No CrossRef data available.
Article contents
EPA-0022 – Diagnosis of Diabetes and Obesity Have no Impact on Six Month Remission Rates for Depressed Primary Care Patients
Published online by Cambridge University Press: 15 April 2020
Abstract
Prior studies have demonstrated an inter-relationship between the diagnosis of diabetes, obesity and depression. Our data has demonstrated that baseline body mass index (BMI) was not predictive for clinical outcomes (remission at six months).
Our hypothesis was that obesity (BMI ≥30) and the diagnosis of diabetes in depressed primary patients would have no effect on depression remission rates six months after diagnosis.
This study was retrospective analysis of 1, 894 primary care patients diagnosed with Major Depressive Disorder or Dysthymia with a PHQ-9 score of 10 or greater.
▪ Outcome variable was clinical remission (PHQ-9 < 5) at six months.
▪ Logistic regression modeling included the demographic variables of age, gender, marital status, the clinical variables of BMI, baseline PHQ-9 score, diagnosis of diabetes (yes/no) and clinical diagnosis (recurrent or first episode of depression, or dysthymia).
Figure 1
Odds ratio for clinical remission (PHQ-9<5) at six months in depressed primary care patients, by variable (N=1,894).
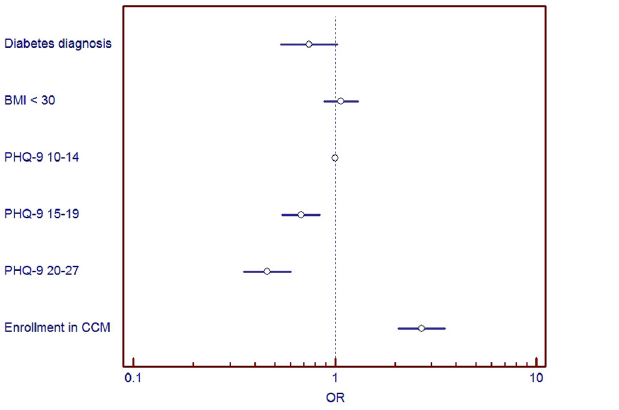
Controlling for age, gender, marital status, race, clinical diagnosis and clinical site with logistic regression modeling.
▪ Baseline obesity was not an independent predictor for depression outcome at six months.
▪ Diagnosis of diabetes was not an independent predictor for depression outcome at six months.
This data suggests that obesity and diabetes were not associated with worsening clinical outcomes in depression management.
- Type
- EPW02 - Depression 1
- Information
- Copyright
- Copyright © European Psychiatric Association 2014



Comments
No Comments have been published for this article.