Clostridium difficile produces endospores, which are responsible for the transmission of the organism between patients, sometimes causing a potentially life-threatening C. difficile infection (CDI) or asymptomatic carriage with some spore shedding.Reference Curry, Muto and Schlackman 1 , Reference Toshniwal, Silva, Fekety and Kim 2 Evidence from genetic relatedness of CDI strains suggests that unknown sources of nonhypervirulent C. difficile spores persist, causing up to 82% of CDIs in vulnerable patients.Reference Didelot, Eyre and Cule 3 Mitchell and GardnerReference Mitchell and Gardner 4 reviewed global CDI mortality, including studies from 2005 to 2011, and estimated a 5.7%–6.9% CDI-attributable mortality rate. In North America, CDI-attributable mortality ranges from 5.7% to 16.7%, varying with endemic and epidemic periods.Reference Kwon, Olsen and Dubberke 5 In 2015 and 2016, there were 14,192 and 14,139 cases of CDI in the UK, respectively. 6 Contaminated linen as a potential source of CDI is understudied. The current UK healthcare laundry policy is the Health Technical Memorandum (HTM) 01-04 Decontamination of Linen for Health and Social Care (2016). 7 In brief, all linen classified as ‘infected’ must be put in water-soluble bags (alginate bags) and then into nonpermeable bags. The linen must then be processed with a thermal disinfection cycle at either 65°C for ≥10 minutes or at 71°C for ≥3 minutes. Evidence of survival and cross contamination of C. difficile spores in simulations and related studies also suggest that these industrial wash parameters may be inadequate.Reference Hellickson and Owens 8 , Reference Mackay, Whitehead and Purdue 9 Failed decontamination of laundry could contribute to surface C. difficile contamination within hospitals, and spread is likely exacerbated through the rented-linen business model in the United Kingdom, where regional commercial laundry facilities distribute linen to other hospitals or care facilities within the region. The potential contribution of textiles as an environmental factor to the complex transmission route of C. difficile may be of particular importance because 27% of new residents become asymptomatic carriers of C. difficile within the first 6 weeks of admittance to a care facility.Reference Ponnada, Guerrero and Jury 10 The aim of the present investigation was to assess the survival of C. difficile spores through a washer extractor cycle, incorporating industrial laundry parameters, to determine whether linen could be a potential source of sporadic outbreaks of CDI.
Methods
Strains and growth conditions
Type strain Clostridium difficile NCTC 11209 was obtained from the National Collection of Type Cultures. The clinical strain ribotype 001/072 was isolated during the investigation. Cooked meat broth (Fluka, Sigma-Aldrich, St Louis, MO) was used to produce spore suspensions, and supplemented brain heart infusion (BHI) agar (Oxoid, Ontario, Canada) was used to germinate and quantify viable spores (BHISs). For growth of vegetative cells, the BHI agar was supplemented with 0.1% L-cysteine (Sigma) and 5% horse blood (TCS Biosciences, Buckingham, UK). For spore germination, 0.1% taurocholic acid sodium salt hydrate (Sigma) was added to the growth agar (BHIS/T). Anaerobic culturing conditions were used.
Spore production
A single colony of C. difficile was inoculated into each of 20 aliquots (10 mL) of pre-reduced cooked meat broth, then incubated for 10 days at 37°C. After the incubation, cultures were combined and centrifuged at 3,300×g for 20 minutes. The spore pellet was resuspended in 5 mL 95% ethanol for 20 minutes to inactivate any vegetative cells. The suspension was then centrifuged and washed in maximum recovery diluent (MRD) 3 times. The final pellet was resuspended in MRD and stored at 4°C until use. Spores were enumerated by spread plating onto BHIS and incubated anaerobically at 37°C for 48 hours.
Soiling effect on C. difficile spore recovery from NHS (100% cotton) sheet swatches
Bovine serum albumin (BSA) was used to simulate soiling in ‘clean’ (0.3g/L) and ‘dirty’ (3g/L) conditions according to BS EN 13704.Reference Orr, Holliday, Jones, Robson and Perry 13 Sterile NHS (100% cotton) sheet swatches (25 cm2) were each inoculated with a 0.1-mL aliquot of 6 log10 colony-forming units per milliliter (cfu/mL) spore-test suspension, with a final concentration of either 30 g/L BSA or 3 g/L BSA, and air dried for 18 hours. The swatches were transferred to either a stomacher bag or to a 50-mL Falcon tube containing 10 mL MRD, then were stomached in a paddle blender (LM40, Seward, UK) on high for 1 minute or were vortexed (ThermoFisher Scientific, Loughborough, UK) on high at 40 Hz for 5 bursts of 5 seconds. Then, 0.1 mL of the supernatant was plated onto BHIS/T agar. All agar plates were incubated anaerobically at 37°C for 48 hours.
Simulated industrial laundering of C. difficile spores on 100% cotton sheets
Sterile swatches (25 cm2) were each inoculated with 0.1 mL C. difficile NCTC 11209 spore suspension containing 8 log10 cfu/mL spores. The swatches were air dried overnight for 18 hours. Before washing, the swatches were attached by a sterile safety pin to a single NHS (100% cotton) sheet and placed in a washer extractor (Schulthess 6166, Wolfhausen, Switzerland). Each load contained 4 inoculated swatches and 4 sterile swatches. The full load (6.5 kg) included 10 additional sterile NHS (100% cotton) sheets. The temperature in the drum was verified every 5 seconds by a data logger (Measurement Systems, Newbury, UK). The industrial detergent system (Spectrum EU, Washing Systems International, Cheshire, UK) is outlined in Table 1. A control wash was also conducted without the detergent, and the investigation was repeated with the clinical strain ribotype 001/072.
Table 1 Simulated Cycle Parameters Programmed by the Detergent Supplier According to Industry Standards
a Peracetic acid: acetic acid and hydrogen peroxide.
After the wash cycle, each swatch was vortexed in 30 mL MRD, 5 times for 5 seconds, then left in the MRD for 5 minutes. The enumeration of surviving spores was conducted by vacuum filtering (black 0.45 µm Whatman filter, GE Healthcare Life Sciences, Marlborough, MA). For detergent cycles, the entire 30 mL suspension was filtered, and for control cycles, duplicate 0.1 mL samples were filtered, both followed by duplicate 0.1 mL samples from a 1 log10 serial dilution. Method validations showed that filtration was successful at neutralizing the detergent (data not shown). The filter membranes were transferred to pre-reduced BHIS agar plates and incubated anaerobically at 37°C for 48 hours.
Scanning electron microscopy (SEM) of spores on cotton after laundering
Cotton swatches were fixed and prepared for viewing by SEM using 2% glutaraldehyde (G7526, Sigma) in phosphate buffer. Individual swatches were mounted on 2.5-cm aluminum stubs and sputter coated with gold (S150B sputter coater, Edwards, Burgess Hill, UK). The stubs were viewed using a SEM (Evo HD 15, Carl Zeiss, Oberkochen, Germany) under high vacuum with a beam accelerating voltage of 5–7 kV for magnifications between 2,500 and 50,000×.
Ethical approval
Ethical approval for the study was obtained from (1) De Montfort University Health and Life Sciences’ Research Ethics Committee (reference: 714) and (2) ‘Nottingham 2’ NHS Research Ethics Committee (reference: 11/EM/0002). Local research and development permission was obtained from the trust responsible for the NHS hospital research site (reference: UHL10003). The participating hospital allowed access to a C. difficile isolation ward.
Media
Braziers CCEY selective agar (Lab160, LabM, Heywood, UK) was used to ensure that only C. difficile spores were isolated from the samples. The agar contained the selective antibiotic cycloserine and cefotoxin supplement (X093, LabM) and egg yolk emulsion (X073, LabM).
Storage and collection of the naturally contaminated sheets
To ensure a realistic quantification of C. difficile spore burden before washing, storage of sheets after use in the ward was the same as for standard infected linen. A set of experimental sheets were delivered weekly to the ward. The sheets were used on CDI patient beds and changed daily or when soiling had occurred. After use, the sheets were placed in alginate bags and sealed. The alginate bags were put into standard red ‘infected-linen’–labelled plastic, nonpermeable bags and stored in the ward’s used linen room. The bags were collected every 24 hours, in accordance with standard practice at the site, were transferred to an external waste compound overnight, and were collected the following morning for sampling.
Sampling
Soiled sheets were numbered, and regions soiled with fecal matter were identified. From these, three 25 cm2 swatches were removed leaving adjacent 25 cm2 soiled regions for sampling after washing. The sheet was placed back into the alginate bag, resealed with the tie, and put into the red ‘infected linen’ bags. The bags were transported to the laundry the same day.
Individual sample swatches were placed in 50-mL Falcon tubes with 30 mL of MRD; viable spores were recovered using the vortexing method (5 seconds 5 times on high speed). Swatches were removed, and suspensions were heat shocked in a water bath at 80°C for 10 minutes. Suspensions were then vacuum filtered. Agar plates were incubated anaerobically at 37°C for 48 hours.
The sampled sheets were then transported to the laundering facilities immediately after sampling and washed in a washer extractor (30 kg commercial washer extractor) cycle meeting the minimum requirements of HTM 01-04 7 and were handled according to BS EN 14065:2002. 12 Post-wash samples were processed with the same method used for pre-wash samples.
Industrial laundering
At the collaborating NHS-approved commercial healthcare laundry, the bags were transferred to the ‘dirty’ side of the facility, and the unopened alginate bags were loaded into a washer extractor for a wash cycle at 75°C for ≥3 minutes with 8 minutes mixing time using the same industrial detergent system used in the simulated washes. The sheets were then transported to the ironer bed, where they were pressed and dried at 175°C with 4 bars of pressure for 3 seconds (calendaring).
Identifying clinical strains
All presumptive C. difficile positive plates were confirmed by the gold-standard latex agglutination and long-wave ultraviolet fluorescence test. Ribotyping was then performed by polymerase chain reaction (PCR) with capillary gel electrophoresis (CE-ribotyping), at a Public Health England (PHE) laboratory (Newcastle, UK).
Statistical analysis
All statistical analyses were performed with SPSS version 22 software (IBM, Armonk, NY). The significance value for all tests was set at P≤.05. Depending on normality of the distribution of the data, either a 1-way analysis of variance (ANOVA) or independent t test was conducted. For nonparametric data, a Mann-Whitney U test or a Kruskal-Wallis test was performed. Each investigation was repeated in triplicate on 2 separate occasions (n=6) unless otherwise stated.
Results
Significantly more spores were recovered from cotton swatches by the vortexing method than by the stomaching method, at both light and heavy levels of soiling (P≤.05) (Fig. 1). For the vortexing method, 4.48 and 4.41 log10 cfu/25 cm2 spores were recovered from heavily and lightly soiled swatches, respectively (original inoculum, 5 log10 cfu/25 cm2).
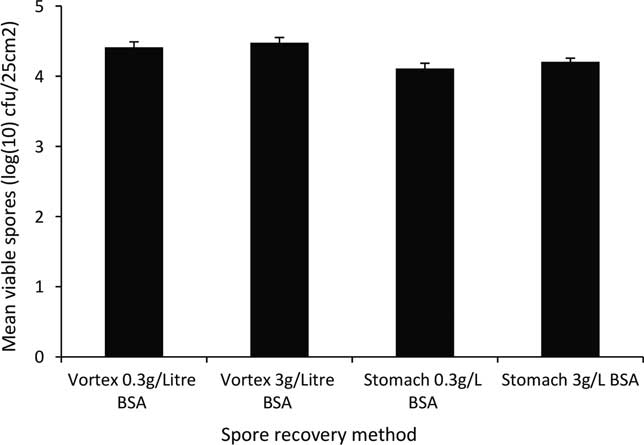
Fig. 1 Comparison of methods for C. difficile spores recovered from NHS (100% cotton) sheet swatches with BSA soiling at low (0.3 g/L) and high (3 g/L) (mean ± SE, n=6).
In the simulated laundry control cycle (without detergent), significantly fewer spores were recovered, compared to the original inoculum (7 log10 cfu/25 cm2), for both C. difficile NCTC 11209 (4.95 log10 cfu/25 cm2; P≤.05) and ribotype 001/072 (5.27 log10 cfu/25 cm2; P≤.05) (Fig. 2). In addition, the numbers of recovered spores after this laundry control cycle were not significantly (P > .05) different between the 2 strains. Without detergent, the effects of temperature and agitation alone did not reduce the number of spores by >2 log10 cfu/25 cm2, leaving the swatches heavily contaminated with 4.95 log10 cfu/25 cm2 C. difficile spores (Fig. 2).
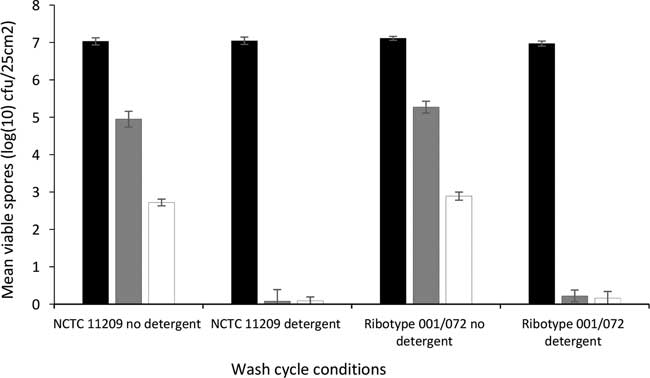
Fig. 2
In vitro assessment of the recovered C. difficile spores after being processed in a washer extractor: the original inoculum (log10 cfu/ml) (![]() ), per inoculated swatch (
), per inoculated swatch (![]() ) and per previously sterile swatch (
) and per previously sterile swatch (![]() ). Strain types NCTC 11209 and ribotype 001/072 (mean ± SE, n=4).
). Strain types NCTC 11209 and ribotype 001/072 (mean ± SE, n=4).
Regarding the level of cross contamination during the control cycle, similar numbers of spores were recovered from previously sterile swatches for both NCTC 11209 and ribotype 001/072 (2.72 vs 2.89 log10 cfu/25 cm2). In wash cycles that included detergent, recovery of spores for both strains was significantly (P≤.05) reduced (to 0–4 cfu/25 cm2 for NCTC 11209 and 0–9 cfu/25 cm2 for ribotype 001/072), with cross contamination to previously sterile swatches ranging from 0 to 8 cfu/25 cm2 and from 0 to 14 cfu/25 cm2 (Fig. 2).
The presence of C. difficile spores on cotton swatches after laundering was confirmed by SEM (Fig. 3). The SEM images show clumps of C. difficile spores, potentially within the soiling with which they were inoculated (Fig. 3d). Possible spore lysis was also evident (Fig. 3c), possibly through detergent or thermal disinfection or a combination of both.
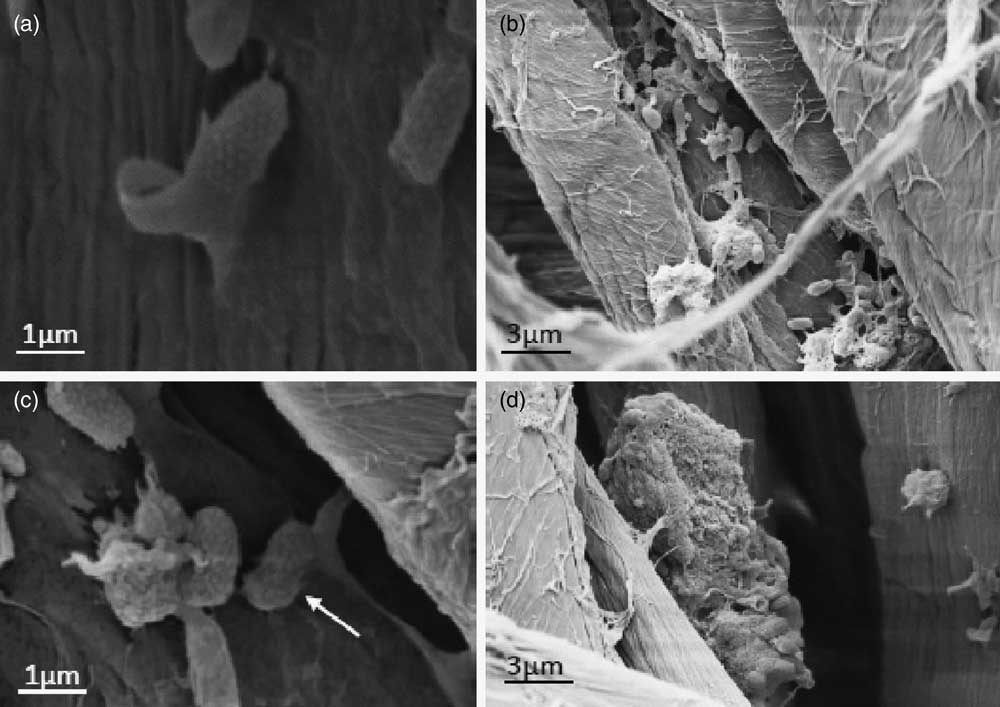
Fig. 3 Scanning electron microscopy (SEM) images of C. difficile spores on a NHS (100% cotton) sheets: swatch inoculated with 0.1 mL 8 log10 cfu/mL test suspensions containing 3 g/L BSA. The swatch air dried for 24 hours and was then washed in a simulated healthcare wash at 71°C with industrial detergent (held at 71°C for 5 minutes). (A) spore, (B) many spores left on the swatch after washing, (C) further magnification area in (B), and (D) large clump of spores (soiling or coaggregation).
Swatches removed from the naturally contaminated sheets had an average spore load of 51 cfu/25 cm2 (1.7 log10 cfu/25 cm2), with a range of 2–158 cfu/25 cm2 (Table 2). The post-wash swatches (washed at ≥71°C for 3 minutes plus 8 minutes mixing, dried, and finished) still had an average spore load of 33 cfu/25 cm2 (1.25 log10 cfu/25 cm2). The post-wash average spore load was calculated from a combined 90-mL sample for each sheet: >100 cfu/75 cm2. Thus, the post-wash reduction was 18 cfu/25 cm2 (or 0.45 log10 cfu/25 cm2), only a 40% reduction in spore load after washing. Subsequent ribotyping of the isolates recovered before and after washing showed that they were indistinguishable and had only a single minor difference from ribotype 001/072 (PHE, Newcastle). This finding suggests that the spores recovered after washing were present before washing and were not a result of contamination during the wash cycle.
Table 2 C. difficile Spores Recovered From Swatches (25cm2) of Naturally Contaminated (100% cotton) Sheets, Before and After Washing to Meet NHS Healthcare Policy Minimum Standards HTM 01-04 at Industrial Launderers (n=3)
Note. cfu, colony-forming units.
aThe cfu per 75 cm2 wasrecorded at maximum count for each sheet (≥100) where the three 30-mL recovered suspensions per sheet were filtered together.
Discussion
The aim of comparing recovery methods of C. difficile spores in the presence of soiling was to ascertain an efficient method of recovering spores in heavily soiled conditions often found on bed sheets of CDI patients. Because the vortexing method recovered significantly more spores than the stomaching method, this method was subsequently used in the laundering investigations. Several agitation methods were previously tested (data not shown) and were not as effective as vortexing. The vortexing method has also been used in other studies to assess the efficacy of the minimum laundry conditions required by HTM 01-04.Reference Orr, Holliday, Jones, Robson and Perry 13 – Reference Fijan and Å ostar Turk 15 Notably, the current healthcare laundry policy, HTM 01-04, 7 suggests the use of ‘agitation’ to recover B. cereus spores for annual seasonal microbiological assessments. Stomaching for 1 minute was recommended by the laboratory responsible for microbiology at the commercial laundry in this study (personal communication, 2011). Therefore, the reported proportions of viable spores (B. cereus or C. difficile) recovered are dependent upon the type and duration of agitation method chosen by the testing laboratory. The use of varying recovery methods for spores from textiles between organizations is concerning because spore recovery can vary significantly depending on the spore recovery method.
The test wash cycles used in this investigation all reached 75°C and were held at ≥71°C for >3 minutes (+8 minutes mixing time), as required by thermal disinfection conditions of the policy HTM 01-04. For both test strains, the use of detergent was an important factor in significantly reducing the numbers of C. difficile spores (Fig. 2). We observed a >6 log10 reduction in the number of viable spores recovered from swatches after washing using the industrial detergent system in the simulated HTM 01-04–compliant healthcare cycle. The >6 log10 reduction still applied after considering that the spore recovery method only recovered an average of 31% of the viable spores remaining on the swatch. In the control cycle without the industrial detergent system, thermal disinfection and agitation were found to be inadequate to affect a >5 log10 reduction in C. difficile spores.
Cross contamination occurred in both the control and detergent washes, where spores removed from the inoculated swatches were transferred to other material present in the drum (Fig. 2). Cross contamination was significantly higher when the detergent system was not included in the cycle.
Chemo-thermal disinfection proved to be significantly better at decontaminating the swatches than thermal disinfection alone, but even in an optimized wash, 0.1–1 log10 cfu/25 cm2 remained. This quantity would fail the microbiological validation requirement of <100 cfu per test swatch with no pathogenic bacteria present. The SEM images in this study (Fig. 3) confirmed the presence of C. difficile spores on swatches after a 71°C wash with detergent.
The healthcare wash-cycle simulations provide quantification and further insight to the understanding of whether C. difficile spores survive the thermal and chemo-thermal conditions that can be applied by laundries. These findings verify the research by Hellickson and Owens,Reference Hellickson and Owens 8 who demonstrated the unquantified presence of C. difficile spores on inoculated and previously sterile swatches washed in a simulated healthcare wash cycle. The present study goes further in establishing that in the simulation conditions described, the use of detergent significantly reduces the number of viable spores recovered by 6–7 log10 on inoculated swatches and reduces cross-contamination by >2.5 log10 on previously sterile swatches. The 0.1–1 log10 cfu/25 cm2 that may remain on swatches after a simulated healthcare wash cycle was a conservative estimate due to the inability to recover 100% of viable spores present with the vortexing method used (Fig. 1).
More recently, Mackay et alReference Mackay, Whitehead and Purdue 9 compared washing ambulance uniform swatches artificially contaminated with C. difficile spores at 30°C and 60°C in a Miele PW6055 (commercial) machine (Miele, Gütersloh, Germany) with Cleanline biological washing powder (Bunzl Cleaning and Hygiene Supplies, Berkshire, UK). Viable C. difficile spores were recovered from all swatches washed at 30°C and 60°C, with a range of 1.6–6.73 log10 cfu C. difficile spores remaining per swatch.
This study provides the first estimate of the level of C. difficile spore contamination on a naturally contaminated sheet, which was surprisingly low considering the published estimate of spore shedding in CDI patients: 5–7 log10 cfu per gram of feces.Reference Riggs, Sethi, Zabarsky, Eckstein, RLP and Donskey 16 The level of C. difficile spores present on the sheets before washing (51 cfu/25 cm2) was comparable to that found after washing (33 cfu/25 cm2).
During the simulation, the detergent system significantly reduced spore contamination (Fig. 2). However, when processed at the commercial healthcare laundry, industrial detergent combined with disinfection temperatures was unable to affect a significant reduction in spores. This finding was particularly surprising because the sheets were exposed to additional repeated high-temperature cycles, through drying and calendaring, beyond what was possible in the simulations.Reference Rodriguez-Palacios and LeJeune 17 , Reference Wilson, Loveday, Hoffman and Pratt 18
The low levels of C. difficile spores surviving on laundered bed sheets may pose a transmission risk via hands touching the linen. Rusin et alReference Rusin, Maxwell and Gerba 19 reported that Serratia rubidea and Micrococcus luteus, transferred from 100% cotton swatches to hands from an initial inoculum of 9.7 log10 cfu were 4.40 and 6.17 log10 cfu, respectively. However, these researchers noted that the hand transfer efficiency was much higher from hard surfaces than from porous surfaces such as textiles.
In conclusion, in this investigation, we quantified C. difficile spores on naturally contaminated bed sheets before and after they were washed in a washer extractor on a commercial laundry site. The thermal disinfection conditions, described in HTM 01-04, were inadequate to fully decontaminate linen that had been naturally contaminated with C. difficile spores. The detergent and additives had the greatest effect in reducing spore burden, whether by removal or in combination with the thermal disinfection. The surviving spores may contribute to environmental contamination when the sheets are used for bed making in the healthcare environment. Processing infected linen in commercial washer extractor cycles could disseminate low levels of C. difficile spores and may be contributing to sporadic outbreaks of CDI.
Acknowledgments
The authors thank the Textile Services Association for the loaned equipment, detergent supplies, and industry-specific advice. We thank PHE Newcastle for ribotyping of isolated C. difficile and the commercial laundry and hospital that provided access to their facilities.
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.







