Background
Candida auris is an emerging multidrug-resistant fungal pathogen that is increasingly recognized as a cause of healthcare-associated infections and outbreaks in healthcare settings. The first few cases in the United States were described in 2016 following an alert issued by the Centers for Disease Control and Prevention (CDC), with subsequent spread in healthcare settings associated with a high burden of colonization among individuals in ventilator-capable skilled nursing facilities (SNFs). Reference Vallabhaneni, Kallen and Tsay1,Reference Rossow, Ostrowsky and Adams2 The first case-patient of C. auris transmission in Maryland was identified in June 2019.
The ability of C. auris to colonize the skin of individuals as well as contaminate the surrounding environment contributes to transmission in congregative settings. Reference Biswal, Rudramurthy and Jain3,Reference Eyre, Sheppard and Madder4 Prior outbreaks have been attributed to poor existing infection control practices including poor hand hygiene, inadequate environmental cleaning, and lack of proper disinfection agents. Reference Karmarkar, O’Donnell and Prestel5 Existing research has highlighted individual patient risks factors associated with C. auris colonization including mechanical ventilation, antifungal treatment, prior frequent hospitalizations and residence in SNF. Reference Rossow, Ostrowsky and Adams2
Other emerging infectious diseases, including COVID-19 and Mpox, have disproportionately affected vulnerable communities, and there is growing interest in examining health disparities in healthcare-associated infections as well as underlying systemic structural contributors to antimicrobial resistance. Reference Philpott, Hughes and Alroy6,Reference Tipirneni, Schmidt, Lantz and Karmakar7 One case–control study from 2016 to 2018 in New York among 60 C. auris case-patients residing in ventilated capable SNFs noted that residents with and without C. auris did not differ by age, sex, or race/ethnicity. Reference Rossow, Ostrowsky and Adams2 However, measures of socioeconomic vulnerability – at either the individual or facility-level - have not yet been systematically evaluated among patients who are infected or colonized with C. auris. There is also a lack of data on which neighborhood socioeconomic characteristics and vulnerability indices can accurately identify infectious disease risk in SNFs.
Recent studies have recognized that neighborhood deprivation is associated with gaps in staffing and resources, Reference Falvey, Hade and Friedman8 which may preclude implementation of optimal infection control practice. This may be compounded by intersectionality between individual- and facility-level disadvantages, producing greater vulnerability than either, by itself. For example, an individual with medical risks that are unaddressed due to poor access to care may also reside in a SNF with greater disadvantage. There are opportunities for using both quantitative and qualitative findings together to provide a better groundwork for sustainable intervention. Reference Jeleff, Lehner and Giles-Vernick9
In this study, we describe characteristics of patients and facilities with C. auris in the state of Maryland with a focus on socioeconomic vulnerabilities. In this exploratory work, we evaluate the association of two different vulnerability indices and their association with C. auris risk at both the individual level and facility level. We also describe findings from infection control assessments conducted in Maryland facilities suspected of having C. auris transmission. Finally, we propose a conceptual model that combines patient-level and facility-level medical and social vulnerabilities in the transmission of this pathogen and thus may provide direction for future prevention and control strategies.
Methods
We conducted a mixed-methods study to characterize the emergence of C. auris in the state of Maryland from 2019 to 2022, with a focus on socioeconomic vulnerability and infection prevention opportunities.
During this period, the Maryland Department of Health (MDH) investigated all C. auris-positive clinical and surveillance cultures through basic epidemiologic methods including contact tracing for additional case finding. Infection control programs of healthcare facilities with suspected C. auris transmission were assessed by MDH using a state-specific Infection Control Assessment and Response (ICAR) tool modified from the CDC ICAR tool. 10
We first performed a descriptive analysis of all case-patients of C. auris identified in Maryland from June 2019 to December 2021. We defined case-patients as any individual >18 years old that had C. auris detected on either a clinical or surveillance (screening) sample obtained at a Maryland healthcare facility. Screening or surveillance C. auris specimens, consisting of composite axilla/groin skins swabs obtained during point prevalence colonization screenings, were tested via polymerase chain reaction by the Maryland Public Health Laboratory (MDPHL). Clinical C. auris case-patients were identified by culture from different body sites during routine clinical care and reported to the health department.
Clinical information on potential patient-level risk factors was obtained from healthcare facilities and from the Chesapeake Regional Information System for our Patients (CRISP).
Socioeconomic inequalities and their relationship to poor health outcomes have been described using vulnerability indices including the social vulnerability index (SVI) and the area deprivation index (ADI). The ADI is a publicly available measure created to define neighborhood socioeconomic status at the census block-group level based on 17 domains representing poverty, education, and housing with data from the United States Census and the American Community Survey. Reference Kind and Buckingham11,12 The CDC SVI tool Reference Flanagan, Hallisey, Adams and Lavery13,14 is a measure created to identify socially vulnerable populations at the census tract level based upon 16 social factors divided into four distinct themes: (1) socioeconomic status, (2) household characteristics, (3) racial and ethnic minority status, and (4) housing type and transportation. Both ADI and SVI are expressed as percentile calculated at either the state or national level. State-level percentiles were utilized in this study for better discrimination. State ADI ranges from 1 to 10 and SVI 1–100, with higher percentiles indicating greater socioeconomic disadvantage. We split the ADI into quintiles and SVI into quartiles to better analyze and characterize the distribution of patients given the nonlinear effects. We defined severely disadvantaged as neighborhoods noted to be within the top quintile of deprivation (ADI ≥ 8) of ranking for ADI and census tracts noted to be in the top quartile (SVI ≥ 75) of ranking for SVI. Data obtained were from the 2020 ADI and SVI Index which both draw from American Community Survey 2020 encompassing 5-year data 2016–2020.
We obtained patient home addresses from CRISP and utilized the latest address prior to detection of C. auris. Addresses associated with SNF case-patients were replaced by their addresses before admission to a facility. Case-patient addresses and SNF addresses were geocoded and assigned both a census tract and census block to calculate the SVI and ADI, respectively. The average ADI of the surrounding blocks was used for SNFs located in areas without a designated ADI.
We summarized patient and SNF characteristics using descriptive statistics. We compared characteristics of SNFs with and without identified C. auris transmission using χ2 test for categorical variables. Transmission was defined as ≥ 2 epidemiologically linked case-patients at the same SNF. All statistical analyses were completed using STATA.
From June 2019 to December 2022 the MDH Infection Prevention and Control (IPC) team, consisting of nurses, physicians, and public health professionals, conducted ICARs at 12 unique SNFs with confirmed transmission of C. auris from June 2019 to December 2022. ICARs included prevention and control audit tools tailored to Maryland facilities that included the following domains: hand hygiene, staffing, environment of care, environmental services, and wound care. We subsequently analyzed the source text documents containing those ICAR reports using Nvivo 11 (QSR International, Burlington, MA) for qualitative content analysis. Four IPC experts performed conventional content analysis on two randomly selected assessments to create a coding manual based upon common infection control observations. One reviewer manually coded the assessments and categorized emergent themes into overarching infection control domains and subthemes supported by the strongest observations.
This study was determined as exempt by the MDH institutional review board.
Results
Epidemiologic analysis
Individual case-patient-level analysis
Between June 2019 and December 2021, 140 individuals tested positive for C. auris in Maryland. Of these, 119 (85%) were detected by the MDPHL, while 21 case-patients were detected through testing at other laboratories. Of a total 144 samples positive for C. auris, the most common samples were axilla/groin surveillance swabs (99), blood cultures (16), urine cultures (14), and wound cultures (4). Overall, 46 (33%) of case-patients had a positive clinical culture during this period. The overall positivity rate among total 4499 surveillance (screening) tests for C. auris submitted to the MDPHL during this period was 2.7%.
The median age of C. auris case-patients was 68 years (IQR 53–74), and 91 (65%) were male. Sixty (43%) case-patients were residents of SNFs; 37 (26%) were mechanically ventilated, 87 (62%) had a documented wound, 49 (35%) had a documented feeding tube, and 29 (21%) had central lines in place. Thirty-nine of 140 (28%) case-patients died within 90 days of a positive C. auris test. Case-patients had home addresses from 7 different states; 122 (87%) had a home address in the state of Maryland. Of 116 individuals with an identifiable home street address in Maryland, the median state ADI was 6 (IQR 4–8). Thirty-three (28%) of case-patient home addresses were located in areas in the top quintile of deprivation based on state ADI (ADI> = 8). Statewide estimates for SVI showed that C. auris case-patient home addresses had a median SVI in the 68th percentile (IQR 37–85), with 47 (41%) located in areas in the top quartile of deprivation (SVI> = 75) (Table 1).
Table 1. Percentage of individuals with C. auris colonization or infection who resided in severely disadvantaged neighborhoods by theme. Severely disadvantaged was defined as the top quartile of disadvantage (SVI> = 75) within the state

Skilled nursing facility-level analysis
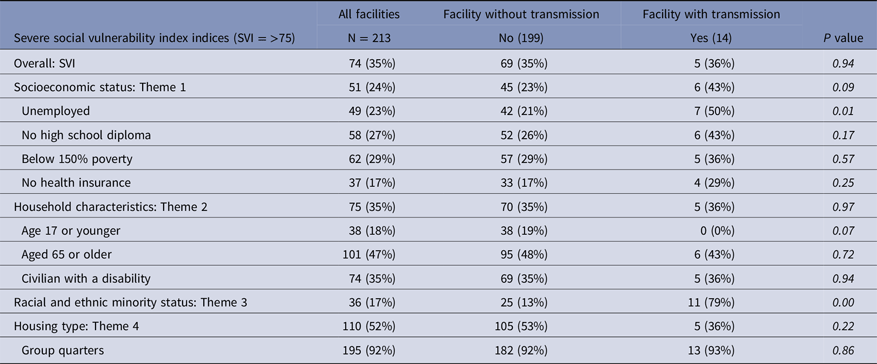
Fifteen SNFs had likely transmission of C. auris between June 2019 and December 2022. Fifty percent (8/16) of ventilator-capable SNFs had noted transmission compared to 3% (7/209) of SNFs without ventilator capability. ADI was available for 212 SNFs including all 15 with noted C. auris transmission. The Maryland state median ADI of all 212 SNFs was 6 (IQR 5). Based on ADI, 31% of all Maryland SNFs and 40% of all Maryland ventilator-capable SNFs are located in the top quintile of deprivation (ADI> = 8). There was no statistically significant difference in ADI between SNFs with and without C. auris transmission. Data on SVI was available for 213 SNFs including 14 with noted C. auris transmission. Based on SVI, 35% of all Maryland SNFs are located in areas in the top quartile of deprivation. The overall proportion of severe SVI between SNFs with and without C. auris transmission did not differ. However, SNFs with C. auris transmission were significantly more likely to be located in areas in the top quartile of deprivation due to unemployment and minority status, compared to SNFs without identified transmission (Table 2).
Table 2. Comparison of severe social vulnerability index (SVI> = 75) between skilled nursing facilities with and without identified C. auris transmission
Qualitative analysis: ICARs
Twelve of 15 SNFs with confirmed C. auris transmission had assessments available to be analyzed. Observations on hand hygiene revealed inconsistent access to alcohol-based hand rub and missed opportunities for hand hygiene. Education of staff surrounding C. auris was often lacking with notable gaps. Wound care observations were remarkable for lack of consistent use of aseptic technique and potentially contaminated supplies taken out of patient rooms at multiple facilities. Review of environmental cleaning processes revealed gaps in multiple areas including high-touch surfaces, maintenance, availability of cleaning supplies, and proper contact time (Table 3).
Table 3. Summary of findings from infection control and response audits of skilled nursing facilities with C. auris transmission (N = 12)

Discussion
In this mixed-methods study of the first 140 C. auris case-patients identified in the state of Maryland, we found both individual-level and facility-level indices of neighborhood socioeconomic vulnerability to be associated with C. auris. Case-patient residence in SNFs and presence of wound(s) were frequent, and infection control deficiencies in SNFs were identified.
In our individual-level analysis of neighborhood characteristics of C. auris case-patients in Maryland, we found that this cohort belonged to neighborhoods that are less insured, have lower socioeconomic status and higher concentrations of racial/ethnic minorities, relative to the Maryland average. Similarly, 28% of case-patients resided in neighborhoods that were in the top quintile of deprivation by the ADI, a measure that describes socioeconomic disadvantage. However, it is unclear if these findings of somewhat higher socioeconomic vulnerability relative to the state average are specific to the case-patients’ C. auris status or represents individuals with healthcare contact.
For methicillin-resistant Staphylococcus aureus (MRSA), neighborhood characteristics such as poverty, lack of education, and access to health care at the census tract level are associated with racial disparities in MRSA infections. Reference See, Wesson and Gualandi15 Neighborhood deprivation and socioeconomic disadvantage have also previously been linked to increased risk of readmission and frequent contact with healthcare facilities which are risk factors for C. auris. Reference Kind, Jencks and Brock16
Prior research has shown that individual-level patient characteristics, such as membership in marginalized groups that experience structural racism and ageism, contributed to poor health outcomes during the COVID-19 pandemic in SNFs. Reference Abrams, Loomer, Gandhi and Grabowski17 More research needs to be done to understand the role of individual risk factors in addition to the neighborhood risk factors that may contribute to multidrug-resistant organism (MDRO) transmission.
When evaluating socioeconomic vulnerability at the facility-level, we found that one-third of all SNFs were in areas with severe disadvantages. In addition, SNFs in neighborhoods with lower socioeconomic status and high numbers of racial minorities were more likely to experience C. auris transmission. Prior research shows that SNFs in socioeconomically disadvantaged neighborhoods have less staff, lower quality ratings, and more financial strain. Reference Falvey, Hade and Friedman8,Reference Yuan, Louis, Cabral, Schneider, Ryan and Kazis18,Reference Park and Martin19 Future research should clarify the relationship between SNF neighborhood socioeconomic disadvantages and differential environmental exposure or built environment that could contribute to MDRO outbreaks and infection control deficiencies.
Our findings on the clinical characteristics of C. auris case-patients are similar to those from previous studies that showed most patients infected or colonized with C. auris had multiple comorbidities. Reference Eyre, Sheppard and Madder4,Reference Adams, Quinn and Tsay20 Particularly, patients were noted to require ventilation, central lines, wound care, and feeding tubes. Many also had extensive prior contact with healthcare facilities which has been shown to be a risk factor for infection. Reference Rossow, Ostrowsky and Adams2,Reference Caceres, Rivera and Armstrong21 Almost half of Maryland case-patients were directly associated with SNFs. Additionally, C. auris outbreaks disproportionately occurred in SNFs with ventilator-capable units and infection control practices in SNFs with outbreaks had notable deficiencies. Prior research has highlighted the role that long-term care facilities have played in driving transmission in group settings, particularly in ventilator-capable SNFs. Reference Pacilli, Kerins and Clegg22
ICARs were completed at multiple SNFs with ongoing transmission of C. auris, and common themes emerged. Poor hand hygiene adherence was noted at multiple SNFs and audits were not routinely performed by infection control staff. Many SNFs were not using appropriate disinfectants for C. auris, noting that there was inconsistent access to cleaning supplies throughout the SNF. Staff including environmental services were not always aware of correct cleaning processes and infection control policies. These observations are consistent with prior infection control assessments during C. auris outbreaks and further support the role that strong IPC practices serve in preventing and stopping the spread of infection. Reference Karmarkar, O’Donnell and Prestel5,Reference Aldejohann, Wiese-Posselt, Gastmeier and Kurzai23,Reference Caceres, Forsberg and Welsh24
We observed that many patients in this study had wounds that required wound care. Prior studies have noted that a substantial proportion of C. auris case-patients had documented wounds. Reference Karmarkar, O’Donnell and Prestel5,Reference Pacilli, Kerins and Clegg22 This prompted attention to wound care practices during infection control observations conducted by the MDH IPC team, and lapses in proper infection control during delivery of wound care were observed frequently. Although the relative contribution of risk of colonization due to the presence of wounds and the risk of transmission due to infection control lapses during provision of wound care remains unclear, these findings are consistent with previous studies on other MDROs and suggest the need for focused attention to wound presence and care. Reference van Buul, van der Steen and Veenhuizen25,Reference McKinnell, Miller, Eells, Cui and Huang26
This study has several notable limitations. Although we found high comorbidity and higher than expected socioeconomic vulnerability relative to the state average in C. auris case-patients, we did not compare individuals with C. auris to a control group without C. auris. Further, this cohort does not include all case-patients occurring during the period under review; it is likely that additional case-patients of C. auris went undetected due to limitations in existing laboratory or epidemiological methods, and while MDH used an aggressive approach to case-patient finding during this period, this also led to surveillance bias toward increased detection in SNFs with initial case-patients. Despite these limitations, we believe that these data suggest a complex interplay between individual- and facility-level neighborhood vulnerability due to both socioeconomic and medical characteristics (Figure 1). Medical conditions that are risk factors for acquisition of C. auris or other MDROs may be more prevalent in individuals who are marginalized; these individuals may be more likely to be residents of SNFs that are less able to halt the spread of emerging pathogens due to inadequate resources. Therefore, although infection control opportunities can be identified and addressed in real time in response to transmission and outbreaks, these responses may be short-lived and inadequate. That similar risk factors exist for both risk of infection and MDRO transmission across time and geographic regions suggests that unless underlying systemic factors are addressed, we are likely to see limited success in control of these organisms and to see a replacement of one organism with another in the same vulnerable groups. A longer-term approach to preventing infectious disease transmission and emergence will require policy solutions based on a critical evaluation of underlying socioeconomic vulnerability and targeted, commensurate allocation of resources.

Figure 1. Conceptual model of C. auris transmission.
Acknowledgments
This work is supported by the Leaders in Epidemiology, Antimicrobial Stewardship and Public Health Fellowship.
Financial support
No financial support was provided for this manuscript.
Competing interests
All authors report no conflicts of interest relevant to this manuscript.







