care of complex CHD had been an impediment to undertaking these surgeries in the past. Moreover, with access to facilities abroad which could offer more advanced care, there were few referrals of complex CHD by paediatricians and paediatric cardiologists to local cardiac surgeons. Only one arterial switch operation had previously been performed at the centre for a two month-old infant about nine months before the COVID-19 pandemic and though surgery had been successful, intensive care had been the major challenge. The ASO performed during the pandemic was the first neonatal arterial switch operation performed at the institution and intensive care was augmented by round-the-clock discussion with experienced paediatric cardiac intensivists in different parts of the globe via internet voice calls, video calls, and chats using mobile applications including Facetime, WhatsApp, Zoom, and Telegram. Colleagues in different parts of the globe including North America, South America, the Middle East, and Asia were engaged to make provision for the differences in time zones in order to ensure unlimited communication with experts as required.
-
Local collaboration was also undertaken and involved the performance of complex cardiac surgeries with senior local surgeons from other cardiac centres in the country who were not doing complex surgeries independently, but were routinely running cardiac operating lists for low-risk cases. The collaboration of experienced surgeons previously operating independently provided the advantage of diverse skill, quicker surgeries, and less fatigue on the few available personnel.
-
High-risk procedures were substituted for less risky procedures when possible. In conditions where beneficial palliative procedures were feasible and did not increase the risk of complications at corrective surgery, such simpler procedures were performed. These included pulmonary artery banding for very large ventricular septal defects with severe pulmonary hypertension in small infants and Blalock–Taussig shunts in infants with Tetralogy of Fallot. These procedures were considered less risky and cost-effective for both the patient and the institution, given the constraints for expertise, consumables, and pharmacological agents available during the period of the pandemic.
-
Some non-urgent, high-risk cases with estimated low success rates post-operatively such as large left-to-right shunts with borderline operability in older children were deferred temporarily to reduce strain on staff and infrastructure during the pandemic. In fact, the financial implication including long ICU stays with the attendant costs in the midst of the pandemic as well as high risk of mortality explained to parents made some caregivers electively opt to defer these procedures of their free will. With the non-availability of alternative indigenous care, such patients will have planned inclusion on the surgical lists as the pandemic eases off and local care resumes to full capacity or overseas referrals are possible.
-
Extensive parental counselling was carried out in all cases to fully explain the prevailing limitations, reasons for procedures chosen and/or deferred, to obtain full written informed consent of caregivers, whose wishes were respected within the limits of medical ethics.
-
-
As before the pandemic, expertise in some aspects of cardiac care including some complex surgical and interventional procedures, electrophysiology services and advanced imaging will remain unavailable and patients requiring such services will need to “wait” the pandemic out.
-
The availability and cost of consumables: Many consumables utilised in cardiac care services are not sourced locally and importation in the face of the COVID-19 pandemic has been an uphill task. Even when the challenges of importation are surmounted, manufacturing restrictions in source countries as well as increased costs of materials have not made procurement any easier.
-
Long waiting lists of patients will still be the reality as few centres are equipped to continue service provision, especially with current safety guidelines.
-
As guidelines of social distancing make medical interactions largely online, the problems of poor telecommunication networks and internet connectivity in developing countries need to be tackled to achieve seamless communication. Telemedicine in strict terms cannot be carried out successfully in the face of these technological constraints and these deficiencies need to be addressed to facilitate the utility of technology for medical communication.
Lessons learned
-
One important lesson we, and indeed the world at large have gained from this pandemic is that we can go farther together. Local collaboration with advantages of economies of scale, skills, and knowledge exchange among indigenous personnel within the country constitutes an important part of strengthening the paediatric cardiac care system in the sub-Saharan region. This may be the time to consider coalescing already existing paediatric cardiac centres within the same geopolitical zone into single larger facilities that are better able to provide comprehensive paediatric cardiac service coverage rather than multiple individual centres with grossly limited capabilities.
-
Beyond the period of the pandemic, virtual communications will remain an invaluable tool in improving patient care through real-time discussions and also offer the opportunity for remote tutoring and mentoring in the field of paediatric cardiac care. Telemedicine can however not substitute formal fellowship and training programmes; as basic knowledge and skills form the foundation on which remote guidance can thrive.
-
Indeed, the COVID-19 pandemic has been an accelerated learning curve in indigenous paediatric cardiac care, which has taken the local teams on a path of self-actualisation. It is possible that this may be a silver lining that will hasten the much-needed transition to widespread fully independent and comprehensive paediatric cardiac care programmes in the country and the sub-Saharan region as a whole.
Conclusions
The care of children with CHD requires attention as the pandemic progresses. The need to scale-up services is inevitable to avoid further collateral damage from the effects of the COVID-19 pandemic. There is a need for a region-adapted guideline for service provision to cater for the needs of the majority of patients while providing a safe environment for healthcare workers, patients, and their caregivers. These efforts must be undertaken with consideration for the prevailing phase of the pandemic at any given time. Judicious balance between patient needs and available resources of the healthcare system must be ensured with regular communication between hospital staff, administration systems, and public health teams in each locality to verify the adequacy of guidelines at any given time, as the pandemic progresses or hopefully eases off.
Acknowledgements
We thank the entire staff of Babcock/Tristate Heart and Vascular Centre, Babcock University Teaching Hospital, Ilishan-Remo, Ogun state, Nigeria, the patients and their families.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Authors’ contributions
OJS, OM, BOU, and MOS conceptualised and designed the work; OJS, OM, and BOU drafted the manuscript; AO, AI extracted, analysed, and represented the data shown in this work; MOS, AO, OJS, and AI revised the manuscript critically for important intellectual content. All authors reviewed the manuscript and approved its submission.




