Introduction
HIV/AIDS remains a major public health threat despite the significant decline in AIDS-related deaths worldwide (Frank et al., Reference Frank, Carter, Jahagirdar, Biehl, Douwes-Schultz, Larson and Abu-Raddad2019). As of 2019, there were an estimated 38.0 million people worldwide living with HIV/AIDS, with the highest percentage in sub-Saharan Africa (SSA) (World Health Organization [WHO], 2020). Approximately 1.7 million new HIV infections and 690,000 AIDS-related deaths occurred in 2019 (WHO, 2020). A recent report on the impact of the COVID-19 pandemic on antiretroviral therapy (ART) suggests a possible disruption in HIV/AIDS management, which is expected to increase AIDS-related deaths in the next year, mostly in SSA. This has resulted in the need to scale up HIV/AIDS-related interventions to help curb the pandemic in the face of the COVID-19 threat (Jewell et al., Reference Jewell, Mudimu, Stover, Ten Brink, Phillips, Smith and Bansi-Matharu2020; WHO, 2020).
Globally, several interventions or programmes are being implemented to end the HIV/AIDS pandemic (Fauci & Lane, Reference Fauci and Lane2020). In 2016, for instance, the United Nations Political Declaration on HIV/AIDS set a global target of accelerating the fight against HIV and ending the AIDS pandemic by 2030 (United Nations General Assembly, 2016). Among the targets of the United Nations Program on HIV/AIDS (UNAIDS) is to achieve 95-95-95 by 2030 – that is, to diagnose at least 95% of people living with HIV, of whom at least 95% should be on treatment and out of which at least 95% should have achieved viral suppression by 2030 (Pandey & Galvani, Reference Pandey and Galvani2019). However, a recent report shows that most countries are likely to miss the 2030 global target (Frank et al., Reference Frank, Carter, Jahagirdar, Biehl, Douwes-Schultz, Larson and Abu-Raddad2019), largely due to gaps in HIV testing and treatment initiation (UNAIDS, 2018). Early initiation of treatment significantly decreases viral load and its associated morbidity and mortality (Cohen et al., Reference Cohen, Chen, McCauley, Gamble, Hosseinipour, Kumarasamy and Godbole2011).
HIV counselling and testing is the first and most important step towards prevention and early initiation of treatment (Cohen et al., Reference Cohen, Chen, McCauley, Gamble, Hosseinipour, Kumarasamy and Godbole2011; Sharma et al., Reference Sharma, Ying, Tarr and Barnabas2015). However, it has been reported that about 9.4 million people living with HIV in 2017 did not know their status and a significant proportion of these people live in SSA (UNAIDS, 2018). Despite the significant improvement in voluntary HIV counselling, testing and HIV prevention measures, including the introduction of rapid diagnostic tests and self-tests (WHO, 2020), coverage remains low in most sub-Saharan African countries (Sharma et al., Reference Sharma, Ying, Tarr and Barnabas2015; Harichund et al., Reference Harichund, Moshabela, Kunene and Abdool Karim2019). Apart from discrimination, stigma and non-confidential testing environments (Bwambale et al., Reference Bwambale, Ssali, Byaruhanga, Kalyango and Karamagi2008; Harichund & Moshabela, Reference Harichund and Moshabela2018), lack of comprehensive HIV/AIDS knowledge remains one of the major barriers to uptake of HIV testing in SSA (Aderemi et al., Reference Aderemi, Mac-Seing, Woreta and Mati2014; Harichund & Moshabela, Reference Harichund and Moshabela2018). For example, in a cross-sectional survey to determine HIV testing uptake among youths in SSA, Asaolu et al. (Reference Asaolu, Gunn, Center, Koss, Iwelunmor and Ehiri2016) reported that having comprehensive HIV knowledge is associated with higher odds of being tested. Seidu et al. (Reference Seidu, Ahinkorah, Dadzie, Tetteh, Agbaglo and Okyere2020) also reported that having comprehensive HIV/AIDS knowledge is associated with lower odds of self-reported sexually transmitted infections among sexually active men in SSA.
With the introduction of community and home-based HIV counselling and testing models, the uptake of HIV testing among males in SSA has been boosted (DiCarlo et al., Reference DiCarlo, Mantell, Remien, Zerbe, Morris and Pitt2014; Hensen et al., Reference Hensen, Lewis, Schaap, Tembo, Mutale and Weiss2015). Available evidence suggests that most studies on comprehensive HIV/AIDS knowledge and testing in SSA have focused on women (e.g. Teshome et al., Reference Teshome, Youjie, Habte and Kasm2016; Yaya et al., Reference Yaya, Bishwajit, Danhoundo, Shah and Ekholuenetale2016; Sheikh et al., Reference Sheikh, Uddin and Khan2017; Darteh, Reference Darteh2020), students (e.g. Agha, Reference Agha2012; Asante, Reference Asante2013 Oljira et al., Reference Oljira, Berhane and Worku2013; Kejela et al., Reference Kejela, Oljira, Dessie and Misker2015), youth or adolescents (e.g. Ziraba et al., Reference Ziraba, Madise, Kimani, Oti, Mgomella, Matilu and Ezeh2011; Asaolu et al., Reference Asaolu, Gunn, Center, Koss, Iwelunmor and Ehiri2016; Chikwari et al., Reference Chikwari, Dringus and Ferrand2018) and men who have sex with men (e.g. Sorensen et al., Reference Sorensen, Sansom, Brooks, Marks, Begier and Buchacz2012). Thus, there is a paucity of literature on the association between comprehensive HIV/AIDS knowledge and testing among the general male population in SSA. Therefore, this study focuses generally on the association between comprehensive HIV/AIDS knowledge and HIV testing among men in SSA. Understanding the association between comprehensive HIV/AIDS knowledge and HIV testing is important in identifying targeted areas for HIV/AIDS education and testing strategies that could potentially increase HIV testing uptake among men in SSA and contribute to the realization of the global HIV/AIDS target of 95-95-95 by 2030.
Methods
Theoretical model
The study was guided by the Knowledge, Attitude and Practice (KAP) survey model adapted from Muleme et al. (Reference Muleme, Kankya, Ssempebwa, Mazeri and Muwonge2017). This model states that an individual’s knowledge could be influenced by socio-demographic factors that affect their attitude, which then becomes an incentive or a disincentive to practice (behaviour). The assumption here, based on previous studies (Asaolu et al., Reference Asaolu, Gunn, Center, Koss, Iwelunmor and Ehiri2016; Seidu et al., Reference Seidu, Ahinkorah, Dadzie, Tetteh, Agbaglo and Okyere2020), was that those with comprehensive HIV/AIDS knowledge would be more likely to test for their HIV/AIDs status. Furthermore, it was recognized that comprehensive HIV/AIDS knowledge and testing could be influenced by socio-demographic factors, including age, marital status, employment status, educational level, exposure to newspapers, exposure to radio, exposure to television, wealth index, place of residence, condom use and multiple sexual partners, as reported in the literature (Ziraba et al., Reference Ziraba, Madise, Kimani, Oti, Mgomella, Matilu and Ezeh2011; Agha, Reference Agha2012; Teshome et al., Reference Teshome, Youjie, Habte and Kasm2016; Yaya et al., Reference Yaya, Bishwajit, Danhoundo, Shah and Ekholuenetale2016; Agegnehu et al., Reference Agegnehu, Geremew, Sisay, Muchie, Engida and Gudayu2020; Kefale et al., Reference Kefale, Damtie, Yalew, Adane and Arefaynie2020). Figure 1 shows the theoretical associations between the outcome, independent and control variables employed in the study.

Figure 1. Knowledge, attitude and practice theoretical model; adapted from Muleme et al. (Reference Muleme, Kankya, Ssempebwa, Mazeri and Muwonge2017).
Data source
The study used data from the most recent (2010–2019) Demographic and Health Surveys (DHS) of 29 sub-Saharan African countries – specifically, the men’s recode files. The DHS is a nationally representative survey conducted in over 85 low- and middle-income countries. It focuses on essential markers, including breastfeeding, fertility, family planning, immunization, HIV/AIDS, child health and nutrition (Corsi et al., Reference Corsi, Neuman, Finlay and Subramanian2012). The survey employs a two-stage stratified sampling technique, which makes the data nationally representative. The study by Aliaga and Ruilin (Reference Aliaga and Ruilin2006) provides details of the sampling process. A total of 104,398 men who had complete information on all the variables of interest were included in the current study. The Strengthening the Reporting of Observational Studies in Epidemiology’ (STROBE) statement was consulted during the writing of the manuscript (Von Elm et al., Reference Von Elm, Altman, Egger, Pocock, Gøtzsche, Vandenbroucke and Initiative2014). The dataset is freely available for download at: https://dhsprogram.com/data/available-datasets.cfm.
Definition of variables
Outcome variable
The outcome variable was HIV testing, which was derived from the question ‘Have you ever tested for HIV?’ Responses were ‘Yes’ and ‘No’, coded as ‘No’=0 and ‘Yes’=1.
Explanatory variable
Comprehensive HIV/AIDS knowledge was used as the main explanatory variable. This was defined as knowing that consistent use of condoms during sexual intercourse, and having just one uninfected faithful partner, can reduce the chance of getting an HIV infection; knowing that a healthy-looking person can have the AIDS virus; and rejecting the two most common local misconceptions about AIDS transmission or prevention (i.e. via mosquito bites or witchcraft/supernatural means). Comprehensive HIV knowledge was dichotomously coded ‘Yes’ = 1 and ‘No’ = 0. An index was created based on the correct answers to the preceding questions (Darteh, Reference Darteh2020; Frimpong et al., Reference Frimpong, Budu, Adu, Mohammed, Tetteh, Seidu and Ahinkorah2021).
Control variables
Eleven control variables were considered in the study, broadly grouped into individual level and contextual level variables. The individual level variables included age, employment status, marital status, educational level, exposure to newspapers, exposure to radio, exposure to television, condom use and number of sexual partners. The contextual level factors included wealth quintile and type of place of residence. These variables were not determined a priori; instead, they were based on parsimony, theoretical relevance and practical significance with HIV testing (Yaya et al., Reference Yaya, Bishwajit, Danhoundo, Shah and Ekholuenetale2016; Agegnehu et al., Reference Agegnehu, Geremew, Sisay, Muchie, Engida and Gudayu2020; Kefale et al., Reference Kefale, Damtie, Yalew, Adane and Arefaynie2020).
Statistical analyses
The data were analysed with Stata version 14.0. The analysis was done in three steps. The first step was the graphical computation of the prevalence of HIV testing and comprehensive HIV/AIDS knowledge among men in SSA. The second step was a bivariate analysis, which calculated the proportions of HIV testing across the explanatory and control variables with their significance levels (Table 1). To check for a high correlation among the explanatory and control variables, a test for multicollinearity was carried out using the variance inflation factor (VIF) and the results showed no evidence of high collinearity (Mean VIF=1.41, Maximum VIF=1.69, and Minimum VIF=1.06).
Table 1. Description of study sample

All the variables that showed statistical significance from the Table 1 were moved to a multilevel logistic regression analysis. Five models were used to present the results (Model 0, Model I, Model II, Model III, Model IV). Model 0 was the empty model that had no explanatory or control variables. Model I had only the key explanatory variable. Model II had the individual-level control variables. Model III had the contextual-level control variables. Model IV had the explanatory variable and all the control variables. However, the results for Models 0, I and IV are presented. The multilevel logistic regression analysis comprised fixed effects and random effects (Austin & Merlo, Reference Austin and Merlo2017). The results of the fixed effects of the models were presented as Adjusted Odds Ratios (AORs) while the random effects were assessed with intra-cluster correlation (ICC) (Merlo et al., Reference Merlo, Wagner, Ghith and Leckie2016). Model comparison was done using the log-likelihood ratio (LLR) and Akaike’s Information Criterion (AIC) test. The highest log-likelihood and the lowest AIC were used to determine the best-fit model (see Table 2). All frequency distributions were weighted (v005/1000000) while the survey command svy in Stata was used to adjust for the complex sampling structure of the data in the regression analyses.
Table 2. HIV testing by explanatory variables (N=104,398 weighted)

Results
Figure 2 presents the prevalence of HIV testing among men in the 29 sub-Saharan African countries. On the average, the prevalence of HIV testing was 53.5% in SSA. Rwanda and Niger recorded the highest (93.6%) and lowest prevalences (9.8%) respectively. The prevalence of comprehensive HIV/AIDS knowledge among men in the 29 countries was 50.8%, with the highest in Rwanda (76.4%) and the lowest in Benin (31.1%) (Figure 3).
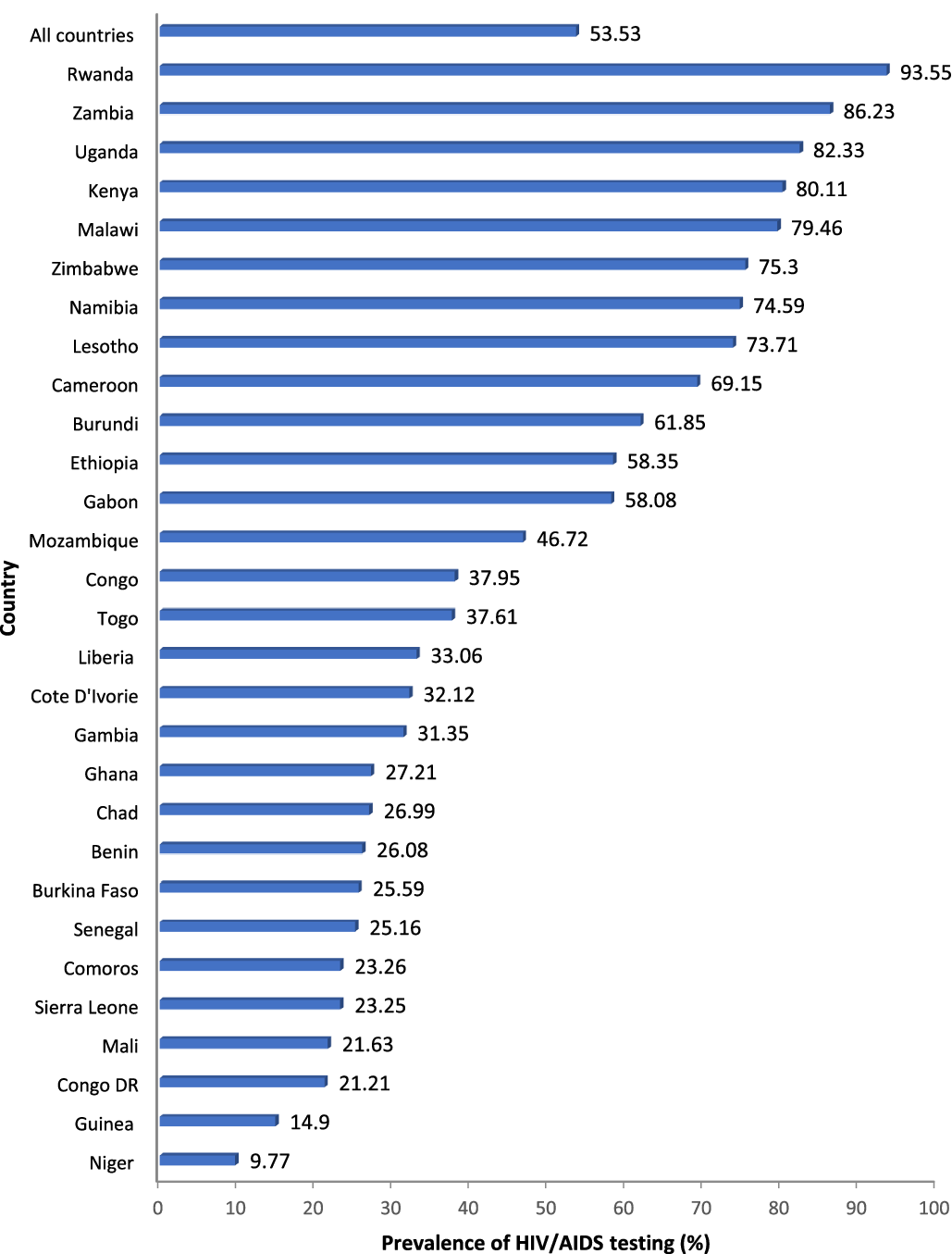
Figure 2. Prevalences of HIV testing among men in 29 countries in sub-Saharan Africa.

Figure 3. Prevalences of comprehensive knowledge of HIV/AIDS among men in 29 countries in sub-Saharan Africa.
Table 2 presents the prevalences of HIV testing by the explanatory and control variables. The majority (62.5%) of men who had comprehensive knowledge of HIV/AIDS presented themselves for testing compared with only 44.3% of men who had no comprehensive HIV/AIDS knowledge. HIV testing was highest among men in the age group 30–34 (59.4%), those who were not working (54.3%) and who were cohabiting (55.6%). Men with secondary education (61.3%), the richest (65.6%), those residing in urban areas (59.7%), those exposed to newspapers almost every day (82.3%), those exposed to radio almost every day (81.4%), and those exposed to television almost every day (72.6%) had the highest proportions of HIV testing. Men who used condoms and those who had multiple sexual partners had slightly higher proportions testing for HIV (60.9% and 60.8% respectively).
Multilevel logistic regression results on determinants of HIV testing among men in sub-Saharan Africa
Fixed effects results
Table 3 presents the multilevel logistic regression results on the determinants of HIV testing among men in SSA. Men who had no comprehensive HIV/AIDS knowledge were less likely to test for HIV compared with their counterparts who had comprehensive HIV/AIDS knowledge (AOR=0.59, CI: 0.57–0.60) With the covariates, age, employment status, marital status, educational level, wealth index, exposure to newspapers, exposure to radio, exposure to television, condom use, having multiple sexual partners, and place of residence were associated with HIV testing (Model IV).
Table 3. Multilevel logistic regression results on the determinants of HIV testing among men in sub-Saharan Africa

*p<0.05; **p<0.01; ***p<0.001.
Ref.=Reference category; PSU: Primary Sampling Unit; ICC=Intra-Class Correlation; AIC=Akaike’s Information Criterion.
Model 0=empty model with no explanatory variables; Model I=model with only the key explanatory variable; Model IV=model with the key explanatory variable and the control variables.
Random effects results
The random effects results indicated a substantial variation in HIV testing among men in SSA across the PSUs without the explanatory and control variables, as shown in Model 0 (σ 2=0.35; 95% CI=0.30–0.41). The ICC value showed that about 10% (ICC=0.09) of the total variance was attributable to the clustering at the contextual level. The variations changed with the inclusion of key explanatory, individual and community level variables, and all explanatory variables. The AIC values showed variations in model fitness from one model to another. However, the final model, which had all the explanatory variables, was considered the best-fit model since it had the lowest AIC (Table 3).
Discussion
This study investigated the association between comprehensive HIV and AIDS knowledge and HIV testing among men in 29 sub-Saharan African countries using DHS data. The prevalences of comprehensive HIV/AIDS knowledge and HIV testing among men in SSA were found to be 50.3% and 53.5%, respectively, which are lower than the UNAIDS target of 95% by 2030 (United Nations General Assembly, 2016). The study also found that comprehensive HIV/AIDS knowledge, age, employment status, marital status, educational level, wealth index, exposure to newspapers, exposure to radio, exposure to television, condom use, having multiple sexual partners and place of residence were associated with HIV testing.
The finding that Rwanda, Uganda, Kenya, and Malawi recording the highest prevalences of HIV testing among men in SSA, and Niger, Guinea, Congo DR, and Mali recorded the lowest prevalences, is consistent with the findings of a previous cross-sectional study in SSA (Staveteig et al., Reference Staveteig, Wang, Head, Bradley and Nybro2013). The disparities in prevalence of HIV testing among countries in SSA could be the result of disparities in programmes adopted by each country to deal with HIV/AIDS. Rwanda for example, implemented an extensive HIV/AIDS comprehensive education programme in 1986 using the radio and public health educators (Allen et al., Reference Allen, Lindan, Serufilira, Van de Perre, Rundle and Nsengumuremyi1991), and launched the ‘treat all programme’ in the early 2000s, later restructured (in 2016) by the Rwandan Ministry of Health to make testing cheap and more easily accessible and put all those who tested positive on treatment immediately. These, coupled with previous successes that have seen over 99% of health facilities in Rwanda providing HIV testing services, have all contributed to the higher comprehensive HIV/AIDS Knowledge and HIV testing prevalence in Rwanda than in other countries, such as Congo DR; this is reported to be challenged with lack of HIV testing services and inadequate testing centres, which could be a plausible explanation for its low HIV testing (Carlos et al., Reference Carlos, Martínez-González, Burgueño, López-Del Burgo, Ruíz-Canela and Ndarabu2015; Nsanzimana et al., Reference Nsanzimana, Prabhu, McDermott, Karita, Forrest and Drobac2015; UNAIDS, 2017).
In general, the reason for the increase in HIV testing among men in SSA from 22.8% reported by Staveteig et al. (Reference Staveteig, Wang, Head, Bradley and Nybro2013) to 53.5% reported in the present study could be the general scaling up and implementation of the UNAIDS 90:90:90 programme in SSA, which sought to achieve by 2020 (90% of people living with HIV/AIDS knowing their status, 90% of people who know their status having access to antiretroviral therapy and at least 90% of people on treatment having a suppressed viral load) (Piot et al., Reference Piot, Abdool Karim, Hecht, Legido-Quigley, Buse and Stover2015; Maheu-Giroux et al., Reference Maheu-Giroux, Marsh, Doyle, Godin, Lanièce Delaunay and Johnson2019). Notwithstanding this, there is the need for SSA countries to further develop pragmatic health strategies (such as self-testing and mobile or workplace testing) and comprehensive education on the need to test for HIV/AIDS as this will help attain the United Nations goal of achieving 95-95-95 by the year 2030.
The literature suggests that comprehensive knowledge of HIV/AIDS leads to positive behavioural attitudes, which in turn lead to a reduced risk of infection (Seidu et al., Reference Seidu, Ahinkorah, Dadzie, Tetteh, Agbaglo and Okyere2020). It is, therefore, not surprising to find that men who had no comprehensive HIV/AIDS knowledge also had lower odds of testing for HIV compared with their counterparts who had comprehensive knowledge, and this supports the findings of a previous study among youths in SSA by Asaolu et al. (Reference Asaolu, Gunn, Center, Koss, Iwelunmor and Ehiri2016).
Corroborating the findings of previous studies (Staveteig et al., Reference Staveteig, Wang, Head, Bradley and Nybro2013; Asaolu et al., Reference Asaolu, Gunn, Center, Koss, Iwelunmor and Ehiri2016), this study found that men aged 15–19 years had lower odds of testing for HIV compared with those aged 25–29 years. A plausible reason for this could be that younger males are mostly dependent on their parents and may lack the decision-making power and the financial capability to go for HIV testing. Also, their unwillingness to go for testing may be as a result of fear, anxiety or stigma (Asante, Reference Asante2013). Programmes to scale up HIV testing should therefore consider conducting periodic and mandatory HIV testing for younger men in educational settings.
This study found that those who were working had lower odds of testing for HIV, unlike the study by Kefale et al. (Reference Kefale, Damtie, Yalew, Adane and Arefaynie2020). A plausible reason for this finding could be that workers may have difficulty absenting themselves from work and find the time to spend at health centres or hospitals to test for HIV. Policymakers therefore need to intensify the provision of rapid diagnostic tests, self-test gadgets and mobile health vans to bring HIV testing to the doorstep of men, especially the working population in the sub-Saharan African region.
In support of findings of previous studies (Ziraba et al., Reference Ziraba, Madise, Kimani, Oti, Mgomella, Matilu and Ezeh2011; Agha, Reference Agha2012), this study found that those who were not married had the lowest odds of testing for HIV. The common practice of premarital HIV testing in many sub-Saharan African countries could be the plausible reason behind this finding. Previous studies have highlighted how HIV testing is often made mandatory for people preparing to marry in some SSA countries, including Nigeria, Ethiopia, and Cameroon so most married men have already tested for HIV (Arulogun & Adefioye, Reference Arulogun and Adefioye2010; Akoku et al., Reference Akoku, Tihnje, Tarh, Tarkang and Mbu2018; Ahmed & Seid, Reference Ahmed and Seid2020).
Findings from previous studies (Teshome et al., Reference Teshome, Youjie, Habte and Kasm2016; Yaya et al., Reference Yaya, Bishwajit, Danhoundo, Shah and Ekholuenetale2016; Sheikh et al., Reference Sheikh, Uddin and Khan2017; Agegnehu et al., Reference Agegnehu, Geremew, Sisay, Muchie, Engida and Gudayu2020) support the present finding that those with no education had the lowest odds of testing for HIV. A plausible reason for this is that people who are educated may have greater access to information on HIV testing, as well as how and where to get tested, than those who have no formal education (Agegnehu et al., Reference Agegnehu, Geremew, Sisay, Muchie, Engida and Gudayu2020; Kefale et al., Reference Kefale, Damtie, Yalew, Adane and Arefaynie2020). Another likely explanation is that individuals who have no education may lack the ability to understand the need to test for HIV (Kefale et al., Reference Kefale, Damtie, Yalew, Adane and Arefaynie2020). Also, people who are educated may possibly get their knowledge on HIV testing from school-based HIV/AIDS prevention programmes (Kefale et al., Reference Kefale, Damtie, Yalew, Adane and Arefaynie2020). There is the need to design public health interventions, such as creating more community health posts and information centres where less-educated individuals could be educated on the virus and the lifetime and economic consequences of HIV/AIDS and the importance of testing for HIV.
Furthermore, corroborating other previous studies (Yaya et al., Reference Yaya, Bishwajit, Danhoundo, Shah and Ekholuenetale2016; Agegnehu et al., Reference Agegnehu, Geremew, Sisay, Muchie, Engida and Gudayu2020; Kefale et al., Reference Kefale, Damtie, Yalew, Adane and Arefaynie2020), the study found that men who were exposed to newspapers, radio, and television almost every day were more likely to test for HIV. A possible reason for this could be that those who are exposed to mass media may be exposed to educative contents that aids their understanding of HIV/AIDS, especially with its mode of acquisition and spread, available testing options and living with the virus (Kefale et al., Reference Kefale, Damtie, Yalew, Adane and Arefaynie2020). This highlights the importance of education through mass media as a tool to significantly improve the prevalence of HIV testing in sub-Saharan African countries. The finding that men who used condoms, and also men who had multiple sexual partners, were more likely to test for HIV supports the findings of a previous cross-sectional study in Mozambique by Agha (Reference Agha2012). A possible reason for this is that men who use condoms and have multiple sexual partners are aware that they may be more exposed to HIV/AIDS, and hence their willingness to go for an HIV test.
Akin to other previous studies (Agegnehu et al., Reference Agegnehu, Geremew, Sisay, Muchie, Engida and Gudayu2020), the study found that men in the poorest wealth quintile had the lowest odds of testing for HIV. A possible reason for this could be that poor individuals may not be able to afford the transport costs to and from health service centres for HIV testing since these are often located far away in sub-Saharan African countries (Agha, Reference Agha2012). The scaling up of self-testing and the deployment of cheap rapid diagnostic/testing kits in all parts of SSA to enable individuals to conduct their own HIV test, coupled with strategies to either reduce transport costs or provide free transport to and from health service centres for HIV testing in sub-Saharan African countries, could be steps in the right direction to improve HIV testing among the poor individuals in the communities.
Research has shown that urban residents are more likely to have adequate knowledge of HIV/AIDS and have the self-efficacy to adhere to HIV/AIDS education and test for HIV (Yaya et al., Reference Yaya, Bishwajit, Danhoundo, Shah and Ekholuenetale2016; Kefale et al., Reference Kefale, Damtie, Yalew, Adane and Arefaynie2020). Surprisingly, the present study found that those residing in urban areas were less likely to test for HIV compared with those in rural areas. This finding contradicts the finding of previous studies (Yaya et al., Reference Yaya, Bishwajit, Danhoundo, Shah and Ekholuenetale2016; Kefale et al., Reference Kefale, Damtie, Yalew, Adane and Arefaynie2020). A possible reason for this could be the variations in geographical location, socio-cultural, and socioeconomic characteristics of the study areas.
The study had its strengths and limitations. Its main strength was its use of nationally representative data from 29 sub-Saharan African countries. The data collection technique and methodology employed by the DHS followed best practice by experienced and well-trained data collectors, resulting in a high response rate. The findings of this study can, therefore, be generalized to all men in SSA. Advanced statistical models that accounted for both individual and contextual factors were also employed. However, the study followed a cross-sectional study design and as such it was not possible to account for unobserved heterogeneity; causal interpretation cannot be deduced from the study findings. Also, the relationships established between the explanatory and dependent variables may vary over time.
In conclusion, after controlling for confounding factors, men in SSA with comprehensive knowledge of HIV/AIDS were found to be more likely to test for HIV compared with their counterparts who had no comprehensive knowledge of HIV/AIDS. To improve HIV testing among men in SSA as a crucial step towards the eradication of the virus and the attainment of the 95-95-95 by 2030 global target, this study recommends that policymakers and all stakeholders in SSA step up comprehensive HIV/AIDS knowledge education while ensuring that HIV testing services are cheap and easily accessible through the provision of self-testing kits and mobile or workplace testing programmes. Mass media could be key to facilitating this.
Acknowledgments
The authors are grateful to the MEASURE DHS project for granting free access to their original data.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Conflicts of Interest
The authors declare that they have no conflicts of interest. There are no financial, copyright, trademarks or patent implications arising from this research and no organization has any vested interest in this research.
Ethical Approval
Publicly available survey data were used, and ethical approval for the surveys was granted by the governments of the relevant countries and the US government. Further information about DHS data usage and ethical standards are available at http://goo.gl/ny8T6X.
Author contributions
JKT: formal analysis, writing of original draft, reviewing and editing, visualization. JBF: writing of original draft, reviewing and editing. EB: methodology, formal analysis, writing of original draft, reviewing and editing. CA: formal analysis, writing of original draft, reviewing and editing. AM: writing of original draft, reviewing and editing. BOA: conceptualization, methodology, formal analysis, writing, reviewing and editing, visualization. AS: conceptualization, methodology, formal analysis, writing, reviewing and editing, visualization.







