Introduction
The worldwide burden of cancer disease is projected to increase to 28.4 million new cancer cases by the year 2040, representing a 47% increase from the 19.3 million recorded in 2020 (Sung et al. Reference Sung, Ferlay and Siegel2021). The escalation is mainly due to the increasing aging population and cancer risk factors that are present in low, middle, and high human development index (HDI) countries (Sung et al. Reference Sung, Ferlay and Siegel2021). The projected increase in cancer burden is likely to have a more severe impact in countries with health-care systems with less established cancer care services. Escalation in cancer disease burden leads to increased demands on cancer health-care services and family resources (Yun et al. Reference Yun, Rhee and Kang2005; Zafa et al. Reference Zafa, Siddiqui and Channa2019).
In the cancer care system and disease trajectory, the only resource that is constantly utilized from the time of diagnosis to remission, or death, is the family caregivers (FCGs). The FCGs play a central role in cancer care, and unlike the other personnel involved in caring for cancer patients, FCGs perform their roles without any prior training or formal support. Consequently, the FCGs get heavily burdened with caregiving responsibilities, while at the same time continuing to provide physical, emotional, and practical support to cancer patients (Thomas et al. Reference Thomas, Campbell and Lee2021).
In many countries where the cancer burden is high and projected to increase, the health-care systems provide no formal programs to support the FCGs or to evaluate their needs or quality of life (QoL). The lack of such efforts is troubling, considering the upward trends of cancer disease, and findings showing that unmet physical and psychological needs have a high impact on the FCG’ QoL (Cochrane et al. Reference Cochrane, Woods and Dunne2022). The current study was conducted in Oman, a high HDI country, with increased cancer incidence and a health-care system in the process of establishing cancer care services (Al-Lawati et al. Reference Al-Lawati, Al-Bahrani and Al-Raisi2019).
There are no prior studies about the QoL of FCGs of adult cancer patients in Oman. The country (Oman) has a population of approximately 5.46 million people, and the age-adjusted annual incidence of cancer ranges from 70 to 110 per 100,000 (Mehdi et al. Reference Mehdi, Al Farsi, Al Bahrani, Al-Shamsi, Abu-Gheida and Iqbal2022). The upward trends in cancer incidence are expected to continue due to an aging population (Al-Lawati et al. Reference Al-Lawati, Al-Bahrani and Al-Raisi2019). In response to the cancer trends, the country has expanded its cancer services by opening a new cancer treatment center in the capital city, with services that primarily focus on diagnostics, therapeutics, and research (Al Farai et al. Reference Al Farai, Al Moundhri and Panaro2022). The country has clinics for cancer survivors and plans to establish programs focusing on home health, caregiver education, and supportive care (Mehdi et al. Reference Mehdi, Al Farsi, Al Bahrani, Al-Shamsi, Abu-Gheida and Iqbal2022). There was no active home health or supportive care program for FCGs in Oman at the time of this study.
In Oman, all citizens have access to free cancer care services provided by the public health-care system, but the increasing number of cancer patients is escalating the costs associated with this type of health care (Mehdi et al. Reference Mehdi, Al Farsi, Al Bahrani, Al-Shamsi, Abu-Gheida and Iqbal2022). The economic pressures have propelled the country to embark on strategies that ensure cost-effective care and prompt management of cancer and equitable resource allocation (Mehdi et al. Reference Mehdi, Al Farsi, Al Bahrani, Al-Shamsi, Abu-Gheida and Iqbal2022). Some of the strategies that have been emphasized include cancer prevention, screening, genetic screening, and increasing the number of patients who receive cancer care in outpatient units (Mehdi et al. Reference Mehdi, Al Farsi, Al Bahrani, Al-Shamsi, Abu-Gheida and Iqbal2022).
The shift from inpatient to majority outpatient cancer care has shifted more burden related to cancer patient care to the family and FCGs. In Oman, the caregiving burden among FCGs is not well known, but studies conducted in other countries in the middle east show that the health-care systems in the region pay suboptimal emphasis on supportive care for cancer patients (Keefe et al. Reference Keefe, Al Garni and Villalon2016). Supportive care in cancer includes the management of physical and psychological symptoms and side effects from diagnosis through treatment to posttreatment care, and this care helps to curtail some of the challenges faced by FCGs (Keefe et al. Reference Keefe, Al Garni and Villalon2016). Some FCGs of cancer patients in this region have been reported to face more challenges in the caregiving role due to their spirituality (Nemati et al. Reference Nemati, Rassouli and Ilkhani2017; Nikseresht et al. Reference Nikseresht, Rassouli and Torabi2016). A study conducted in Iran showed that FCGs of cancer patients tend to have a spiritual crisis and suffer spiritual distress due to beliefs that cancer disease happens as a way for the patient to compensate for past deeds and behaviors, experience disappointments, and feel deprived of divine attention (Nemati et al. Reference Nemati, Rassouli and Ilkhani2017). Islamic culture and religious beliefs are predominant in both Iran and Oman.
In Oman, a recent study showed that cancer patients reported that they received low- to moderate-quality oncology nursing care, especially in the domain of religious and spiritual care (Sharour et al. Reference Sharour, Al Sabei and Al Harrasi2022). Available literature also shows that FCGs of cancer patients in Oman are exposed to risks associated with oral anticancer agents since a large number are involved in administering the medication at home, but 42% forget to wash their hands with soap after administering oral chemotherapy (Hassan et al. Reference Hassan, Al-Marzooq and Al-Habsi2021). The reports of low-quality oncology nursing care and unsafe practices among FCGs may be indicators of suboptimal support for cancer patients and their FCGs. Inadequate support for cancer patients and their FCGs may escalate the caregiving burden, and patient’s symptoms, and can lead to a negative impact on the caregiver’s QoL. This study aimed to explore the determinants of QoL among Omani FCGs of adult patients with cancer pain.
Methods
Participants
A descriptive cross-sectional design was used to collect data from a sample of 165 FCGs (see Figure 1) and their adult patients with cancer and receiving care at the National Oncology Centre (NOC) in Oman. There were no prior studies conducted in Oman among FCGs of adult cancer patients that could be used to estimate the effect size. To reliably explore the predictors of QoL, the F-test for multiple regression was planned and the level of significance was set at 0.05. Using settings of a minimum power of 0.80, a minimum effect size of 0.2, 10 potential predictors, and an acceptable type 1 error with an alpha of 0.05, the G-power software estimated the required minimum sample to be 114.
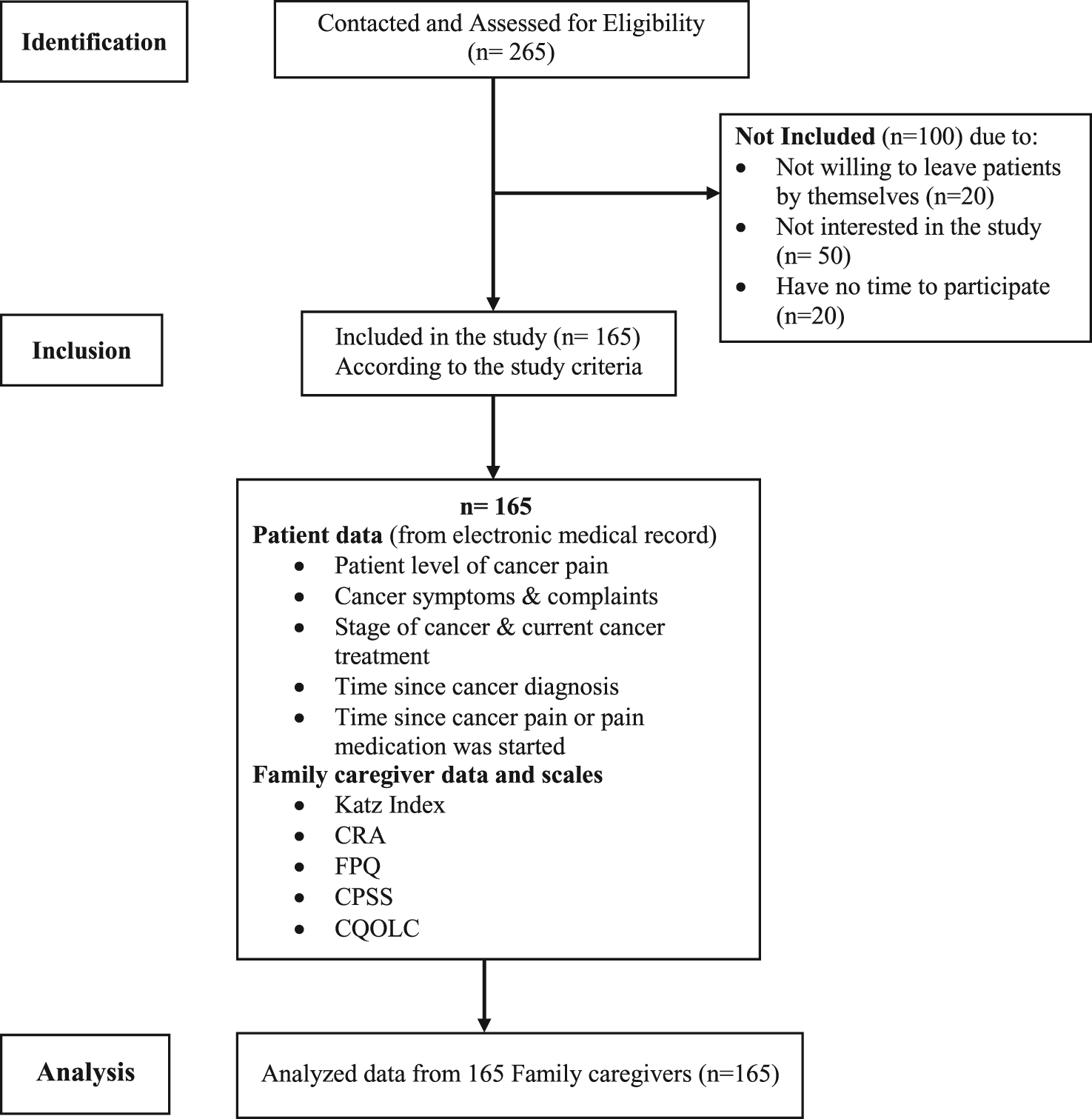
Fig. 1. Flow chart for inclusion and exclusion of participants.
The patients were individuals of age ≥18 years with a confirmed diagnosis of cancer (any type of cancer), receiving treatment for cancer pain, and in a condition stable enough to give consent for the study. The FCGs were individuals responsible for providing regular care and assistance to the patient during medical appointments, personal care, pain and related symptom management, and other activities when the patient is at home or in the hospital. The FCG was identified by the patient as the primary caregiver at home and had to be of age ≥18 years, able to speak English or Arabic, and have been in the caregiver role for at least 1 month. Individuals hired to help the family with caregiving responsibilities were excluded. The patient and FCGs were recruited consecutively through the different units of the NOC (the center receives patients from all regions of Oman).
Procedures
The study was approved by the Research and Ethics Committee of the university and the hospital system responsible for the NOC. The research assistants (RAs) identified eligible participants with the assistance of the nursing staff of the NOC. The participants were approached when they came seeking health care or follow-up care at the NOC. The RAs (all registered nurses) requested each patient to identify their primary caregiver. Written consent was obtained from the patients and their caregiver before data collection. A total of 265 eligible patients and their FCGs were approached and 165 (62.3%) agreed to participate (see Figure 1).
Variables and measures
A patient data sheet and the interview questionnaire (IQ) were used for data collection. The patient data sheet was used to collect data about the patient’s current level of pain, cancer-related symptoms and complaints present when the patient is at home, stage of cancer when it was first diagnosed, current cancer treatment, time since the cancer was first diagnosed, and length of time since cancer pain started or pain medication was started. The above data was obtained from the patient’s electronic medical record (the patient’s electronic medical record is updated during each patient visit).
The IQ was used to collect data from FCGs and comprised the patient’s and FCGs’ demographic characteristics, the Katz index (Katz et al. Reference Katz, Down and Cash1970), the Caregiver Reaction Assessment (CRA) (Given et al. Reference Given, Given and Stommel1992), the Family Pain Questionnaire (FPQ) (Ferrell et al. Reference Ferrell, Rhinner and Rivera1993), the modified caregiver cancer pain and other symptom management self-efficacy scale (CPSS) (Anderson et al. Reference Anderson, Dowds and Pelletz1995), one-item measuring the FCGs’ self-rated health, and the Caregiver Quality of Life Index–Cancer Scale–Persian Version (CQOLC) (Khanjari et al. Reference Khanjari, Oskouie and Langius-eklöf2011).
The Katz index (6 items) measures patients’ functional status by assessing their ability to independently perform the activities of daily living (Katz et al. Reference Katz, Down and Cash1970). The CRA has a subscale (5 items) that measures the impact of caregiving on physical health status (Given et al. Reference Given, Given and Stommel1992). The CRA subscale was used to measure the impact of caregiving on the FCGs’ physical health. A high total score on the Katz index and CRA indicates a high functional status and a greater impact of caregiving on physical health, respectively. The Cronbach’s alpha of the Katz index and CRA in the current study were 0.92 and 0.72, respectively.
The FCGs’ current self-rated health was measured using an item anchored on 2 extreme values of 1 to 10 (“1 = very healthy” to “10 = very ill”) assessing current health as compared to health at the same time in the past year. A score of 6 or higher indicates distressed health status. The FCGs also responded to 3 items measuring the level of distress caused by cancer pain to the patient (on a scale of “0 = no distress” to “10 = a great deal of distress”), the level of distress caused by the patient’s pain to the FCG (on a scale of “0 = no distress” to “10 = great deal of distress”), and the FCG’s confidence in their ability to control patient’s pain (on a scale of “0 = no confidence at all” to “10 = great deal of confidence”).
The knowledge subscale of the FPQ was used to measure the FCGs’ knowledge about cancer pain management (Ferrell et al. Reference Ferrell, Rhinner and Rivera1993). The FCGs’ responses are recorded using a 10-point scale with “0” as the most positive outcome and “10” as the most negative outcome (extent of agreement or disagreement with a given statement). The total scores (10 items) range from 0 to 100. The CSPP (16 items) was used to rate the FCGs’ self-efficacy to support patients and manage their cancer pain and cancer symptoms (Anderson et al. Reference Anderson, Dowds and Pelletz1995; Campbell et al. Reference Campbell, Keefe and McKee2004; Porter et al. Reference Porter, Keefe and Garst2008). The participants’ responses were recorded using a 10-point Likert scale (10 = “very uncertain” and 100 = “very certain”). High total scores indicate a greater self-efficacy for pain and related symptom management. In the current study, Cronbach’s alpha of the CPSS and FPQ were 0.93 and 0.50, respectively.
The CQOLC was used to assess the QoL of FCGs (Khanjari et al. Reference Khanjari, Oskouie and Langius-eklöf2011; Weitzner et al. Reference Weitzner, Meyers and Steinbruecker1997). The CQOLC (35 items) has 4 subscales of mental/emotional burden (14 items), lifestyle disruption (9 items), positive adaptation (8 items), and financial concern (3 items) and 1 item about the family interest that is not part of any subscale (Khanjari et al. Reference Khanjari, Oskouie and Langius-eklöf2011). The responses were recorded using a 5-point Likert scale ranging from 0 (not at all) to 4 (very much), and high total scores reflect better QoL (range from 0 to 140). The Cronbach’s alpha of the CQOLC was 0.82 in the current study.
Analysis
Data were analyzed using the Statistical Package for Social Sciences software version 23 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to describe the sample, FCGs’ knowledge, self-efficacy, physical well-being, and the caregivers’ QoL. The Shapiro–Wilk test confirmed that overall CQOLC scores were normally distributed. The mean score of the CQOLC and its domains was used as a cutoff point to form a binary outcome. The chi-square test and t-test were used to examine the factors associated with overall QoL and the 4 domains of QoL. Linear regression analysis was used to examine the predictors of QoL. The level of significance was set at p ≤ 0.05.
Results
Participants
The results presented in Table 1 show that most of the FCGs were female (58.2%), married (64.2%), and a child of the cancer patient (53.9%). The caregiving role was almost a full-time job (36.36 ± 92.23 hours per week), and on average, the FCGs had been in this situation for 11.16 ± 11.03 months. Most of the FCGs had high self-rated health (94.5%) but a large number (41.2%) reported a high impact of caregiving on their physical health. The FCGs with overall low QoL reported significantly lower mean self-rated health (p = 0.002) and a significantly higher mean impact of caregiving on physical health (p = 0.011).
Table 1. Characteristics of family caregivers
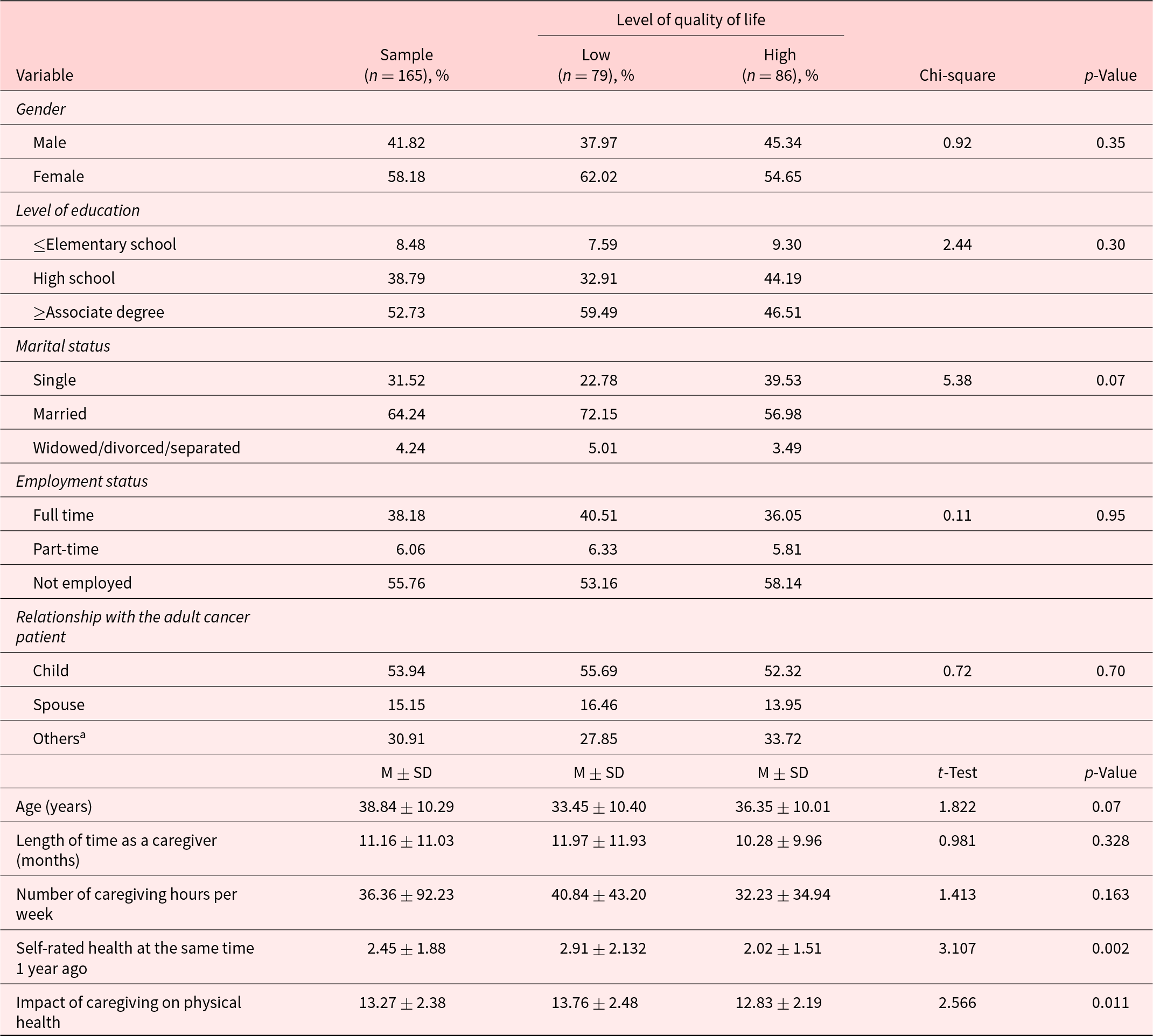
M, mean; and SD, standard deviation.
a Includes neighbor, mother, in-law, friend, grandchild, and niece.
The cancer patients were mostly female (75.2%), diagnosed with stage 3 or 4 cancer (58.79%), and on chemotherapy (57.6%) (see Table 2). The majority of patients reported having intermittent pain (83%), and the pain was rated as severe (50.9%) (Table 3). A significantly higher number of FCGs with low QoL were taking care of a patient with severe cancer pain (55.7%) compared to FCGs with high QoL (46.5%) (p = 0.040). Additionally, FCGs with low QoL were taking care of patients with lower functional status (4.64 ± 2.14) compared to FCGs with a high QoL (5.51 ± 1.36) (p = 0.002).
Table 2. Characteristics of cancer patients
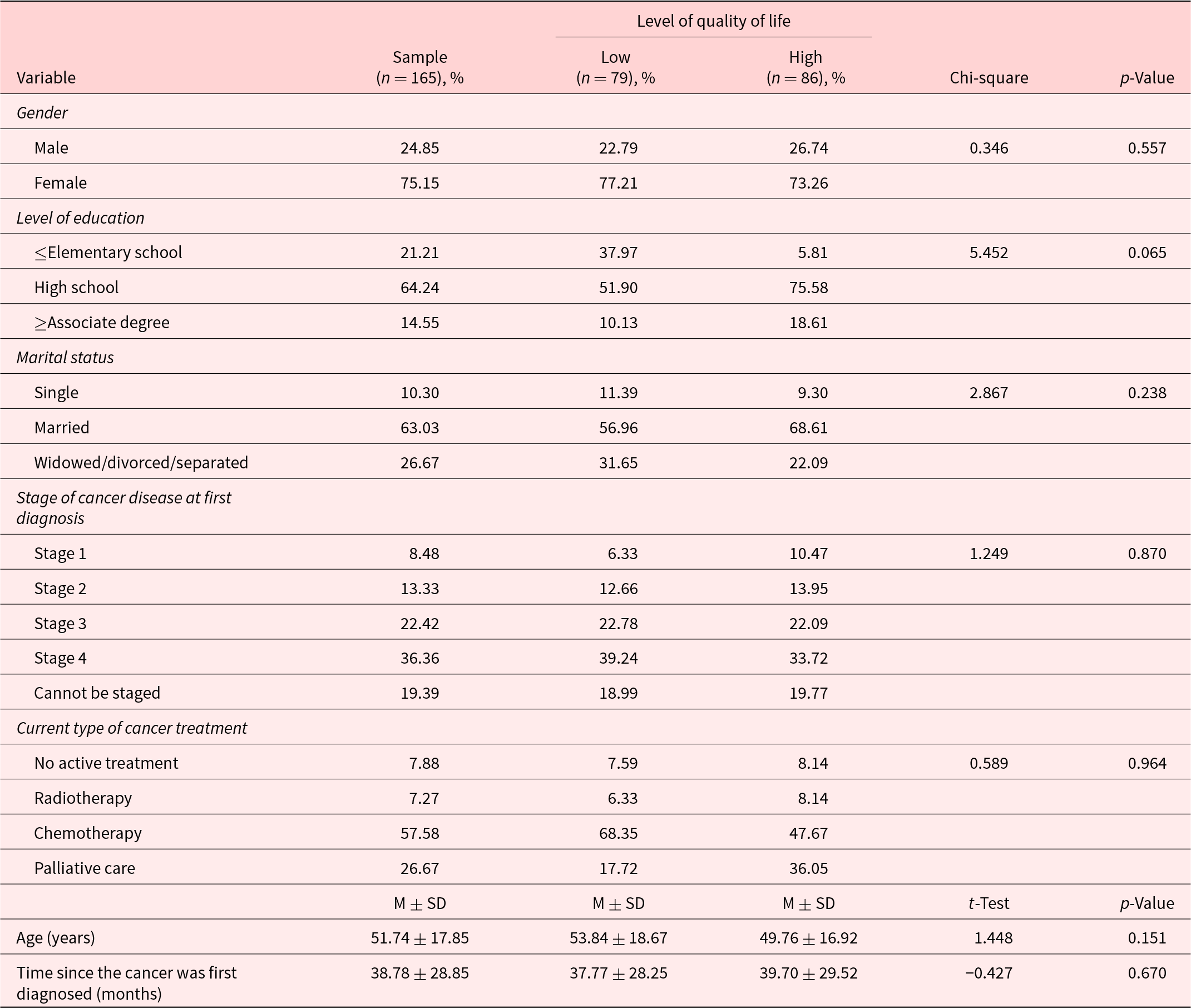
M, mean; and SD, standard deviation.
Table 3. Patients’ cancer pain and functional status
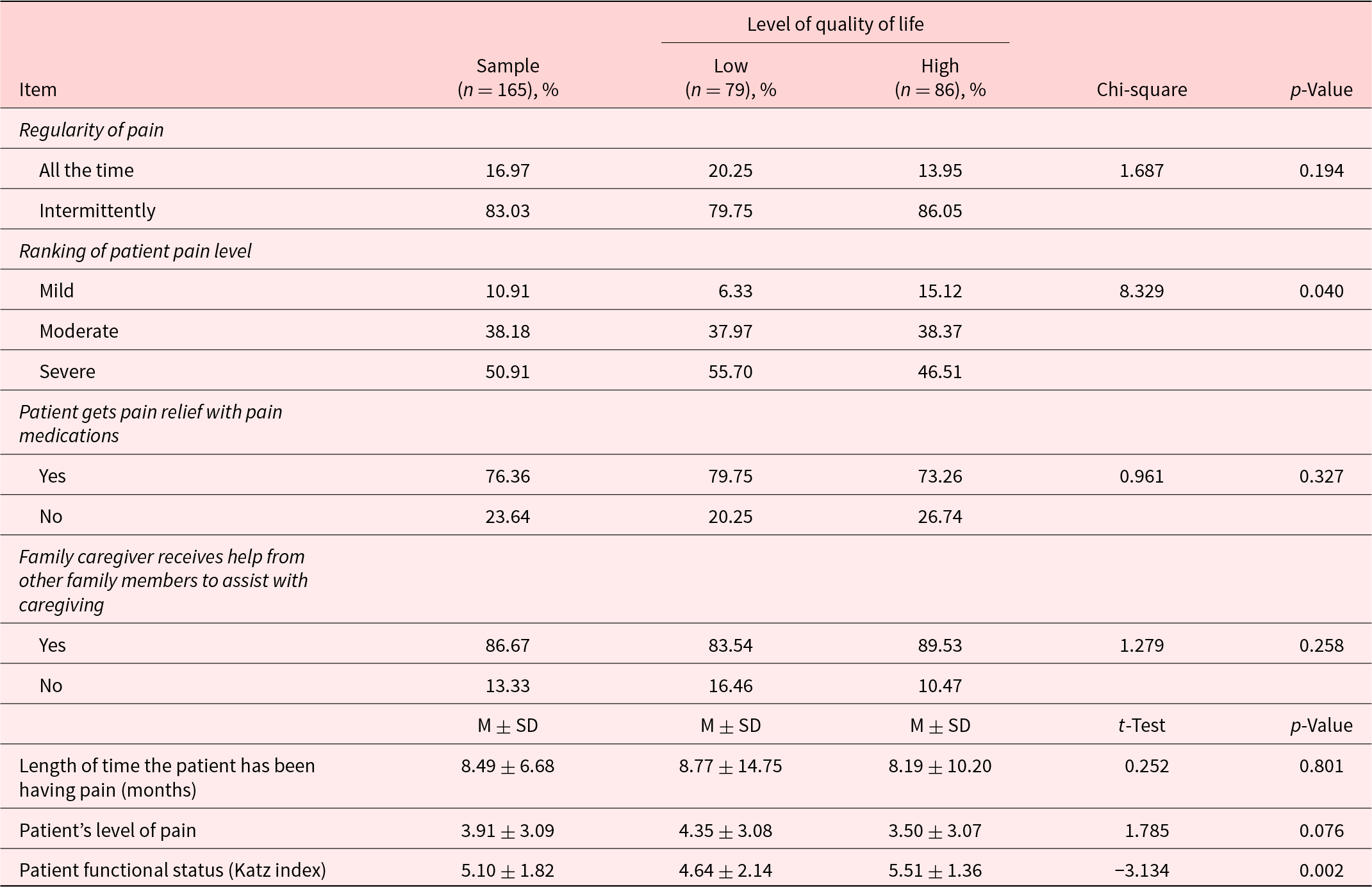
M, mean; and SD, standard deviation.
Knowledge about cancer pain and self-efficacy for cancer pain and symptom management
The FCGs’ mean score for knowledge about cancer pain management (46.21 ± 14.91) was equivalent to moderate knowledge score (see Table 4). There were no significant differences in knowledge scores between FCGs with low and high QoL. The mean CPSS score shows that the FCGs had moderate self-efficacy (892.9 ± 296.20). The FCGs with a high QoL had significantly higher self-efficacy compared to those with a low QoL (p = 0.009). All the FCGs reported that cancer pain was distressing to them (mean = 6.85 ± 3.29) and the patients (mean = 6.74 ± 3.11). The reported level of distress due to cancer pain was significantly higher among FCGs with low QoL (p = 0.000) and patients who were cared for by FCGs with low QoL (p = 0.013). On the other hand, FCGs with a higher QoL were significantly more confident in their ability to control the patient’s pain when compared to those with a low QoL (p = 0.013).
Table 4. Caregivers’ knowledge and self-efficacy in cancer pain and symptom management
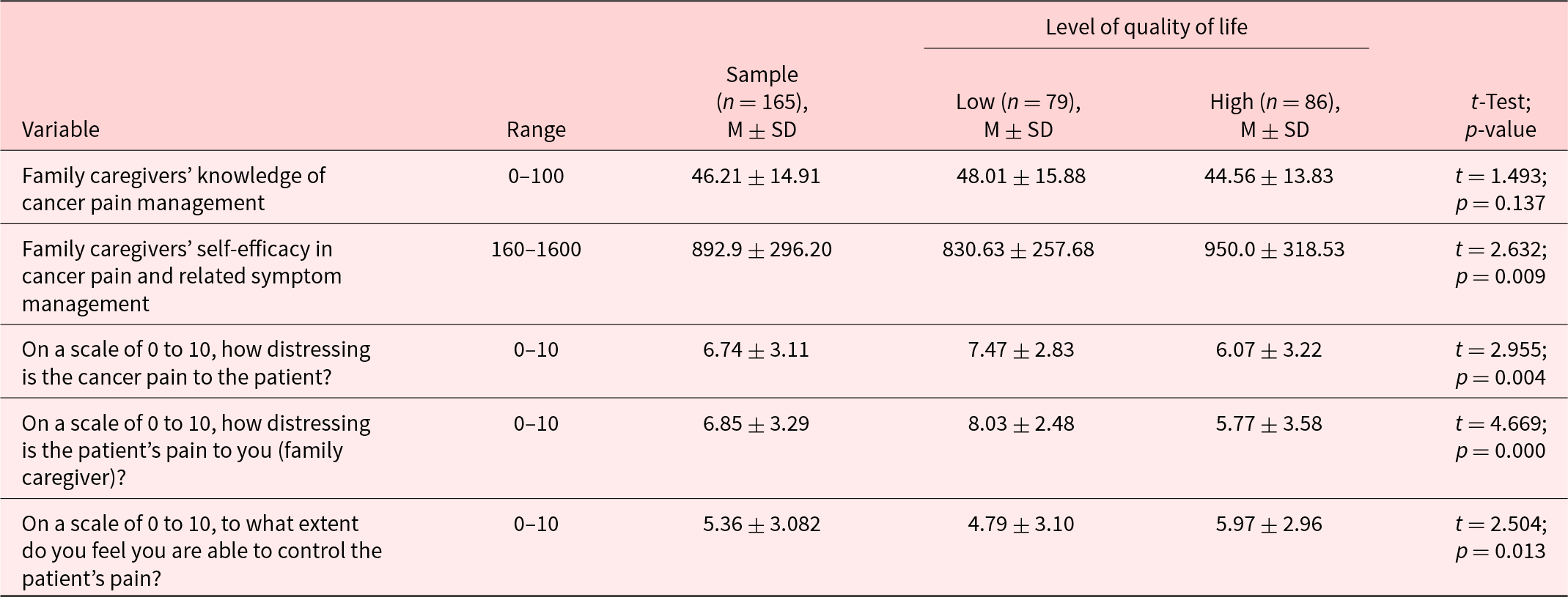
M, mean; and SD, standard deviation.
Family caregiver’s quality of life
The results presented in Table 5 show an almost even split between the number of FCGs found to have low (48%) and high (52%) QoL. However, overall the FCGs had a low QoL (58.44 ± 17.95). The majority of FCGs reported having a high QoL in the domains of mental/emotional burden (57.6%) and financial strain (67.9%). The domain of QoL in which the majority of FCGs had low QoL scores was support and positive adaptation (55.2%).
Table 5. Family caregivers’ quality of life
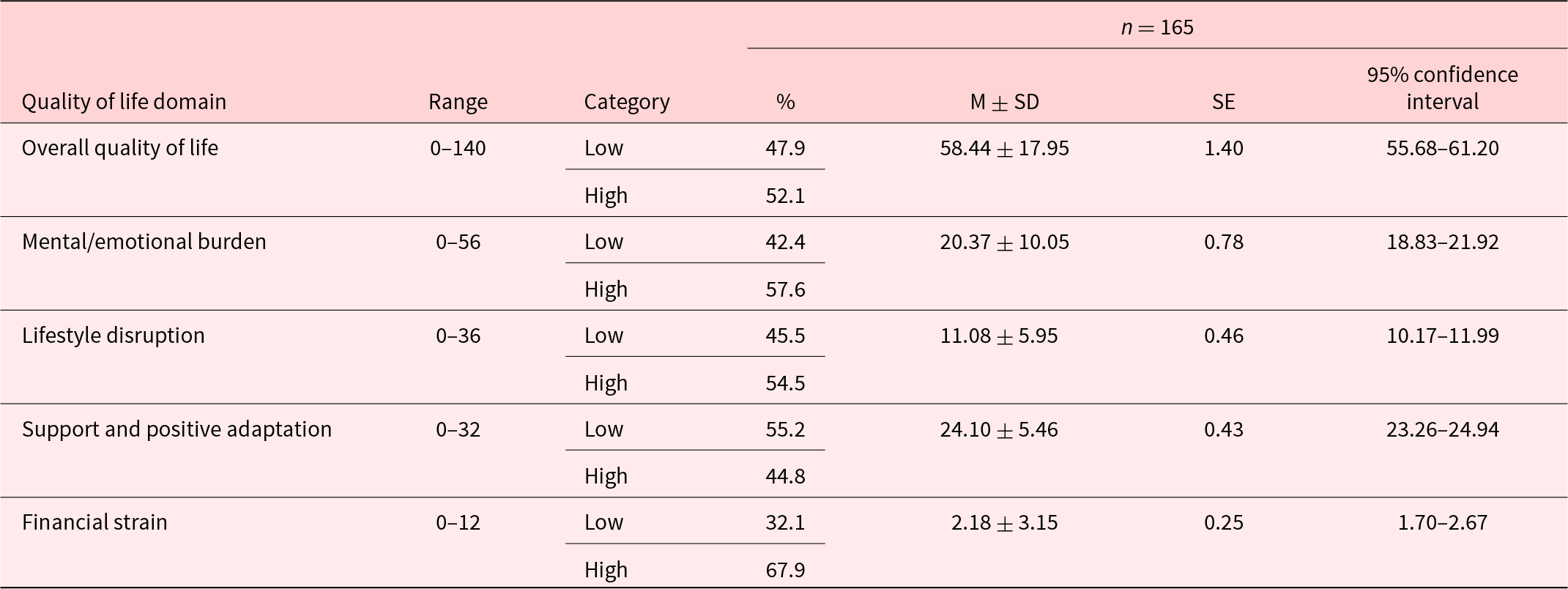
M, mean; SD, standard deviation; and SE, standard error.
Predictors of family caregivers’ quality of life
The regression analysis (see Table 6) shows that the level of distress faced by FCGs due to the patient’s pain (p < 0.01), patient’s functional status (p < 0.01), and the FCGs’ perceived impact of caregiving on their health (p < 0.05) were significant predictors of overall QoL and accounted for 23.1% of the variance in the overall QoL (p < 0.01). The significant predictors of mental and emotional burden were the level of distress faced by FCGs due to the patient’s pain (p < 0.01), patient’s functional status (p < 0.01), the perceived impact of caregiving on the FCGs’ health (p < 0.05), and self-efficacy (p < 0.05), and these 4 factors were responsible for 26.1% of the variance in this domain (p < 0.01).
Table 6. Predictor of family caregivers’ quality of life
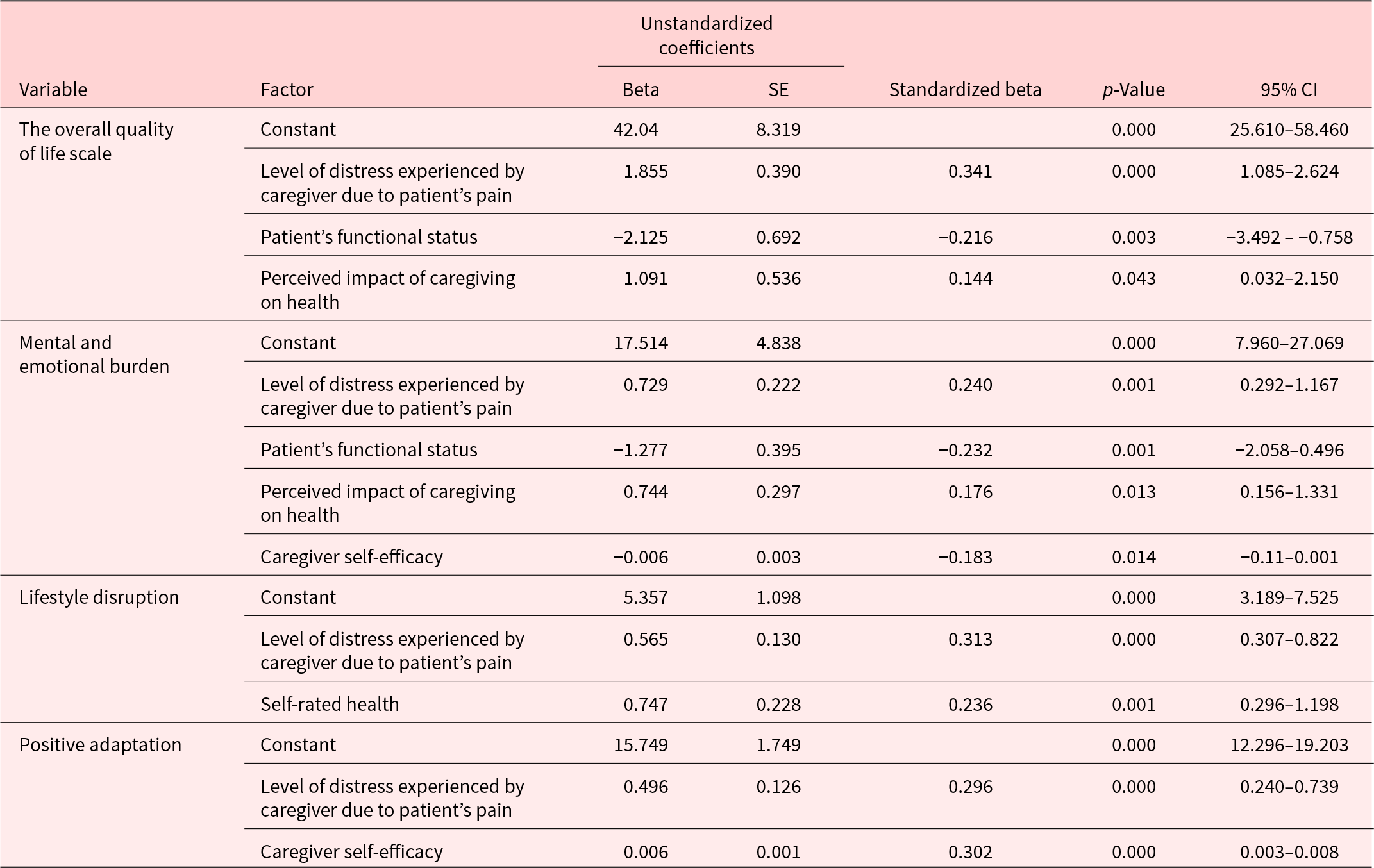
SE, standard error; and CI, confidence interval.
The predictors of lifestyle disruption were the level of distress faced by FCGs due to patient’s pain (p < 0.01) and self-rated health (p < 0.01), and these 2 factors accounted for 16.7% of the variance in lifestyle disruption (p < 0.01). The predictors of positive adaptation were the level of distress faced by FCGs due to the patient’s pain (p < 0.01) and self-efficacy (p < 0.01), and both these factors were responsible for 13.1% of the variance in positive adaptation (p < 0.01). There was no significant relationship between financial strain and any of the factors examined.
Discussion
To our knowledge, this is the first study to explore the QoL of FCGs of adult patients with cancer pain in Oman. The other 2 studies that involved caregivers in Oman focused on FCGs of children with cancer and their unmet needs and caregiving burden (Al-Dhawyani et al. Reference Al-Dhawyani, Al-Hinai and Chan2022; Chan et al. Reference Chan, Al‐Dhawyani and Al Hinai2022). The results of the current study show that FCGs in Oman have low QoL (58.44 ± 17.95) and a large number (48%) had very low QoL. There were no studies conducted in Oman and nearby countries that could be used for comparison, but the findings of low QoL (using the CQOLC) have also been reported among FCGs in the Netherlands (mean = 49.4 ± 20.04) (Decadt et al. Reference Decadt, Laenen and Celus2021).
Studies measuring FCGs’ QoL using the CQOLC conducted in Singapore (mean = 86.5 ± 24.1), Canada (mean = 82.1 ± 20), Malaysia (mean = 80.17), and Uganda (mean = 70.2 ± 20.3) found higher levels of QoL than ours (Abdullah et al. Reference Abdullah, Idris and Shamsuddin2019; Duimering et al. Reference Duimering, Turner and Chu2020; Kizza and Muliira Reference Kizza and Muliira2020; Leow et al. Reference Leow, Chan and Chan2014). Unlike in Oman, cancer patients in the above-highlighted countries have access to established palliative care programs. The studies conducted in Singapore, Canada, and Uganda included a large number of FCGs caring for adult cancer patients receiving some form of palliative care services.
Similar to other studies, the caregivers’ QoL was most negatively impacted in the domains of support and adaptation (Ochoa et al. Reference Ochoa, Lunsford and Smith2020). This finding confirms that access to supportive care is essential for the well-being of FCGs of adult cancer patients. The findings of a high negative impact on support and positive adaptation have also been reported in Uganda and Malaysia (Abdullah et al. Reference Abdullah, Idris and Shamsuddin2019; Kizza and Muliira Reference Kizza and Muliira2020). On the contrary, a study involving Turkish FCGs of cancer patients found that psychological health, spiritual health, and physical health were the most negatively impacted domains (Üzar-Özçetin and Dursun Reference Üzar-Özçetin and Dursun2020). While in Saudi Arabia, a study of QoL among FCGs of cancer patients (Short-Form Health Survey SF-36) found high scores of QoL and better functioning in the domains of physical functioning, role functioning, and emotional well-being, but moderate to low in the domains of energy/fatigue and general health (Almutairi et al. Reference Almutairi, Alodhayani and Alonazi2017).
The majority of FCGs in the current study had high QoL scores in the domains of mental/emotional burden and financial strain. This finding is not surprising considering Oman’s extended family traditions and culture, high HDI status, and access to free cancer care services provided by the public health-care system (Mehdi et al. Reference Mehdi, Al Farsi, Al Bahrani, Al-Shamsi, Abu-Gheida and Iqbal2022). In Oman, the family members are highly involved in patient care and many times take up full control of the treatment decision-making for the cancer patient because social norms expect the acquisition of these duties when a family member is in poor health (Al‐Bahri et al. Reference Al‐Bahri, Al‐Moundhri and Al‐Mandhari2018). A recent study of Omani cancer patients and their FCGs showed that a large number have positive and supportive attitudes toward cancer patients and only feel social obstacles when planning for the marriage of a person with a history of cancer diagnosis (Al-Azri et al. Reference Al-Azri, Al-Hattali and Al-Ghafri2021).
Overall, the FCGs in our study had moderate knowledge about cancer pain (46.21 ± 14.91) and moderate self-efficacy in cancer pain and related symptom management (892.9 ± 296.20), but this may be suboptimal since a large number were taking care of a patient with severe cancer pain (50.9%). Additionally, FCGs with low QoL reported lower mean self-rated health, lower mean self-efficacy, and less confidence in their ability to control the patient’s cancer pain. The FCGs with low QoL also tended to be those caring for a patient with severe cancer pain and low functional status and reported higher levels of distress due to the patient’s cancer pain and a high impact of caregiving on their physical health. The above findings suggest that the caregivers’ QoL is affected by the patient’s cancer pain, the patient’s functional status, and the caregivers’ self-efficacy for cancer pain and related symptom management.
This study shows that the modifiable predictors of FCGs’ overall QoL were the level of distress faced by FCGs due to the patient’s cancer pain (p < 0.01), patient’s functional status (p < 0.01), and perceived impact of caregiving on FCGs’ health (p < 0.05). Other studies show that taking care of patients in active cancer treatment, a spouse/partner relationship with the caregiver, living with the patient (Decadt et al. Reference Decadt, Laenen and Celus2021), knowledge about cancer pain management, and self-efficacy for pain management are significant predictors of caregivers’ overall QoL (Kizza and Muliira Reference Kizza and Muliira2020).
The other factors associated with the different domains of QoL such as the FCGs’ self-efficacy in cancer pain and related symptom management and caregiver self-rated health are similar to what has been reported in other studies. For instance, a longitudinal study showed that distress in spousal caregivers is associated with a high level of distress among cancer survivors (Milbury et al. Reference Milbury, Badr and Fossella2013), and high scores in QoL aspects such as bodily pain, vitality, social activities, and mental health are associated with spiritual well-being (Spatuzzi et al. Reference Spatuzzi, Giulietti and Ricciuti2019). A study of FCGs of patients with advanced cancer and receiving home hospice in Singapore found that the main predictors of QoL improvement were caregivers’ satisfaction with social support, religiosity, and changes in the patient’s condition (Leow et al. Reference Leow, Chan and Chan2014). It is also important to note that a low QoL among cancer caregivers is associated with poor patient performance status and expression of interest in more support services (Duimering et al. Reference Duimering, Turner and Chu2020).
Overall, our study shows that a large number of Omani FCGs of adult patients with cancer pain have a low QoL. Understanding the intricacies of the QoL of FCGs of cancer patients and the associated factors in countries such as Oman with health-care systems that are still developing is essential because it directs us to critical interventions that can enhance the patient, caregiver, and health-care system outcomes. For instance, the association between the caregiver QoL and factors such as FCGs’ health status, FCGs’ self-efficacy for cancer symptom management, patient’s cancer pain, and patient’s functional status demonstrates that health promotion for FCGs, education, and training to enhance self-efficacy in pain and symptom management, and other caregiving skills, can positively augment outcomes of the clients and health-care system.
Therefore, a supportive care program that assesses, educates, empowers, and assists cancer patients and their caregivers can mitigate many of the negative outcomes of FCGs (Berry et al. Reference Berry, Dalwadi and Jacobson2017). Other studies have shown that the main caregiver-identified priorities in cancer care for their patients are those that focus on training the caregiver, the health and well-being of the caregiver, and policy reforms to address caregiver needs (Thomas et al. Reference Thomas, Campbell and Lee2021). The findings of our study support these priorities. Additionally, we recommend additional studies to develop and calibrate supportive care interventions focusing on health promotion for FCGs and strategies for equipping FGCs with knowledge and skills in cancer pain and symptom management while at home. The availability of such evidence-based interventions will enable countries with underdeveloped cancer care systems to address the existing and future caregiving-related outcomes despite the increasing cancer burden.
Strength and limitation
This study is the first to explore the QoL of FCGs of adult cancer patients in Oman. The study used standardized scales to measure the FCGs’ QoL, self-efficacy, and knowledge about cancer pain management at home, but has limitations that need to be considered before generalizing the findings to all FCGs in Oman. For instance, the used nonrandom sample and the reliability of the FPQ was low. The data were collected during the follow-up care visits or when seeking health care rather than in the home care setting, and this could have affected the FCGs’ perception of their QoL and other variables. Finally, psychological variables, such as depression and anxiety, were not evaluated in the present study but are critical markers of well-being and QoL. The adjusted R 2 values of the multivariate analyses were not particularly high, and this may indicate that there are other factors related to caregivers’ QoL.
Conclusion
Despite the increasing cancer burden in Oman, there were no baseline studies on the QoL and well-being of FCGs of adult patients with cancer pain. The current study highlights that FCGs of adult patients with cancer pain have low QoL, and some of the modifiable factors that are associated with this predicament include FCGs’ health status, FCGs’ self-efficacy for cancer pain and symptom management, patient’s functional status, and the impact of the patient’s cancer pain on the caregiver. Supportive care programs and interventions can help address these factors and subsequently enhance the caregivers’ QoL.
Conflicts of interest
The authors report no conflicts of interest.










