To the Editor—We read with great interest the article by Wang et al Reference Wang and Yu1 and the study by Cheng et al Reference Cheng, Wong and Chen2 that highlighted the vital role of N95 respirators for preventing SARS-CoV-2 transmission and COVID-19 among healthcare workers (HCWs). The protective role of N95 respirators in other respiratory diseases could be translated to tackle the COVID-19 pandemic. Reference Wang and Yu1 Preliminary results in Hong Kong demonstrated that the use of N95 respirators for triage, for medical care of suspected or confirmed cases and during aerosol-generating procedures, drastically reduced COVID-19 infection among HCWs. Reference Cheng, Wong and Chen2 We acknowledge that the effectiveness of N95 respirators to prevent SARS-CoV-2 transmission should be confirmed and their use in clinical practice should be supported during the COVID-19 pandemic. However, we are facing a scenario of global shortage in availability of personal protective equipment (PPE), including surgical masks and N95 respirators. Reference Feng, Shen, Xia, Song, Fan and Cowling3 Countries are in dispute over the insufficient number of manufacturers. With unfair markets and increasing prices, low- and middle-income countries are at risk of losing their ability to acquire PPE for their HCWs. Several studies have previously reported methods for PPE decontamination Reference Lemmer, Howaldt and Heinrich4 or reuse of N95 respirators. Reference Lin, Tang, Hung, Hua and Lai5
Globally, the discussion by health authorities regarding new approaches to managing the N95 respirator shortage is urgent. The extended use or reuse and/or implementation of decontamination methods of N95 respirators might be an alternative that can prevent SARS-CoV-2 transmission among HCWs during the COVID-19 pandemic. Therefore, we have summarized recommendations regarding the extended use or reuse of N95 respirators, and we provide an overview of published information by regulatory authorities, surveillance organizations, and ministries of health of several countries.
Two researchers independently scrutinized the websites of the regulatory authorities of countries or regions and of ministries of health that a members or associates of the International Coalition of Medicines Regulatory Authorities (ICMRA). 6 Following the screening of information up to April 10, 2020, information from each country or region was collected in an electronic database. We collected the date of publication and information and excerpts from the guidance document regarding the recommendations for extended and reuse of N95 masks or filtering face pieces (FFPs). Extended use was defined as use for longer periods without removing the respirator (eg, treating several patients or working for >1 shift without interruption), and reuse indicated that the respirator was removed, stored, and used at least 1 more time. 7
Overall, 27 countries or regions were screened: 5 countries (19%) only allowed extended use (Canada, France, Mexico, New Zealand and Sweden); 2 countries (7%) mentioned only reuse (Germany and Netherlands); and 3 countries (11%) recommended both strategies for rationing N95 respirators (Brazil, European region and the United States). No information was available on extended use or reuse of N95 respirators in the websites of 17 countries (63%). Some countries (Germany and Netherlands) recommended specific methods for N95 respirators decontamination, and others (Europe and United States) mentioned several options, leaving the decision to health services managers (Table 1). The following decontamination methods were mentioned: dry heat in a drying cabinet at 65–70°C (Germany); vaporous hydrogen peroxide (Netherlands, Europe, and the United States); ultraviolet germicidal irradiation and moist heat (Europe and the United States). The maximum duration of extended used ranged from 4 hours (France, New Zealand, and Sweden) to 40 hours (Mexico), and the maximum number of cycles of decontamination ranged from 2 (Germany) to 5 (United States).
Table 1. Recommendations for Extended Use or Reuse of N95 Respirators Among Health Professionals During COVID-19 Pandemic by Country and Regulatory Authority, 2020
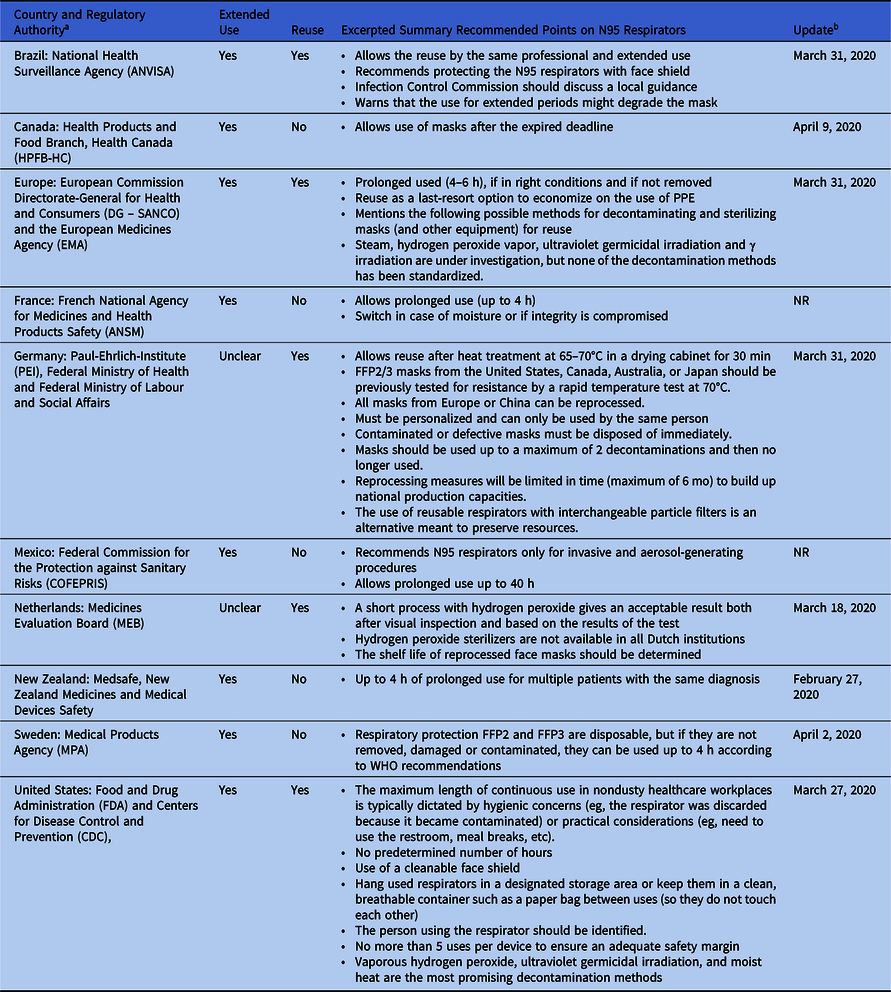
Note. NR, not reported; FFP, filtering face piece.
a Countries, Regulatory Authority, for which was not possible to find specific recommendations related to N95 respirators: Australia, Therapeutic Goods Administration (TGA); Austria, Austrian Medicines and Medical Devices Agency (AGES MEA), Austrian Federal Office for Safety in Health Care; China, China Food and Drug Administration (CFDA); Denmark, Danish Medicines Agency; India, Ministry of Health and Family Welfare; Ireland, Health Product Regulatory Authority (HPRA); Italy, Italian Medicines Agency (AIFA); Japan, Pharmaceuticals and Medical Devices Agency (PMDA), and the Ministry of Health, Labour and Welfare (MHLW); Korea, Ministry of Food and Drug Safety (MFDS); Nigeria, National Agency for Food Drug Administration and Control (NAFDAC); Poland, The Office for Registration of Medicinal Products, Medical Devices and Biocidal Products (URPLWMiPB); Russia, Federal Service for Surveillance in Healthcare (Roszdravnadzor); Singapore, Health Sciences Authority Singapore (HSA); South Africa, Medicines Control Council (MCC); Spain, Spanish Agency of Medicines and Medical Devices (AEMPS); Switzerland, Swissmedic; United Kingdom, Medicines and Healthcare Products Regulatory Agency (MHRA).
b Update: date mentioned in the document.
Emergency use authorization (EUA) by the US Food and Drug Administration (FDA) allows the use of unapproved medical products or unapproved use of approved medical products. Currently, PPE items, in vitro diagnostic tests, and ventilators are included in the FDA EUA to tackle the COVID-19 pandemic. However, the FDA still does not allow sharing or reusing N95 respirators. 8 Considering the COVID-19 pandemic specifically, the Centers for Disease Control and Prevention (CDC) published guidance regarding extended use and limited reuse of N95 respirators. Possible methods for decontamination cited as the most promising by the CDC were vaporous hydrogen peroxide, ultraviolet germicidal irradiation, and moist heat. 9 In Brazil, the National Health Surveillance Agency (ANVISA) allowed the hospital infection control commissions (CCIHs) at each health service to create protocols for reuse by the same professional: use, withdrawal, packaging, assessment of integrity, time of use, and criteria for disposal. 10
The impact of the COVID-19 pandemic in each country or region might be influenced by the number of cases, the proportion of patients needing hospitalization, and the infrastructure of healthcare systems. Health authorities should consider global PPE shortages and should define feasible recommendations for extended use or reuse or decontamination of N95 respirators. Regulatory agencies of few countries empowered health services managers to implement strategies for decontamination and/or reuse procedures. The Ministry of Labor and Social Affairs of Germany described the recommended decontamination method for N95 respirators in detail (ie, dry heat at 65–70°C in a drying cabinet for 30 minutes). On the other hand, up to 60% of the screened countries did not report any recommendations for extended use or reuse or decontamination of N95 respirators. In summary, we have provided some evidence that regulatory authorities are trending toward relaxing regulations during the PPE shortage. The extended use and reuse of N95 respirators have become the last resort because it is crucial to maintain HCW protection during the COVID-19 pandemic.
Acknowledgments
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ice.2020.173




