Cardiac arrest occurs in 2–6% of children admitted to a paediatric ICU which is approximately 100-fold higher than out-of-hospital cardiac arrest.Reference Slonim, Patel, Ruttiman and Pollack1Reference Suominen, Okkola, Voipio, Korpela, Palo and Rasanen2Reference Young, Gausche-Hill, McClung and Lewis3Reference Donoghue, Nadkarni and Berg4 Survival to hospital discharge after paediatric in-hospital cardiac arrest in the United States remains less than 45% despite advances in resuscitation science over the last 20 years.Reference Slonim, Patel, Ruttiman and Pollack1Reference Girotra, Spertus and Li5Reference Bhanji, Topjian and Nadkarni6 In a large registry study of paediatric in-hospital cardiac arrest patients, risk-adjusted rates of 24-hour survival as well as survival to hospital discharge were lower when cardiopulmonary resuscitation occurred at night, compared to cardiopulmonary resuscitation events occurring during daytime or evening hours.Reference Bhanji, Topjian and Nadkarni6 The same study noted lower 24-hour survival for events that occurred during weekends compared to days and weekdays.Reference Bhanji, Topjian and Nadkarni6Reference Christensen, Lee, Gowen, Rettiganti, Deshpande and Morray7Reference Esangbedo, Yu and Raymond8 These differences in outcomes have also been found in children with out-of-hospital cardiac arrest and adults with in-hospital cardiac arrest and out-of-hospital cardiac arrest.Reference Peberdy, Ornato and Larkin9Reference Shinohara, Muguruma, Toida, Gakumazawa, Abe and Takeuchi10Reference Kitamura, Kiyohara, Nitta, Nadkarni, Berg and Iwami11Reference Lin, Shi, Wang and Liang12 Additionally, a study of paediatric extracorporeal cardiopulmonary resuscitation found worse neurologic injury when extracorporeal cardiopulmonary resuscitation occurred at nights or on weekends.Reference Burke, Chan, Brogan and McMullan13 The reasons for this difference in outcomes are unclear, however, prior studies have shown it is not secondary to disparities in cardiopulmonary resuscitation quality.Reference Esangbedo, Yu and Raymond8Reference Wolfe, Morgan and Sutton14
Hospitalized children with CHD have a ten-fold higher risk of cardiac arrest than children without CHD.Reference Lowry, Knudson, Cabrera, Graves, Morales and Rossano15 There have been no studies to date looking at whether children with CHD have disparities in survival or cardiopulmonary resuscitation quality among those in-hospital cardiac arrests that occur during nights or weekends compared to days and weekdays. If children with CHD who suffer in-hospital cardiac arrest do have lower rates of survival during nights and weekends like the general paediatric population, this could influence potential modifiable factors such as hospital staffing, which has been shown to be associated with outcomes after in-hospital cardiac arrest in the paediatric cardiac intensive care unit.Reference Gaies, Clarke, Donohue, Gurney, Charpie and Hirsch16 We hypothesise that children with CHD will have lower rates of survival for in-hospital cardiac arrest occurring during nights and weekends, and that those differences will not be explained by differences in cardiopulmonary resuscitation quality.
Materials and method
Data collection
Pediatric in-hospital cardiac arrest data was collected from the Pediatric Resuscitation Quality (pediRES-Q) Collaborative (ClinicalTrials.gov: NCT02708134), a large international multi-centre network of children’s hospitals that collects data on paediatric cardiac arrests and chest compression quality metrics (Appendix 1). The study was approved by each hospital’s institutional review or research ethics board. There was a waiver of consent per United States Code of Federal Regulations 45 CFR 46.116(d) and 45 CFR 46.408(a). Data use agreements were obtained for each institution and compliance with the Health Insurance Portability and Accountability Act (HIPAA) was maintained.
For each index in-hospital cardiac arrest event, we collected data on prospectively selected pre-arrest, intra-arrest and post-arrest factors. Pre-arrest characteristics included patient demographics, admission type (surgical versus medical), ventricle status (single ventricle versus other) [single ventricle defined as lacking two well developed ventricles at all stages of repair including preoperative, Stage 1, Stage 2, and Stage 3], cardiac arrest aetiology, and interventions in place at the onset of in-hospital cardiac arrest. Intra-arrest data included chest compression quality [chest compression depth, chest compression rate and chest compression fraction], timing of arrest, presence of invasive monitoring prior to the onset of cardiac arrest (arterial line or end tidal carbon dioxide), initial rhythm, duration of chest compressions and use of extracorporeal cardiopulmonary resuscitation. Post-arrest data included arrest outcome, hospital survival outcomes and selected post-resuscitation care variables. Chest compression quality metric data were recorded using the ZOLL R-series monitor-defibrillator (ZOLL Medical, Chelmsford, MA) and dual sensor defibrillator pads, placed on the anterior (chest) and posterior (back) of the patient. Accelerometer-based technology embedded in each pad recorded chest compression rate, depth and fraction and mitigated depth artefact caused by hospital mattress deflection during compressions.Reference Niles, Duval-Arnould and Skellett17
Inclusion and exclusion criteria
We included patients who had a diagnosis of CHD, < 18 years of age at time of arrest, ≥ 37 weeks gestational age, and had an index in-hospital cardiac arrest with at least 5 minutes of monitor-defibrillator chest compression quality metric data recorded. We excluded patients with out-of-hospital cardiac arrest, including patients who arrived to the emergency department actively receiving cardiopulmonary resuscitation. Patients were excluded if they were already on extracorporeal membrane oxygenation at the beginning of the arrest, or if there were limitations to cardiopulmonary resuscitation in place. In analysis of chest compression epochs, we excluded events if only apical anterior placement defibrillator pads were used (e.g. surface deflection artefact potential) or if accelerometer depths of < 1.5 cm or > 8 cm were recorded, as this was likely artefact.
Definition of cardiopulmonary resuscitation quality metrics and time variables
Epochs were defined as 60 s increments of chest compression data. We recorded compliance of each epoch with the American Heart Association’s 2020 guidelines for basic life support with the predefined targets of chest compression rate 100–120 per minute; chest compression depth ≥ 3.4 cm for < 1 year of age and ≥ 4.4 cm for 1 to < 8 years of age, and 4.5–6.6 cm for 8 to < 18 years of age; and chest compression fraction ≥ 80%. Chest compression fraction refers to the percentage of time during a cardiopulmonary resuscitation event that chest compressions were performed without interruption. Compliance for each event was defined as ≥ 60% of event epochs meeting these AHA guideline targets. We compared chest compression quality metrics and outcomes of in-hospital cardiac arrest between events that occurred during the day versus night. We also compared the same for weekday versus weekend events. We defined “day” as 07:00 to 22:59, and “night” as 23:00 to 06:59, “weekday” as Monday 07:00 to Friday 22:59, and “weekend” as Friday 23:00 to Monday 06:59. For day versus night events and weekday versus weekend events, we compared pre-arrest characteristics within 2 hours of each event: lowest pH, highest lactate and highest vasoactive inotrope score (VIS), as well as two elements of post cardiac arrest care within the first 6 hours after each event: presence of fever (defined as temperature > 38° Celsius) or hypotension (defined as systolic blood pressure < 5th percentile for age).
Outcome measures
Outcome measures evaluated included return of spontaneous circulation, return of circulation with or without extracorporeal membrane oxygenation, survival to hospital discharge and survival to discharge with favourable neurological outcome. Return of spontaneous circulation was defined if spontaneous circulation was achieved for a period of at least 20 minutes. Return of circulation was defined as either achieving return of spontaneous circulation or successful cannulation for extracorporeal membrane oxygenation during the cardiac arrest event. Survival with favourable neurological outcome was prospectively defined as a Pediatric Cerebral Performance Category score of 1, 2 or 3 at the time of discharge from the hospital, or no change from pre-arrest Pediatric Cerebral Performance Category score.Reference Fiser18 We also used an alternate definition of survival with favourable neurologic outcome for a sensitivity analysis of Pediatric Cerebral Performance Category score of 1 or 2 at the time of discharge from the hospital, or no change from pre-arrest Pediatric Cerebral Performance Category score.
Statistical analysis
Demographic and clinical characteristics are presented as median/IQR (interquartile range) for continuous variables and percentages for categorical variables. For each event, we calculated chest compression quality metrics of median chest compression rate and chest compression depth, as well as the percent of epochs with chest compression fraction ≥ 80%. We then reported the overall median chest compression rate, depth and fraction by characteristics and outcomes. Associations between chest compression metrics and day/night, weekend/weekday, return of spontaneous circulation, return of circulation, survival to hospital discharge and survival to hospital discharge with favourable neurologic outcome were analysed utilising Wilcoxon rank sum, Chi square and Fisher’s exact tests. Analyses were stratified by age group, time of day and day of week for outcomes. Multivariable logistic regression models were used to assess the relationship between outcomes and age category, time of day, day of week, initial rhythm, hospital site and chest compression quality metric compliance, with odds ratios and 95% confidence intervals presented. Age, duration of arrest, illness category, presence of end tidal carbon dioxide or indwelling arterial line monitoring, and initial cardiac rhythm were included in the models as covariates. We also performed sensitivity analysis with an alternate definition of “day” and “night”, with “day” defined as 08:00 to 16:00, and “night” defined as 23:00 to 06:59. We performed a sensitivity analysis with an alternate definition of “weekday” and “weekend,” with “weekday” defined as Monday through Friday 08:00 to 16:00 and “weekend” defined as Saturday and Sunday 08:00 to 16:00. There were multiple reasons for choosing a primary and secondary definition of day/night and weekday/weekend for our analysis. The primary definition was chosen for consistency since prior studies from the pediRES-Q collaborative have used this definition.Reference Esangbedo, Yu and Raymond8Reference Niles, Duval-Arnould and Skellett17 The alternate definitions were chosen for a more precise differentiation between day/night and weekday/weekend. The alternate definition of day/night was chosen to be consistent with a prior study from the pediRES-Q collaborative.Reference Esangbedo, Yu and Raymond8 The alternate definition of weekday/weekend was chosen in order to better differentiate weekday days and weekend days. Additionally, we performed a sensitivity analysis of compliance using expanded limits of chest compression rate of 90–130 and chest compression depth (±10% for each age category).
Results
There were 132 in-hospital cardiac arrest events in CHD patients with five or more evaluable 60-sec epochs of chest compression metrics and complete data included in this analysis from 21 participating sites (1–38 events per site) from the pediRES-Q Collaborative. Data was collected between October, 2015 and July, 2020. From these 132 cardiac arrest events, there were 3614 epochs of chest compression data that were analysed (Fig 1). Table 1 summarises the patient demographics and event data studied by age category. Fifty percent of patients were categorised as surgical cardiac. Thirty-six percent of patients had a diagnosis of single ventricle. The majority of patients had invasive monitoring by end tidal carbon dioxide (83%)or indwelling arterial catheter (55%) prior to the onset of the cardiac arrest. Surgical patients compared to medical cardiac patients were more likely to have an indwelling arterial catheter in place prior to the onset of arrest (70% vs. 41%, p = 0.0015), but no differences in end tidal carbon dioxide monitoring prior to the onset of arrest (86% vs. 79%, p = 0.36). Table 2 summarises the characteristics of the cardiac arrest events. There were a higher percentage of extracorporeal cardiopulmonary resuscitation events during the weekday compared to the weekend. Supplemental Table 1 displays the extracorporeal cardiopulmonary resuscitation events by age category and time of day/day of week using the primary definitions of day/night and weekday/weekend. Supplemental Table 2 displays the extracorporeal cardiopulmonary resuscitation events by age category and time of day/day of week using the alternate definitions of day/night and weekday/weekend. Extracorporeal cardiopulmonary resuscitation events that occurred during the night versus day had longer cardiopulmonary resuscitation duration [59 minutes (49.5, 71.0) versus 47.5 minutes (40.0, 54.0); p = 0.026]. Extracorporeal cardiopulmonary resuscitation events that occurred during the weekend versus weekday had no difference in cardiopulmonary resuscitation duration [55 minutes (40.0, 64.5) vs. 48 minutes (43.0, 61.0); p = 0.74].

Figure 1. Flow diagram for data analysis. IHCA: In-hospital Cardiac Arrest; ROSC: return of spontaneous circulation; ROC: return of circulation; SHD: survival to hospital discharge.
Table 1. Demographics and event epochs by age category

IQR: interquartile range.
Table 2. Cardiac arrest event characteristics

ICU, intensive care unit; VF, ventricular fibrillation; VT, ventricular tachycardia; CO2, carbon dioxide; CPR, cardiopulmonary resuscitation; ECPR, extracorporeal cardiopulmonary resuscitation.
Table 3 summarises the chest compression quality metrics and compliance for all patients by age category during the day compared to night and weekday compared to weekend. There was no significant difference in chest compression rate, depth or fraction for events occurring during the day compared to night or weekday compared to weekend. The only exception was for the 8 to < 18-year age group who had a higher chest compression fraction at night compared to day (p = 0.04). Compliance with AHA guidelines also did not differ by time of day or day of week in any age category. When using the alternate definition of compliance, there were similar results with no significant difference. Overall, compliance was low in all age categories, mainly due to chest compression depth not meeting the targets specified by the AHA guidelines. When determined for just chest compression rate and chest compression fraction (not including chest compression depth), compliance improved. Of note, when using the alternate definition of day/night and weekday/weekend, there were similar results with no significant difference noted (Supplemental Table 3).
Table 3. Cardiopulmonary resuscitation metrics and percent compliance with American Heart Association 2020 basic life support guidelines
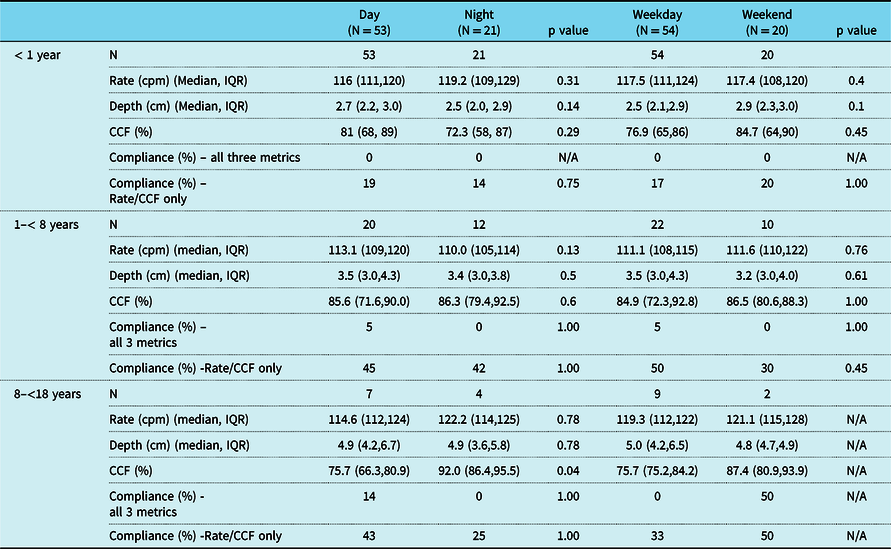
*(N = 117, 15 excluded for inappropriate sensor and placement).
cpm, compressions per minute; IQR, interquartile range; cm, centimeters; CCF, chest compression fraction.
Table 4 displays outcome by time of day and day of week. There was no significant difference in return of spontaneous circulation or return of circulation between days compared to nights or weekdays compared to weekends. There was a significant increase in survival to hospital discharge for events occurring on weekdays compared to weekends overall (47% versus 26%; p = 0.03), but no difference with events on days compared to nights. Survival to hospital discharge with favourable neurological outcome (using the primary and alternate definition) did not differ by time of the day or day of week overall, or after controlling for age category. Supplemental Table 4 displays outcomes using the alternate definition of day/night and weekday/weekend. There were similar results in outcomes noted between days and nights. Comparing weekdays and weekends, there was no difference in survival to hospital discharge, but there was an increase in survival to hospital discharge with favourable neurologic outcomes (using the alternate definition).
Table 4. Outcomes by time of day and day of week

n represents the total of patients in each group, and % represents the percentage of the patients who had that outcome (ROSC, ROC, SHD, SHD favourable neurological outcome).
We also performed a multivariable analysis that controlled for potential confounding factors of time of day, day of week, age category (compared to < 1 year of age), duration of event, illness category (surgical cardiac versus medical cardiac), interventions in place (end tidal carbon dioxide or indwelling arterial catheter) and initial rhythm (Table 5). We did not include extracorporeal membrane oxygenation in the multivariable model since extracorporeal membrane oxygenation was collinear with return of spontaneous circulation and return of circulation. Time of day and day of week were not associated with any outcome. There was, however, a significant association between the age category < 1 year compared to 8 to < 18 year and outcomes of return of spontaneous circulation (odds ratio 0.05 [0,0.65]; p = 0.02) and return of circulation (odds ratio 0.27 (0.08,0.95); p = 0.04). Cardiopulmonary resuscitation duration was significantly associated with return of spontaneous circulation (odds ratio 0.91 (0.88,0.94); p=<0.001) but not any other outcome. Although surgical cardiac patients were more likely to have an indwelling arterial catheter prior to onset of cardiac arrest, multivariable analysis showed surgical cardiac patients compared to medical cardiac patients were found to have improved survival to hospital discharge (odds ratio 4.22 (1.72,10.33); p = 0.002) and survival to hospital discharge with favourable neurologic outcome (using both definitions). Supplemental Table 5 displays the multivariable analysis of outcomes using the alternate definition of “day” and “night”. We did not include the presence of end tidal carbon dioxide monitoring or indwelling arterial catheter in this analysis because the sample size was too small (n = 88). When using the alternate definition of “day” and “night”, there were significant associations between day of week and survival to hospital discharge and survival to hospital discharge with favourable neurological outcome (alternate definition). Supplemental Table 6 displays the multivariable analysis of outcomes using the alternate definitions of “weekday” and “weekend.” When using the alternate definitions of “weekday” and “weekend,” there was higher survival to hospital discharge with favourable neurologic outcome (alternate definition) on weekdays compared to weekends, however no differences in any other outcomes.
Table 5. Multivariable analysis of outcomes

N=125 (7 events dropped given initial cardiac rhythm unknown). All values written as OR (95%CI)
Three important pre-arrest factors that indicate severity of illness were analysed within 2 hours of the event: lowest pH, highest lactate and vasoactive inotrope score. There was no significant difference between day and night or weekday and weekend with respect to pre-arrest lowest pH or highest lactate. There was a significant difference between pre-arrest vasoactive inotrope score: night vasoactive inotrope score = 10.0 (6.0,15.0) and day vasoactive inotrope score = 5.0 (2.0,7.0); p = 0.02. There was no difference with pre-arrest vasoactive inotrope score between weekday and weekend cardiac arrest events.
Two important elements of post-cardiac arrest care were analysed, temperature and systolic blood pressure. We evaluated each event for any documented systolic blood pressure measurement less than the 5th percentile for age within the first 6 hours after return of circulation, as well as any documented temperature greater than 38 degrees Celsius within the first 6 hours after return of circulation. There was no significant difference in the presence of fever or hypotension in events occurring during the day compared to night, or weekday compared to weeknight.
Discussion
It has previously been shown that children who have in-hospital cardiac arrest have improved survival to hospital discharge for those events occurring during the day compared to night and weekdays compared to weekends. Reference Bhanji, Topjian and Nadkarni6 Reference Christensen, Lee, Gowen, Rettiganti, Deshpande and Morray7 Reference Esangbedo, Yu and Raymond8 However, these differences were not significantly associated with disparities in chest compression quality. Reference Esangbedo, Yu and Raymond8 Reference Wolfe, Morgan and Sutton14 Whether using the primary or alternate definition of day/night, on univariate analysis there were no differences in outcomes between events during the day versus night (Table 4 and Supplementary Table 4). On multivariate analysis, using the primary definition of day/night, there was increased survival to hospital discharge on weekdays but no other differences in outcomes (Table 5). However, on multivariable analysis using the alternate definition of day/night (Supplemental Table 5), children with CHD have improved survival to hospital discharge and survival to hospital discharge with favourable neurologic outcome for index in-hospital cardiac arrest events occurring during weekdays compared to weekends, even after accounting for potential confounding factors of pre-arrest severity of illness, age category, initial ECG rhythm, duration of cardiopulmonary resuscitation, illness category (surgical cardiac versus medical cardiac), post-arrest blood pressure and temperature. However, there was no difference for events during day compared to night. Chest compression quality metrics were not different between events on days versus nights or weekdays versus weekends, and therefore would not explain outcome differences.
Pre-arrest factors indicating severity of illness and post cardiac arrest care were also not different between weekdays and weekends. When comparing event characteristics, the rate of extracorporeal cardiopulmonary resuscitation was more frequent during weekdays (47%) compared to weekends (18%) in our cohort, which could explain improved survival to hospital discharge and survival to hospital discharge with favourable neurologic outcome. The reasons for discrepancy in rates of extracorporeal cardiopulmonary resuscitation on weekends compared to weekdays remain unclear. Even though duration of cardiopulmonary resuscitation prior to cannulation for events occurring during day was shorter than at night, there was no significant differences in duration of cardiopulmonary resuscitation prior to cannulation for events during weekday compared to weekend. Although most hospitals have around the clock on call extracorporeal membrane oxygenation teams to emergently cannulate a patient, these teams are typically not on site on weekends. Thus, it was a surprising finding that in this cohort, duration of cardiopulmonary resuscitation prior to cannulation for events occurring during weekends and weekdays. It is possible that those patients who received extracorporeal cardiopulmonary resuscitation on weekends had similar duration of cardiopulmonary resuscitation on weekdays because the extracorporeal membrane oxygenation teams had already been on site at the start of the cardiac arrest and thus more prepared. Thus, if extracorporeal membrane oxygenation team members are not on site at the start of the cardiac arrest, this may influence the decision to forgo the use of extracorporeal cardiopulmonary resuscitation since there is a perception that delays to cannulation may ultimately affect long term outcomes. Future studies should analyse what factors lead to the decrease in the use of extracorporeal cardiopulmonary resuscitation for cardiac arrests on weekends.
Prior studies have shown improved survival to hospital discharge and better neurologic outcomes with the use of extracorporeal cardiopulmonary resuscitation compared to conventional cardiopulmonary resuscitation in children and adults. Reference Twohig, Singer, Grier and Finney19 Reference Lasa, Rogers and Localio20 However, prior studies in children and adults analysing the association between outcomes with extracorporeal cardiopulmonary resuscitation and time of day and day of week have shown conflicting results. A study by Lee et al analysed outcomes of adults in a single centre undergoing extracorporeal cardiopulmonary resuscitation and found improved outcomes for those undergoing extracorporeal cardiopulmonary resuscitation during the weekday compared to weekend. Reference Lee, Chung and Jeon21 A study by Lunz et al. analysed outcomes of adult patients who had extracorporeal cardiopulmonary resuscitation in a single centre, and found that although patients with events occurring on weekends compared to weekdays did not affect survival to hospital discharge, it did affect long-term survival. Reference Lunz, Camboni and Philipp22 A study by Burke et al. analysed outcomes of children in a single centre undergoing extracorporeal cardiopulmonary resuscitation and found that although events occurring on nights and weekends had higher rates of neurologic injury, there were no differences in survival or neurologic outcome. Reference Burke, Chan, Brogan and McMullan13
It is unclear why there was a lack of improved outcomes when comparing day versus night in our study as seen in prior studies of the general paediatric population with in-hospital cardiac arrest. However, it may be related to the fact that there was a similar rates of extracorporeal cardiopulmonary resuscitation use on days versus nights in our study. This is different than the study by Tonna et al. which was an observational study of adult extracorporeal cardiopulmonary resuscitation events using the American Heart Association’s Get with the Guidelines-Resuscitation Registry and showed a decreased use of extracorporeal cardiopulmonary resuscitation after-hours and weekends. Reference Tonna, Selzman and Girotra23
It is also possible that the improved outcomes associated with weekday events are not related to extracorporeal cardiopulmonary resuscitation use, but rather other factors that we did not study, such as unit staffing and provider experience. On weekends compared to weekdays, hospitals usually have lower numbers of staff as well as less experienced staff. It is possible that these staffing model differences may affect multiple aspects of peri-arrest care which can affect outcomes. Reference Gaies, Clarke, Donohue, Gurney, Charpie and Hirsch16 In the pre-arrest phase, while a more experienced nurse may be able to detect subtle changes earlier and prevent a cardiac arrest, there are some events that cannot be prevented. For those events that are unpreventable, an experienced nurse earlier detection of impending arrest may result in earlier mobilisation of providers to prepare for the cardiac arrest leading to a more successful resuscitation. A more experienced nurse and provider may also deliver improved post-cardiac arrest care. Although our study did not show any differences between events occurring on weekends compared to weekdays in two important elements of post cardiac arrest care: fever or hypotension, there were many variables in post cardiac arrest care that were not evaluated.Reference Topjian, de Caen and Wainwrigt 24 Although our study did not analyse staffing models during events, future studies should evaluate this important factor. Although nursing experience may be one important factor, the results of a study by Gaies et al showed that the “weekend effect” may not be solely explained by nursing experience. Reference Gaies, Clarke, Donohue, Gurney, Charpie and Hirsch16 Their study showed that the odds of unsuccessful resuscitation from cardiac arrest in a single centre paediatric cardiac intensive care unit increased for those events occurring on weekends compared to weekdays but not night compared to days. Multivariate analysis showed that weekend and experience level of the nurse were independent predictors of unsuccessful resuscitation. Although the quantity of cardiac ICU staff is typically less on weekends, differences in staffing models outside the ICU may also affect the care of patients within the ICU. Compared to weekdays, decreased staff on weekends may result in delays in diagnostic tests, access to specialists and procedures which can ultimately affect patient outcomes. Future studies should analyse the different factors inside and outside of the intensive care unit that result in worse outcomes on weekends since this may improve outcomes.
In multivariable analysis using alternate definitions of day/night (Supplemental Table 5), we also found a significant association of age category < 1 year of age (compared to 8 to <18 years of age) with return of spontaneous circulation, return of circulation, survival to hospital discharge and survival to hospital discharge with favourable neurologic outcome. Prior studies have shown that among children who have in-hospital cardiac arrest, infants < 1 year of age have improved outcomes compared to older children. Reference Donoghue, Nadkarni and Berg4,Reference Meaney, Nadkarni and Cook25 It is unclear the reasons for improved outcomes in younger children, but Meaney et al hypothesised that it could be secondary to more compliant chest walls of younger children leading to better systemic perfusion during cardiopulmonary resuscitation. Reference Meaney, Nadkarni and Cook25 While our study analysed chest compressions quality metrics, we did not analyse haemodynamics (arterial pressure, end tidal carbon dioxide, etc.) during chest compressions. Supplemental Tables 1 and 2 show that the percentage of events requiring extracorporeal cardiopulmonary resuscitation in the < 1-year group is less than the 8 to < 18-year group, and thus increased use of extracorporeal membrane oxygenation cannot be the reason for improved outcomes.
We also found a significant association of patients with surgical cardiac illness category compared to medical cardiac illness category had improved survival to hospital discharge and survival to hospital discharge with favourable neurological outcome, whether we used the primary or alternate definition of day/night. As mentioned before, surgical cardiac illness category compared to medical cardiac illness category patients were more likely to have end tidal carbon dioxide monitoring in place, which may explain improved outcomes. However, multivariable analysis demonstrated that even after controlling for the presence of invasive monitoring before the onset of cardiac arrest, surgical cardiac illness category was independently associated with improved outcomes (Table 5). As discussed above, we were unable to control for the confounder of extracorporeal membrane oxygenation use, and we know that the incidence is higher in surgical compared to medical cardiac patients. Our findings are similar to multiple prior studies that have shown patients with a diagnosis of surgical heart disease compared to medical heart disease have better outcomes after in-hospital cardiac arrest. Reference Lowry, Knudson, Cabrera, Graves, Morales and Rossano15,Reference Alten, Klugman and Raymond26,Reference Ortmann, Prodhan and Gossett27
Limitations
There are some limitations to our study. The cardiac arrest events in this report of the pediRes-Q Collaborative are ones of sufficient duration that the team had time to place the defibrillator pads on the patient. Short duration cardiac arrest events that achieved return of spontaneous circulation before the pads could be placed were not included. Thus, our data may be skewed toward events that are longer in duration, and thus having worse outcomes. It is possible that brief events that are rapidly recognised and with immediate return of spontaneous circulation could be disproportionately distributed by time of day or day of week. Another limitation is that while there were 21 hospitals contributing data to this study, 45% of the cardiac arrest events were reported by two centres. We acknowledge that hospitals who contribute to the collaborative may be a skewed representation of centres who are dedicated to improving cardiopulmonary resuscitation quality in children.
Conclusions
In a large multi-centre international paediatric resuscitation collaborative, children with CHD and in-hospital cardiac arrest of sufficient duration to place defibrillator electrode pads to monitor chest compression metrics, there was no significant difference in chest compression quality metrics by time of day or day of week. There was no significant difference in return of spontaneous circulation or return of circulation by time of day or day of week; however, there was improved survival to hospital discharge and survival to hospital discharge with favourable neurological outcome for events occurring on weekdays compared to weekends. This difference may be related to the increased use of extracorporeal cardiopulmonary resuscitation on weekdays versus weekends in this paediatric patient cardiac population.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1047951122000099
Acknowledgements
We would like to thank the teams of clinicians and quality improvement/research staff that invested time, effort and enthusiasm in this collaborative effort. We would like to thank Annemarie Silver, PhD, from ZOLL Medical for her valuable contributions and unique insights into paediatric chest compression metrics. The concept and development of the resuscitation clinical learning laboratory collaboration would not have been possible without the generous and unrestricted educational grant support of Laerdal Medical (2006-2013) and ZOLL Medical (2014-2021).
Financial Support
The pediRES-Q Collaborative is supported by an unrestricted research grant from ZOLL Medical Corporation.
Conflict of Interest
Dana Niles and Vinay Nadkarni disclose that The Children’s Hospital of Philadelphia received support from an unrestricted research grant from ZOLL Medical. Dana Niles and Vinay Nadkarni disclose that The Children’s Hospital of Philadelphia receives funding from an unrestricted research grant from The American Heart Association. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Appendix 1:
The pediRES-Q Collaborative Investigators : Kamal Abulebda , Riley Hospital for Children, Indianapolis, IN, US; Diane Atkins , University of Iowa Stead Family Children’s Hospital, Iowa City, IA, US; Shilpa Balikai , University of Iowa Stead Family Children’s Hospital, Iowa City, IA, US; Marc Berg , Lucile Packard Children’s Hospital, Palo Alto, CA, US; Robert Berg , The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Utpal Bhalala , Children’s Hospital of San Antonio, San Antonio, TX, US; Matthew S. Braga , Dartmouth-Hitchcock Medical Center, Lebanon, NH, US; Corinne Buysse , Erasmus MC–Sophia Children’s Hospital, Rotterdam, NL; Corrado Cecchetti , Ospedale Pediatrico Bambino Gesù, Rome, IT; Adam Cheng , Alberta Children’s Hospital, Calgary, AB, CA; Andrea Christoff , Children’s Hospital at Westmead, Sydney, NSW; Kelly Corbett , Dartmouth-Hitchcock Medical Center, Lebanon, NH, US; Allan DeCaen , Stollery Children’s Hospital, Edmonton, AB, CA; Gabry deJong , Erasmus MC–Sophia Children’s Hospital, Rotterdam, NL; Jimena del Castillo , Hospital Maternoinfantil Gregorio Marañón, Madrid, ES; Maya Dewan , Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, US; Aaron Donoghue , The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Jordan Duval-Arnould , Johns Hopkins University School of Medicine, Baltimore, MD, US; Ivie Esangbedo , UT Southwestern Dallas Children’s Medical Center, Dallas, TX, US; Michael Flaherty , Massachusetts General Hospital, Boston, MA, US; Stuart Friess , St. Louis Children’s Hospital, St. Louis, MO, US; Sandeep Gangadharan , Mount Sinai Kravis Children’s Hospital, New York, NY, US; Orsola Gawronski , Ospedale Pediatrico Bambino Gesù, Rome, IT; Jonathan Gilleland , Alberta Children’s Hospital, Calgary, AB, CA; Heather Griffis , Healthcare Analytics Unit, The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Richard Hanna , The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Helen Harvey , Rady Children’s Hospital, San Diego, CA, US; Ilana Harwayne-Gidansky , Stony Brook Hospital, Stony Brook, NY, US; Sarah Haskell , University of Iowa Stead Family Children’s Hospital, Iowa City, IA, US; Jennifer Hayes , Children’s Hospital of Orange County, Los Angeles, CA, US; Kiran Heber , Children’s Healthcare of Atlanta, Atlanta, GA, US; Betsy Hunt , Johns Hopkins University School of Medicine, Baltimore, MD, US; Takanari Ikeyama , Aichi Children’s Health and Medical Center, Obu, Aichi, JP; Priti Jani , The University of Chicago Medicine Comer Children’s Hospital, Chicago, IL, US; Kaitlin Jones , Children’s Healthcare of Atlanta, Atlanta, GA, US; Monica Kleinman , Boston Children’s Hospital, Boston, MA, US; Lynda Knight , Lucile Packard Children’s Hospital Stanford, Palo Alto, CA, US; Hiroshi Kurosawa , Hyogo Prefectural Kobe Children’s Hospital, Kobe, Hyogo, JP; Javier Lasa , Texas Children’s Hospital, Houston, TX, US; Kasper Glerup Lauridsen , The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Aarhus University Hospital, Aarhus, DK; Tara Lemoine , Valley Children’s Hospital, Madera, CA, US; Tensing Maa , Nationwide Children’s Hospital, Columbus, OH, US; Dori-Ann Martin , Alberta Children’s Hospital, Calgary, AB, CA; Elizabeth Masse , Seattle Children’s Hospital, Seattle, WA, US; Luz Marina Mejia , Instituto de Ortopedia Infantil Roosevelt, Bogota, CO; Michael Meyer , Children’s Hospital of Wisconsin, Milwaukee, WI, US; Yee Hui Mok , KK Women’s & Children’s Hospital, SG; Ryan Morgan , The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Vinay Nadkarni , The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Sholeen Nett , Dartmouth-Hitchcock Medical Center, Lebanon, NH, US; Dana Niles , The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Michelle Olson , Children’s Hospital of Richmond, Richmond, VA, US; Tara Petersen , Children’s Hospital of Wisconsin, Milwaukee, WI, US; Gene Ong , KK Women’s & Children’s Hospital, SG; Prakad Rajapreyar , Children’s Hospital of Wisconsin, Milwaukee, WI, US; Tia Raymond , Medical City Children’s Hospital, Dallas, TX, US; Joan Roberts , Seattle Children’s Hospital, Seattle, WA, US; Lindsay Ryerson , Stollery Children’s Hospital, Edmonton, AB, CA; Anita Sen , NewYork-Presbyterian Morgan Stanley Children’s Hospital, New York, NY, US; Marcy Singleton , Dartmouth-Hitchcock Medical Center, Lebanon, NH, US; Sophie Skellet , Great Ormond Street Hospital, London, UK; Daniel Stromberg , Dell Children’s Medical Center, Austin, TX, US; Felice Su , Lucile Packard Children’s Hospital Stanford, Palo Alto, CA, US; Robert Sutton , The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Todd Sweberg , Cohen Children’s Medical Center, New Hyde Park, NY, US; Oscar Tegg , The Children’s Hospital at Westmead, Sydney, NSW; Ken Tegtmeyer , Cincinnati Children’s Hospital, Cincinnati, OH, US; Alexis Topjian , The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Wendy Van Ittersum , Akron Children’s Hospital, Akron, OH, US; Javier Urbano Villaescusa ; Hospital Maternoinfantil Gregorio Marañón, Madrid, ES; Ichiro Watanabe , Tokyo Metropolitan Children’s Hospital, Fuchū, Tokyo, JP; Denise Welsby , Great Ormond Street Hospital, London, UK; Jesse Wenger , Seattle Children’s Hospital, Seattle, WA, US; Heather Wolfe , The Children’s Hospital of Philadelphia, Philadelphia, PA, US; Andrea Yeo , National University Children’s Medical Institute, SG; Priscilla Yu , UT Southwestern Dallas Children’s Medical Center, Dallas, TX, US.









