Introduction
In utero environments play an important role in determining health outcomes of the offspring. Adverse environments due to maternal dietary restrictions or stress during pregnancy are known to hamper fetal growth and development. Maternal under-nutrition not only increases the risks of lower birth weight and poorer birth outcomes but also raises the risk for developing chronic diseases later in life.Reference Gluckman, Hanson and Beedle1–Reference Roseboom, de Rooij and Painter3
During Ramadan, pregnant Muslims undergo important nutritional and lifestyle changes. Ramadan is an annual period of daytime fasting that lasts for a month. Eating, drinking, smoking, and sexual activity are prohibited from dawn to sunset. Ramadan is both a religious festival and a moment for spiritual activities and self-restraint.Reference Azizi4 Beside changing nutritional intake, it also involves alterations in sleeping patterns and physical activity levels as people tend to be more active at night.Reference Al-Hourani and Atoum5–Reference Alkandari, Maughan, Roky, Aziz and Karli8 Meal frequency is usually reduced to twice a day: a large meal is taken when breaking the fast at sunset and a smaller meal at “sahoor” before the sun rises. Traditional meals during this month are often high in sugar and fat. In the Northern hemisphere, fasting is most difficult to perform during summer due to the longer days and higher temperatures.
The great majority of pregnant Muslim women have pregnancies that overlap with Ramadan, and although they are permitted to postpone their fasting,Reference Azizi4 many choose to fast. The proportion of pregnant Muslim women who fast for at least a day during Ramadan ranges from 50%–70% (in Iran, the Netherlands) to 70%–90% (in England, Singapore, US, Gambia, and Yemen).Reference Kavehmanesh and Abolghasemi9–Reference Makki13 Even women who postpone their Ramadan fast until after pregnancy experience lifestyle changes during Ramadan, although less pronounced so, as their dietary, physical activity, and sleeping patterns change and as they may experience altered stress levels. This might also affect the women and their unborns. Most of the existing literature on effects of Ramadan on the offspring is not able to distinguish between effects due to fasting and effects due to other lifestyle changes.
There have recently been a growing number of studies into the possible health effects of Ramadan during pregnancy. The dietary intake and weight gain of fasting pregnant women are reduced,Reference Kiziltan, Karabudak and Tuncay14 , Reference Khoshdel, Kheiri, Hashemi-Dehkordi, Nasiri, Shabanian-Borujeni and Saedi15 and fasting has been associated with several metabolic alterations including reduction in serum glucose, insulin, lactate, and carnitine levels, as well as elevation in serum triglyceride, cortisol, and leptin concentrations.Reference Kiziltan, Karabudak and Tuncay14 , Reference Khoshdel, Kheiri, Hashemi-Dehkordi, Nasiri, Shabanian-Borujeni and Saedi15
Most previous studies on Ramadan and birth outcomes were small and included only births within a limited time period, which allowed for only a limited correction for the confounding effects of seasonality. In the present study, we use data from a nationwide registry over an 11-year time period to evaluate birth outcomes of all babies born to mothers of Turkish and Moroccan descent (grouped together under the label “Mediterranean”) in the Netherlands whose pregnancies overlapped with Ramadan, irrespective of lifestyle changes.
Previous large studies on Ramadan and birth outcomes provided mixed results: a study from the USA found a slightly lower birth weight and a lower fraction of male births.Reference Almond and Mazumder11 A study with over 1,000,000 babies born to Muslims in Germany found no such effects.Reference Jürges16 Several smaller studies showed no effects of Ramadan during pregnancy with regard to birth weight and risk of low birth weight (LBW),Reference Kavehmanesh and Abolghasemi9 , Reference Kiziltan, Karabudak and Tuncay14 , Reference Cross, Eminson and Wharton17 , Reference Ozturk, Balat and Ugur18 nor with respect to amniotic fluid volume,Reference Mirghani, Weerasinghe, Smith and Ezimokhai19 uterine arterial blood flow,Reference Mirghani, Salem and Weerasinghe20 and Apgar score.Reference Malhotra, Scott, Scott, Gee and Whaton21 But, other studies did find lower birth weights,Reference Savitri, Yadegari and Bakker10 reduced fetal breathing movements,Reference Mirghani, Weerasinghe, Smith and Ezimokhai19 , Reference Mirghani, Weerasinghe, Ezimokhai and Smith22 lower placental growth,Reference Alwasel, Abotalib and Aljarallah23 and decreased amniotic fluid volume.Reference Sakar, Gultekin and Demir24 The discrepancies between these results may be due to differences in length of daylight and fast during Ramadan, background characteristics of the population, and local nutritional and cultural habits associated with Ramadan. In order to inform pregnant women who are considering fasting during Ramadan as well as their obstetric health care providers, it is important to collect information on this issue in settings that resemble their own.
In a related literature, several large studies investigated long-term implications for the offspring and found poorer cognitive performances among childrenReference Almond, Mazumder and van Ewijk25 , Reference Majid26 and higher child mortality rates.Reference Schoeps, Van Ewijk, Kynast-Wolf, Nebié, Zabré and Sié27 Among adults, prenatal Ramadan exposure was associated with poorer health, including poorer lung functionalities and increased occurrences of disabilities and of symptoms of type 2 diabetes and coronary heart problems.Reference Almond and Mazumder11 , Reference van Ewijk, Painter and Roseboom12 , Reference Pradella and van Ewijk28 , Reference van Ewijk29
Here, we set out to investigate whether Ramadan exposure in pregnancy had effects on perinatal outcomes among women of Moroccan and Turkish descent in the Netherlands.
Methods
Study population
We analyzed data from the Perinatal Registry of the Netherlands (Perined), a nationwide registry that includes maternal, obstetric, postpartum, and neonatal information of all deliveries in the Netherlands from January 2000 through December 2010. Midwives, general practitioners, and obstetricians who provided antenatal care and assistance during childbirth completed a form, based on data they had collected from history taking, clinical and laboratory examination, as well as diagnosis and intervention. Perined includes all births (live births and stillbirths) that occur after 16 weeks of gestational age, and it contains approximately 96% of all births in the Netherlands.30
In the Perined database, mothers’ ethnicities are registered as either Dutch or other European ethnicities, Mediterranean (which refers to being of Turkish/Moroccan descent), Creole, Indian, Asian, or other. We restricted the analyses to Mediterranean and Dutch babies and excluded babies from all other ethnicities. In the Netherlands, over 95% of people of Moroccan and Turkish descent are Muslims.Reference Dagevos and Gijsberts31 Although “Mediterranean” is used to refer to a Turkish or Moroccan background, some people from other origins who are usually not Muslim, such as Spanish or Italians, may still be classified into this group. However, they form only a very small share of Mediterraneans in the Netherlands (0.4% of the Dutch population are of Spanish or Italian decent). According to Statistics Netherlands, during our study period, 7.4% of all mothers of newborns had a Turkish or Moroccan background,32 whereas 7.0% of all babies in our data were Mediterranean. This confirms that in the Dutch context, Mediterranean is a good proxy for being Muslim.
All babies (live births and stillbirths) with a gestational age of 22+0 weeks onwards were included in the analyses, except for those analyses in which only live births were analyzed (Apgar score < 7 and prematurity). To obtain information on socioeconomic status (SES) (income) at the postal code level, the Perined data were complemented with data from Statistics Netherlands.
Ramadan exposure
As no information on fasting or other behavioral changes during Ramadan was available, Ramadan exposure was based on real overlap between Ramadan and gestation. Gestation begins at the estimated date of conception, calculated as 14 days after the start of women’s last menstrual period, and ends at the date of birth. Pregnancies were classified as overlapping with Ramadan if at least one day of pregnancy coincided with a Ramadan. Babies who were conceived within 7 days after Ramadan were controlled for in the analyses as the possibility cannot be excluded that their health was still affected by Ramadan. Our approach for measuring prenatal Ramadan exposure differs from most previous research, where only date of birth could be used to establish whether a Ramadan had occurred during a pregnancy. An assumption then had to be made about the length of gestation: usually that each pregnancy lasted for 266 days. In our study, date of conception is known as well, which allows us to more exactly determine whether a Ramadan has occurred during a pregnancy.
A binary classification for Ramadan exposure is more appropriate than measuring exposure using the total days of overlap between Ramadan and gestation, since experiencing fewer than the 29 or 30 days of an entire Ramadan is only possible if a child was conceived or born during a Ramadan. Hence, the number of days of overlap would be associated with the phase of pregnancy during which Ramadan occurred. To study effect heterogeneity by phase of pregnancy, a further Ramadan exposure classification using trimesters was made according to the trimester that most of the Ramadan period coincided with. In order to end up with three equally long trimesters, days 1–88 of pregnancy were considered as trimester 1, days 89–177 as trimester 2, and day 178 and later as trimester 3. In cases where the number of days of overlap between Ramadan and pregnancy trimester was the same for two trimesters, the overlap was classified to occur in the earlier trimester.Footnote 1
Following the definition of our exposure variables, we measured the effect of pregnancy overlap with Ramadan on perinatal outcomes. We were uninformed about the actual fasting behavior. The most likely channel through which Ramadan occurrence during pregnancy is hypothesized to have an effect is through nutritional channels,Reference Trepanowski and Bloomer6 , Reference Alkandari, Maughan, Roky, Aziz and Karli8 but there may be alternative channels such as modifications in sleeping patterns,Reference Roky, Chapotot, Hakkou, Benchekroun and Buguet7 physical activity level,Reference Al-Hourani and Atoum5 and increased consumption of foods containing high levels of sugar, fat, and salt.Reference Bakhotmah33 , Reference Alwasel, Abotalib and Aljarallah34 However, in this study, we cannot distinguish between these channels. Our results should be regarded as intention-to-treat estimates. That is, we make the assumption that all Muslims for whom a Ramadan occurred during pregnancy underwent the impact of Ramadan. This approach has been widely used in large-scale studies on long-run effects of Ramadan during pregnancy on the health of the offspring.Reference Almond and Mazumder11 , Reference Almond, Mazumder and van Ewijk25–Reference Schoeps, Van Ewijk, Kynast-Wolf, Nebié, Zabré and Sié27 , Reference Greve, Schultz-Nielsen and Tekin35 , Reference Schultz-Nielsen, Tekin and Greve36 As the measure of exposure (Ramadan occurrence during pregnancy) utilized is uncorrelated with maternal characteristics such as SES, religious observance, and health, this approach helps avoid confounding due to these variables.Reference Almond and Mazumder11 , Reference Almond, Mazumder and van Ewijk25 , Reference van Ewijk29
A difference with previous research is that we utilize actual overlap between Ramadan and pregnancy. This was impossible in earlier studies where date of conception was unknown and overlap was calculated based on Ramadan occurrence during the 266 days before birth. In those studies, results were biased toward zero as children conceived shortly after a Ramadan and born prematurely are incorrectly categorized as exposed.Reference van Ewijk, Painter and Roseboom12 , Reference van Ewijk29 We avoid this bias. However, as we will detail in the Data analysis subsection, our approach hinges on the assumption that there is no causal effect of prenatal Ramadan exposure on gestational length. We investigate this and show that there is indeed no such effect.
When investigating these effects on gestational age, we have to define exposure in a different way because a shorter gestation mechanically leads to a lower probability of having an overlap with Ramadan. – It must be noted that a mechanical relation, as opposed to a causal relation, does not bias the results from our main approach. We will explain this further in the Data analysis subsection. – When gestational length is the dependent variable, we define exposure as the occurrence of a Ramadan during the 266 days after date of conception.
Outcome measurement
Outcome measures of fetal growth were birth weight, occurrence of LBW (birth weight lower than 2500 g), and small for gestational age (SGA; birth weight below the 10th percentile for gestational age). Outcome measure of neonatal health was the occurrence of an Apgar score lower than 7. Further outcome measures were: a dummy variable indicating whether the child was male, any congenital anomalies, mild congenital anomalies, severe congenital anomalies, gestational duration, prematurity (born at less than 37+0 weeks of gestation), and perinatal mortality (occurrence of stillbirth or death during delivery or within 7 days after birth). Mild congenital anomalies include disorders of the eyes, ears, skin defect, cleft palate, or other organs, which are not life-threatening. Severe congenital anomalies consist of serious or potentially lethal disorders such as anencephaly, microcephaly, congenital cardiac defects, and disorders of the respiratory tract. Gestational duration was based on either ultrasound dating or the time since women’s last menstrual period.
Data analysis
Maternal characteristics, pregnancy complications, and babies’ characteristics were tabulated by Ramadan exposure for descriptive purposes, within Mediterranean and Dutch pregnancies separately.
We used linear regressions to analyze continuous dependent variables and logistic regressions to analyze binary dependent variables. Included covariates are month of conception (using a set of 11 indicator variables), maternal age, maternal age squared, baby’s sex (except when sex was the outcome variable), average income based on postal code (SES), parity, year of delivery, maternal smoking, and conception within 7 days after Ramadan. As the likelihood of Ramadan exposure is mechanically correlated with gestational age at delivery (the larger the gestational age at delivery, the higher the probability of experiencing a Ramadan), controlling for gestational length is essential to avoid bias. That is, duration of gestation influences the probability that a pregnancy overlaps with Ramadan, while it is also correlated with most of the outcomes. Not adequately controlling for gestational age therefore leads to a confounding of Ramadan effects with gestational age effects. We therefore additionally control for gestational length, gestational length squared, and gestational length cubed.
As Wilcox et al. (2011) show, adjusting for gestational length may bias effects of prenatal exposures on birth outcomes if the prenatal exposure affects gestational length, while there are unobserved factors that both affect gestational length and directly affect birth outcomes.Reference Wilcox, Weinberg and Basso37 Gestational age in that case acts as a collider variable. For our analysis strategy to yield unbiased results, we therefore need to exclude the possibility that prenatal Ramadan exposure affects gestational length. We run analyses with gestational age at delivery itself and prematurity as the outcomes. In these regressions, it is impossible to control for gestational length. For analyses on these outcomes, exposure to Ramadan is defined based on whether a Ramadan occurred during the 266 days after the calculated date of conception, with 266 days being the average length of human gestation. This intention-to-treat approach is necessary to avoid the reverse causality that would otherwise arise (shorter pregnancies are less likely to include a Ramadan). It is important to note that the intention-to-treat approach does not lead to an artificial over representation of preterm births among the exposed group. Hence, it does not lead to an upward bias. But, it may lead to a bias toward finding no effects. That is, some children for whom Ramadan would have occurred very late in an at-term pregnancy will be born prematurely before the start of Ramadan. We incorrectly classify them as exposed. If actual Ramadan exposure would have further shortened their gestations, we miss this effect and hence under estimate the effect of Ramadan on gestational length.
As we classified exposure using whether Ramadan occurred during pregnancy, it is essential to separate seasonal effects from true Ramadan effects. Seasonality is known to be associated with various pregnancy outcomes, particularly birth weight and preterm birth.Reference Strand, Barnett and Tong38 , Reference Chodick, Flash, Deoitch and Shalev39 Since Ramadan is based on the Islamic Lunar calendar, it shifts forward by approximately 11 days each year and occurs during each period of the Gregorian calendar over a 33-year cycle. Hence, if about 33 cohorts are available, controlling for month of conception suffices to separate Ramadan from seasonal effects. Our data, however, contain only 11 birth cohorts (2000–2010), so that Ramadan always fell between 11 August and 7 January in the relevant years. Controlling for month of conception might therefore not be sufficient. Therefore, similar to previous literature in this domain,Reference Jürges16 , Reference Almond, Mazumder and van Ewijk25 , Reference Schoeps, Van Ewijk, Kynast-Wolf, Nebié, Zabré and Sié27 , Reference Pradella and van Ewijk28 , Reference Greve, Schultz-Nielsen and Tekin35 we use a “difference-in-differences” strategy to overcome this problem. We include non-Muslims (proxied using ethnic Dutch) in all regressions. The regressions control for an indicator for “a Ramadan occurred during pregnancy” and an indicator for religion. All other covariates are interacted with the religion indicator. The religion*exposure interaction term compares the strength of the association between Ramadan during pregnancy and birth outcomes between Muslims and non-Muslims. As non-Muslims do not observe Ramadan, potential associations between Ramadan during pregnancy and birth outcomes in this group are due to residual confounding with seasonality. A similar pattern of artificial associations will exist among the Muslims as seasonality patterns are likely similar in both groups in the Netherlands. A difference-in-differences analysis takes the association between Ramadan and birth outcomes among Muslims and subtracts the part of these associations that is due to seasonality, as it is measured among the non-Muslims. Thus, it “cleans” the associations between Ramadan and health outcomes among Muslims from all remaining seasonality.Reference Jürges16 , Reference Almond, Mazumder and van Ewijk25
As a robustness check, we also conducted all regressions on the Muslims-only sample without doing difference-in-differences. These regressions may not adequately adjust for seasonality. Results are expressed as linear regression coefficients or odds ratio with 95% confidence intervals and P values. All analyses were done using Stata/SE 11.1.
Results
The Perined data contained 1,987,124 babies. Non-Mediterranean and non-Dutch babies (n = 224,505), twins and triplets (n = 68,810), babies with uncertain length of gestation, and babies with miscoded gestational lengths (n = 73,052) were excluded leaving 1,620,757 babies for analysis of whom 139,322 were Mediterranean babies. Baseline characteristics are shown in Table 1. Ramadan overlapped with 83.3% of all gestations of Mediterranean mothers and slightly less among Dutch mothers.
Table 1. Descriptives
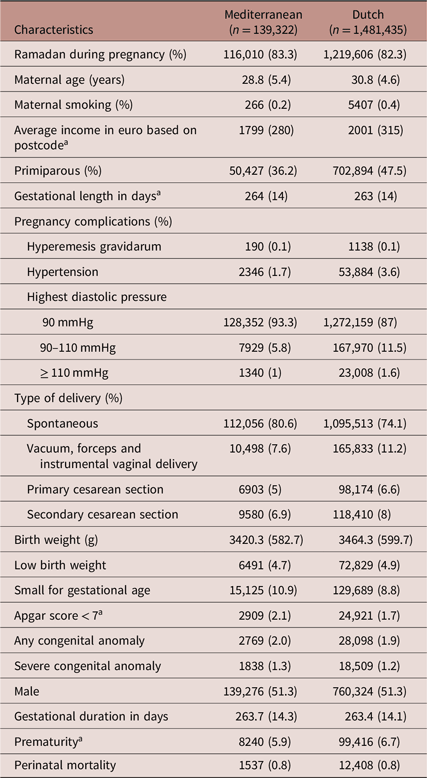
Table shows means (standard deviations) for continuous variables and frequencies (percentages) for binary variables. In case of skewed data (a), medians and interquartile ranges are presented. All differences between Mediterranean and Dutch are significant at the 1%-level (t-tests for continuous variables and χ 2-tests for categorical variables), except for severe congenital anomaly (P = 0.03) and male (not significant).
a Only live births were included.
Table 2 shows the adjusted associations between pregnancy during Ramadan and birth outcomes among Muslims from the difference-in-differences regressions. Muslim newborns with, compared to those without, a Ramadan during pregnancy did not differ in terms of gestational duration. This implies that gestational age cannot have confounded results for the other outcomes by acting as a collider variable.Reference Wilcox, Weinberg and Basso37 Exposed and not-exposed did also not differ in their birth weights, probabilities of having a LBW, being SGA, having an Apgar score < 7, having any congenital anomaly, or a mild congenital anomaly, being male, being premature, or suffering perinatal death. Severe congenital anomalies occurred more frequently after Ramadan exposure, especially for the third trimester exposure. But, this association lost statistical significance after a Bonferroni-Holm correction for multiple testing.
Table 2. Associations between Ramadan occurrence during pregnancy and birth outcomes among Muslim newborns, based on difference-in-differences analyses

Table shows linear regression coefficients for continuous outcomes (birth weight and gestational duration) and odds ratios from logistic regressions for binary outcomes (all other variables). Between brackets, 95% confidence intervals are shown. The columns “First/second/third trimester” for each outcome come from the same regression.
* P < 0.05.
** P < 0.01.
a Only live births were included.
Appendix Table A1 shows the results from regressions in which only Muslims are included without difference-in-differencing. Muslims who had been in utero during gestation had slightly higher birth weights and shorter gestational lengths and were less frequently SGA than unexposed Muslims. They also more often had severe congenital anomalies. However, these regressions may not have sufficiently been adjusted for confounding with season of birth/season of conception. More light is shed on this in Appendix Table A2, which shows the coefficients for the ethnic Dutch from the difference-in-differences regressions presented in Table 2. Coefficients should be interpreted as a comparison between non-Muslims who were in utero during a Ramadan and non-Muslims who were not. No causal effect of Ramadan can be expected in this group: they were included in the difference-in-differences regressions to take out potential confounding due to seasonal effects that are the same among Muslims and non-Muslims. With the exception of the result for severe congenital anomalies, the same pattern of associations appeared among the non-Muslims as among the Muslims in Appendix Table A1. This confirms that the non-difference-in-differences regressions do not sufficiently adjust for seasonality and should be interpreted with caution.
Discussion
Among Mediterranean women in the Netherlands (who are in great majority Muslims with a Turkish or Moroccan background), we found that pregnancy overlap with Ramadan was not associated with adverse pregnancy outcome, including LBW, perinatal asphyxia, and preterm birth.
Ramadan during pregnancy initially seemed associated with an 18% increase in risk for severe congenital anomalies. However, this association lost statistical significance after adjusting for multiple testing. Moreover, this pattern was particularly present for exposure in the third trimester. Consequently, this increase in severe congenital anomalies cannot be explained by the exposure, since virtually all congenital anomalies originate during embryogenesis in early pregnancy. Therefore, the association found between Ramadan exposure and severe congenital anomalies is more likely an artifact due to multiple testing. Our finding of no association between Ramadan exposure and risk of mild congenital anomalies also supports this conclusion.
During Ramadan, Muslims observe lifestyle changes, which include nutritional disturbances, modifications in sleeping patterns, and decreased levels of physical activity. The main channel through which Ramadan exposure is hypothesized to have an effect is through nutritional restrictions. Other potential channels may include modifications in sleeping patterns and increased consumption of foods containing high levels of sugar, fat, and salt. Furthermore, since smoking is prohibited during fasting, Ramadan exposure may lead to a reduction in direct and secondhand smoke exposure. Finally, Ramadan may also affect the fetus via effects on maternal stress levels. We cannot distinguish between these channels, but can only conclude that together, these exposures do not seem to have an effect on newborns’ health.
This study is among the first to investigate the association between Ramadan exposure during pregnancy with birth outcomes using data on a substantial number of cohorts from a national registry. Our large sample size gave our analyses a substantial statistical power. Previous large-scale studies determined exposure based on whether a Ramadan occurred during the 266 days before birth, which equals the average length of human gestation. Our data included both date of birth and date of conception information so that we were able to determine actual occurrence of a Ramadan during pregnancy. Availability of a set of important covariates in the dataset and adjustment for seasonality utilizing a difference-in-differences approach allowed for adequate adjustments.
Three limitations of our study are first, that no data about religion were available, so that Mediterranean ethnicity was used as a proxy for being Muslim. This approach leads to some misclassification. Although Mediterranean should refer to a Turkish or Moroccan descent, some people with a different background may have been included, too. 7.0% of all babies in our data were Mediterranean. As this is slightly less than the 7.4% of newborns who, according to official nationwide statistics, were of Turkish and Moroccan descent,40 this suggests that our category Mediterranean is unlikely to have included many women from other ethnic groups. Moreover, a few percent (probably less than 5%) of people of Turkish or Moroccan descent in the Netherlands are non-Muslims.Reference Dagevos and Gijsberts31 The associated misclassification causes a slight bias toward finding no effects.
Second, Ramadan shifts through the entire Gregorian calendar over a 33-year cycle. An availability of about 33 birth cohorts would therefore have allowed us to completely separate seasonality from Ramadan effects by controlling for month of conception. There are, however, only 11 cohorts in our data. The difference-in-differences analysis strategy in which non-Muslims are used to partial out seasonality patterns should have solved this issue: it may be noticed that using a similar number of cohorts and a similar methodology, previous studies did demonstrate long-run effects of prenatal Ramadan exposure.Reference Almond, Mazumder and van Ewijk25 Nevertheless, it must be noted that the relatively limited number of available cohorts in this study is a limitation.
Third, actual measurements on mothers’ fasting behaviors were not available. If Ramadan mainly has an effect through the nutritional restrictions channel, our results underestimate potential effects of Ramadan fasting because not all pregnant Muslims in the Netherlands fast during Ramadan, while some of those who do fast, only fast for a few days of this month.Reference Savitri, Yadegari and Bakker10 The majority of Muslims in the Netherlands are of Moroccan and Turkish origin (31% and 38%, respectively).Reference van Herten41 , Footnote 2 Of these, around 79% and 22% are estimated to fast during their pregnancies, respectively.Reference Savitri, Yadegari and Bakker10 The implicit assumption in our analyses is that all Muslim mothers who were pregnant during a Ramadan were affected by it. Our estimates should therefore be regarded as conservative (lower-bound) estimates.Reference van Ewijk, Painter and Roseboom12 An important advantage of this approach is that it avoids confounding effects of fasting with systematic differences between Muslims who do versus do not choose to fast during pregnancy.Reference Almond and Mazumder11 But, the downside is that our intention-to-treat approach may have led to a bias toward finding no effects.
The fact that some studies found effects of prenatal Ramadan exposure on perinatal outcomes, where others, including our own study, found no effects, could be explained by a number of factors. Comparing our results to those from previous studies with large sample sizes and statistical power that were adequately able to separate effects of Ramadan exposure from those of seasonal variation, we note that our findings of no decrease in birth weight after prenatal Ramadan exposure and no effects on the sex ratio are confirmed by a recent study on Muslims in Germany.Reference Jürges16 However, a study from Michigan reported slightly lower birth weights (about 18 g) after prenatal exposure and a lower fraction of male births among Muslims conceived during Ramadan.Reference Almond and Mazumder11 Muslims in the Michigan study were mainly of Arab/Middle Eastern ancestry and may have had different fasting behaviors and lifestyle changes than the Muslims in our sample, which were mainly of Turkish and Moroccan ancestry. Muslims in the German study mostly had Turkish backgrounds. The effects of Ramadan during pregnancy on perinatal outcomes may therefore depend not only on specific behavioral patterns during Ramadan such as the percentage of Muslim women fasting during Ramadan, types of nutrition consumed during the breaking of the fast (e.g. glycemic index), but also altered smoking, sleeping, and physical activity patterns, as well as stress experiences.
Effects may also be heterogeneous by sex of the child or by parental SES, or effects may only occur in the lower parts of the outcome distribution.Reference Majid, Behrman and Mani42 We found no evidence for the latter when taking LBW or SGA as dependent variables. The absence of effects on the sex ratio suggests that gender-specific effects are unlikely. We also explored effect heterogeneity by average income in the postal code area where mothers lived as a proxy for SES and found no evidence for effect heterogeneity.
Previous studies found that Ramadan during pregnancy is associated with a wide range of long-term adverse health effects on the offspring, including increased rates of disabilities,Reference Almond and Mazumder11 a poorer cognitive performance,Reference Almond, Mazumder and van Ewijk25 , Reference Majid26 , Reference Greve, Schultz-Nielsen and Tekin35 higher child mortality rates,Reference Schoeps, Van Ewijk, Kynast-Wolf, Nebié, Zabré and Sié27 and increased prevalence of the symptoms of coronary heart problems and type 2 diabetes.Reference van Ewijk29 The present study found no associations with health outcomes at birth. Previous studies also found no or small effects on newborns’ outcomes. This raises the possibility that prenatal exposure to Ramadan could cause long-term health effects without having effects on perinatal outcomes. A similar pattern of no effects on birth weight but long-term health effects has previously also been demonstrated in other instances of maternal nutritional change during pregnancy.Reference Roseboom, Painter, van Abeelen, Veenendaal and de Rooij43 , Reference Persson, Arifeen, Ekström, Rasmussen, Frongillo and Yunus44
In conclusion, our study, in line with other large population-based cohorts, found no effect of maternal exposure to Ramadan on perinatal outcomes. The fact that the absence of perinatal effects does not rule out effects on offspring health in later life, in combination with the fact that large numbers of pregnancies each year are exposed to Ramadan, warrants specific attention for follow-up of pregnancies exposed to Ramadan in future studies.
Acknowledgments
This work has benefited from support by the German Research Foundation, DFG, via grant number 260639091.
Conflicts of interest
The authors declare no potential conflicts of interest.
Appendix
Table A1. Associations between Ramadan occurrence during pregnancy and birth outcomes among Muslim newborns, based on analyses that only included Muslims
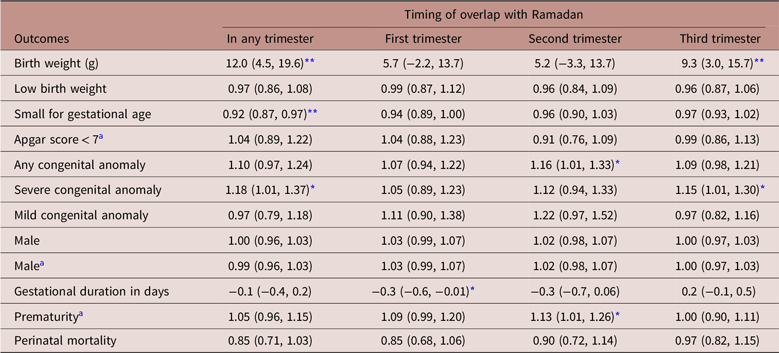
Table shows linear regression coefficients for continuous outcomes (birth weight and gestational duration) and odds ratios from logistic regressions for binary outcomes (all other variables). Between brackets, 95% confidence intervals are shown. The columns “First/second/third trimester” for each outcome come from the same regression.
Table A2. Associations between Ramadan occurrence during pregnancy and birth outcomes among ethnic Dutch newborns, based on difference-in-difference analyses

Results presented in this table come from the same regressions as those in Table 2. The table shows linear regression coefficients for continuous outcomes (birth weight and gestational duration) and odds ratios from logistic regressions for binary outcomes (all other variables). Between brackets, 95% confidence intervals are shown. The columns “First/second/third trimester” for each outcome come from the same regression.







