Introduction
Obesity is a significant global public health concern, with the prevalence increasing from less than 3 % in 1975 to 11 % in 2016 among men and from 6 to 15 % among women(1,Reference Jaacks, Vandevijvere and Pan2) . It is associated with several chronic diseases, including cancer(Reference Calle and Kaaks3), diabetes(Reference Verma and Hussain4,Reference Hossain, Kawar and El Nahas5) , heart disease(Reference Lavie, Arena and Alpert6) and respiratory diseases(Reference Peters, Suratt and Bates7). To address the consequences of the global obesity epidemic, it is crucial to understand how obesity leads to chronic diseases and develops effective prevention and treatment strategies.
The reasons behind obesity-related micronutrient deficiency remain unclear. Studies have suggested that overweight or obesity might affect micronutrient concentrations through imbalanced dietary intake, absorption, distribution, metabolism or excretion(Reference Olusi8–Reference Ledikwe, Blanck and Khan12). Overweight and obese adults have been found to have higher odds of low serum concentrations of micronutrients such as alpha-carotene, beta-carotene, beta-cryptoxanthin, lutein/zeaxanthin, total carotenoids, vitamin C, selenium and folate compared with normal-weight adults(Reference Kimmons, Blanck and Tohill13). A study in Australia found that BMI was negatively correlated with serum concentrations of vitamin D, folate, magnesium and potassium(Reference McKay, Ho and Jane14). Other studies have also reported varying levels of micronutrient deficiency among obese individuals(Reference Moor de Burgos, Wartanowicz and Ziemlański15–Reference Al-Delaimy, van Kappel and Ferrari19). Some studies have focused on micronutrient intake in overweight or obese individuals, with one finding no correlation between BMI and intake of micronutrients in both men and women(Reference McKay, Ho and Jane14). Another study using the US National Health and Nutrition Examination Survey data found that vitamins A, B1, B2, B12 and D were negatively associated with the risk of obesity(Reference Tang, Zhan and Wei20).
Studies have indicated that obesity can cause imbalanced concentrations of micronutrients, potentially due to altered dietary intake, absorption, distribution, metabolism or excretion(Reference Olusi8–Reference Ledikwe, Blanck and Khan12). Prioritising dietary intake as the most modifiable factor from a public health perspective, we conducted a study using NAHSIT data to investigate the relationship between overweight/obesity and adherence to dietary reference intake (DRI) for selected micronutrients. Our hypothesis was that overweight/obese individuals might exhibit varied levels of adherence to DRI for these micronutrients.
Methods
Participants
The Nutrition and Health Survey in Taiwan (NAHSIT) was a population-representative survey in Taiwan investigating the nutritional status of the general population. We conducted a cross-sectional study using data from the NAHSIT 2013–2016. The survey method has been described elsewhere(Reference Li and Fang21). Briefly, a three-stage probability sampling strategy was used to achieve a representative sample for NAHSIT. The first stage was the selection of eight primary sampling units (townships and city districts) using probability proportional to size sampling methods. A total of 160 townships or city districts were chosen. The second stage was to randomly select several starting households to construct sampling clusters within each selected primary sampling unit. In the third stage, door-to-door visits were conducted to carry out interviews until the required number of the age and sex groups was reached. The Latin square design was used to allocate data collection times evenly over the four seasons to avoid seasonal variations that may affect dietary consumption and nutritional status.
The study population of NAHSIT was non-institutionalized Taiwanese nationals. NAHSIT also collected demographic data including age, sex, education, marital status and family income through face-to-face interviews. All participants attended a physical examination at a temporary health examination station, where body mass index (BMI) and waist circumference (WC) data were collected by either nurses or trained staff.
The diagram of the sample selection process is shown in Supplementary Figure S1. The number of participants in the NAHSIT survey was 11 072. The study participants in the present study were restricted to adults aged 19 and above according to the definition of adults adapted from the newest version of daily food guides (n 5770). Participants with complete demographic data, BMI and WC data, and 24 h dietary recall data were included in the final analysis, resulting in a total of 3075 study participants.
Definition of overweight and obesity
Overweight or obesity was defined using BMI or WC according to the criteria of the Ministry of Health and Welfare in Taiwan(Reference Li, Chen and Chang22–Reference Lin, Lee and Chen24). Study participants were grouped into four groups: underweight (BMI < 18⋅5 kg/m2), normal (18⋅5 ≤ BMI < 24 kg/m2), overweight (24 ≤ BMI < 27 kg/m2) and obese (BMI ≥ 27 kg/m2). Moreover, we also used WC to define obesity and examine if similar results were observed. WC ≥ 90 cm for men and WC ≥ 80 cm for women were defined as obesity.
Assessments of nutrient intakes
A validated 24 h dietary recall method was used to estimate the intakes of selected nutrients of study participants(Reference Huang, Lee and Pan25–Reference Chang, Suchindran and Pan27). To address the potential intra-individual variance in estimating usual daily intakes using the 24 h recall data, repeated surveys were conducted for adjustment of the data. The NAHSIT randomly selected participants among different age groups (0–6, 7–12, 13–18, 19–64 and ≥65) from each sampling unit and conducted a repeated 24 h recall survey one week after the first survey. The correlations between two 24 h recall surveys were used to adjust the variance of daily dietary intakes(Reference Chang, Suchindran and Pan27).
Fourteen nutrient intakes, including vitamins A, C, D, E, B1, B2, B3, B6 and B12, iron, magnesium, zinc, calcium and phosphorus were evaluated in NAHSIT. We did not evaluate the other nutrients was because that only these nutrient intake data were available in the NAHSIT dataset. In the present study, we examined the associations of overweight or obesity with the chance of adherence to the DRIs (8th edition in Taiwan). The DRIs were established by the Taiwan Food and Drug Administration (FDA) of the Ministry of Health and Welfare and were publicly accessible(28). The DRIs for selected nutrients are shown in Supplementary Table S1. The DRI adherence was estimated by the prevalence of participants whose intake was lower than the recommended dietary allowance (RDA) or adequate intakes (AIs) for selected micronutrients.
Statistical analysis
We categorised BMI into four groups (underweight, normal weight, overweight and obesity) based on standard definitions. We used the χ2 or Fisher's Exact test to examine the associations between different BMI categories and personal characteristics and conducted stratified analyses by sex. Confounding factors were selected based on prior knowledge and their potential influence on the exposures and outcomes. Finally, we fitted logistic regression models to assess the associations between BMI categories and inadequate intakes of micronutrients, adjusting for age (19 ≤ age ≤ 30, 31 ≤ age ≤ 50, 51 ≤ age ≤ 70 and age ≥ 71), education level (elementary school, junior high and high school, college or above), marital status (single, married or lived together, divorced, separated, widowed or refused to answer) and family income (income < NT $40 000, NT $40 000 ≤ income < NT $80 000, income ≥ NT $80 000, don't know or refuse to answer). All analyses were performed using SAS 9⋅4 (SAS Institute, Cary, NC).
Results
A total of 3075 participants aged 19 and above were included in the final analysis (Table 1). Compared with normal-weight men, men with BMI of 27 kg/m2 and above were more likely to be older and to be married or lived together. Compared with normal-weight women, women with BMI of 27 kg/m2 and above were more likely to be older, tended to be less educated, more likely to be divorced, separated, widowed or refused to state marital status, and to have less family income. The median and interquartile range of micronutrient intakes among men and women are shown in Supplementary Table S2.
Table 1. Demographic descriptions of included study participants from the Nutrition and Health Survey in Taiwan (NAHSIT) 2013–2016 (n 3075)

NT, the New Taiwan dollars; BMI, body mass index.
The associations of baseline personal characteristics with different BMI groups were evaluated using χ2 or Fisher's Exact tests.
After adjusting for age, education level, marital status and family income, we found that obese men have a higher DRI adherence for vitamin B3 (odds ratio (OR) 1⋅70, 95 % confidence interval (CI) 1⋅29, 2⋅23; P-value < 0⋅001), Fe (OR 1⋅46, 95 % CI 1⋅06, 2⋅00; P-value = 0⋅02) and Zn (OR 1⋅41, 95 % CI 1⋅07, 1⋅85; P-value = 0⋅01), compared with normal-weight men. However, compared with normal-weight women, obese women have lower DRI adherences for vitamin C (OR 0⋅73, 95 % CI 0⋅56, 0⋅95; P-value = 0⋅02) and Mg (OR 0⋅72, 95 % CI 0⋅54, 0⋅95; P-value = 0⋅02). For the most micronutrient intakes, we found no difference between obese and normal-weight people in DRI adherence (Table 2).
Table 2. The associations between BMI groups and DRI adherence of selected micronutrients using data from the Nutrition and Health Survey in Taiwan (NAHSIT) 2013–2016
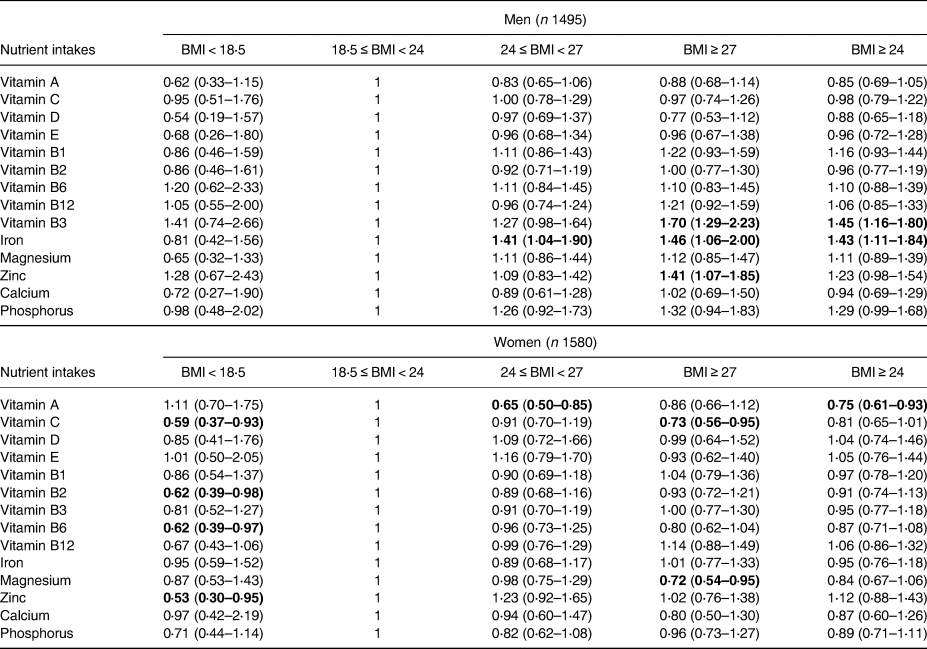
BMI, body mass index. Exposure variable: BMI groups; Outcome variable: DRI adherence. All the logistic regression models were adjusted for age, education level, marital status and family income. The values were presented as odds ratio (95 % confidence interval).
Bold values are statistically significant.
Table 3 shows similar findings using WC to define obesity. After adjusting for potential confounding factors, men with WC ≥ 90 cm had higher DRI adherences of vitamin B3 (OR 1⋅22, 95 % CI 1⋅01, 1⋅47; P-value = 0⋅04), vitamin B12 (OR 1⋅29, 95 % CI 1⋅07, 1⋅57; P-value < 0⋅01) and Fe (OR 1⋅33, 95 % CI 1⋅07, 1⋅65; P-value = 0⋅01). In contrast, women with WC ≥ 80 cm had lower DRI adherences of vitamin A (OR 0⋅82, 95 % CI 0⋅68, 1⋅00; P-value = 0⋅05) and Mg (OR 0⋅78, 95 % CI 0⋅64, 0⋅97; P-value = 0⋅02). For the other micronutrient intakes, we found no difference between obese and non-obese people in DRI adherence.
Table 3. The associations between WC groups and DRI adherence of selected micronutrients using data from the Nutrition and Health Survey in Taiwan (NAHSIT) 2013–2016

WC, waist circumference. Exposure variable: BMI groups; Outcome variable: DRI adherence. All the logistic regression models were adjusted for age, education level, marital status and family income. The values were presented as odds ratio (95 % confidence interval).
Bold values are statistically significant.
Discussion
In the present study, we found that men who were obese or overweight had a higher chance of adhering to the DRIs for vitamin B3, vitamin B12, iron and zinc, but not for most of the other selected nutrients. In contrast, obese women had a higher chance of having insufficient intakes of vitamin A, vitamin C and magnesium compared with normal-weight women. Similar findings were observed using WC as an indicator of obesity. One possible explanation is that obese individuals are more likely to consume high-energy foods that are usually nutritionally poor(Reference Ernst, Thurnheer and Schmid29). The most important contribution of our study is that we did not merely examine the associations between micronutrient intakes and obesity. Instead, we examined the associations between the chance of adherence to the official DRIs and obesity and found insufficient intakes of some micronutrients among obese women. We argue that this approach is superior because a simple negative association between specific micronutrient intakes and obesity cannot determine whether a deficiency exists.
Overweight and obesity have been linked to micronutrient deficiencies in previous studies, which typically proposed possible explanations from a biological mechanism standpoint(Reference García, Long and Rosado30). For instance, research has found that iron and vitamin D are sequestered in adipose tissues in obese individuals because iron is redistributed to different tissues(Reference García, Long and Rosado30–Reference Wortsman, Matsuoka and Chen32). Obesity may also lead to adipocyte dysfunction, which impairs adipose tissue functionality, sequestering fat-soluble vitamins in the adipocyte and reducing micronutrient concentrations in blood(Reference García, Long and Rosado30,Reference Haugen and Drevon33) . Many studies have focused on serum concentrations of micronutrients and their associations with obesity. In China, a study found that obese individuals had lower serum concentrations of vitamin A(Reference Wei, Peng and Cao34). García et al. reported that serum concentrations of vitamin C were negatively associated with BMI and waist-to-height ratio(Reference García, Ronquillo and Caamaño Mdel35). Several studies have also found that serum magnesium was lower in obese or overweight children(Reference Hassan, Ahmed and Nasrullah36–Reference Celik, Andiran and Yilmaz39), adolescents(Reference Suliburska, Cofta and Gajewska40) and women(Reference Laires, Moreira and Monteiro41). Other studies have shown varying levels of micronutrient deficiency among obese individuals concerning different micronutrients(Reference McKay, Ho and Jane14–Reference Al-Delaimy, van Kappel and Ferrari19). However, relatively few studies have examined micronutrient intakes among overweight or obese individuals. For example, one study assessed correlations between BMI and dietary intakes of micronutrients and found no linear correlation between BMI and intake of micronutrients among both men and women(Reference McKay, Ho and Jane14), which contrasts with our findings. Another study found that obese individuals may develop hypoferremia due to inadequate iron intake relative to their body weight(Reference Yanoff, Menzie and Denkinger31), which contradicts our findings in men, where we found that obese men had a higher chance of adhering to the DRIs for iron. A recent study that used data from the US National Health and Nutrition Examination Survey found that vitamins A, B1, B2, B12 and D were negatively associated with the risk of obesity. Furthermore, when the concentrations of all nine vitamins (A, B1, B2, B6, B12, C, D, E and K) were at or above the 55th percentile, the combined intake of them might reduce the risk of obesity in both children and adolescents compared with the median values(Reference Tang, Zhan and Wei20). Studies on the associations between magnesium intake and obesity have been inconsistent. A cohort study of American young adults found a negative correlation between magnesium intake and obesity incidence(Reference Lu, Chen and Yang42). Another study using data from the National Health and Nutrition Examination Survey also found that magnesium intake was negatively correlated with BMI and WC(Reference Jiang, Ma and Li43). In contrast, another study found no association in magnesium intake between obese women and healthy controls(Reference Morais, de Freitas and Severo44), which contrasts with our findings. However, as we have mentioned, although previous studies have found negative associations between certain micronutrient intake and obesity, it does not necessarily mean that micronutrient deficiency is more prevalent among obese individuals. Our study provides further evidence that obese women have insufficient intakes of vitamins A, C and magnesium according to the official DRIs.
Our findings indicate that obese men and women exhibit different patterns of DRI adherence, although the underlying reason is not clear. It is possible that men and women have distinct dietary choices, as suggested by previous studies(Reference Vitale, Masulli and Cocozza45,Reference Beardsworth, Bryman and Keil46) . For instance, one study found that women were more likely to consume legumes, vegetables, fruits, eggs, milk, vegetable oils and added sugar. In contrast, men may consume more starchy foods, soft drinks and alcoholic beverages(Reference Vitale, Masulli and Cocozza45). Our study further demonstrates that obesity status may also impact the dietary choices of men and women, resulting in varying patterns of micronutrient intake. Thus, when conducting dietary intervention trials, obesity status should be considered.
Our study has both strengths and limitations. The strengths of the study include a fair sample size to assess the potential association between obesity and the chance of adherence to the DRIs. Furthermore, the population-based design allows for generalisation of our findings to the public. However, the study also has limitations. Firstly, the cross-sectional design does not allow for establishing causality. Secondly, we only had a one-time dietary assessment, which may introduce misclassification of nutrient intakes. Non-differential misclassification might favour the null hypothesis. However, the NAHSIT performed repeated surveys to adjust the 24 h recall data and minimise potential bias. Thirdly, we did not examine the associations of blood or urinary biomarkers of nutrients with obesity status. One reason for this is that the concentrations of nutrient biomarkers are affected not only by the individual's intake of nutrients but also by their absorption, distribution, metabolism or excretion of micronutrients. An association found between concentrations of certain nutrient biomarkers and obesity might not allow for any conclusion due to the complicated mechanisms. Additionally, many studies have already examined the serum concentrations of nutrient biomarkers among obese individuals, while studies on the role of dietary intake remain limited. We believe that our study contributes to filling this knowledge gap.
In conclusion, our study found that Taiwanese women with overweight or obesity may experience insufficient intake of some micronutrients. Further prospective studies are needed to confirm our findings. Moreover, future research could examine the intakes of both micronutrients and nutrient biomarkers simultaneously among overweight or obese individuals.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/jns.2023.31.
Acknowledgements
M.-C. L. was supported by the National Science and Technology Council, Taiwan (NSTC 111-2410-H-003-100-SSS), the Ministry of Science and Technology, Taiwan (MOST 110-2314-B-003-001) and the China Medical University, Taiwan (CMU108-N-12).
All authors significantly contributed to the manuscript. M.-C. L. contributed to the design of the study, was responsible for the management and retrieval of data, contributed to initial data analysis and interpretation. S.-P. L., H.-Y. F. and M.-C. L. drafted the manuscript. S.-P. L., H.-Y. F. and M.-C. L. contributed to interpreting results, critically reviewed the manuscript. S.-P. L., H.-Y. F. and M.-C. L. reviewed and approved the final manuscript.
The authors declare that they have no conflicts of interest.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the China Medical University & Hospital Research Ethics Center (CRREC-108-136). Written informed consent was obtained from all subjects.





