Introduction
Palliative care (PC) and advance care planning (ACP) have become increasingly prominent in health care globally due to high cancer estimates (Grant et al. Reference Grant, Back and Dettmar2021; Patel and Lyons Reference Patel and Lyons2020). Early discussions about ACP can provide individuals with opportunities to make important decisions about whether to receive PC in the future, especially for those living with cancer whose disease progression may affect their ability to make decisions (Lin et al. Reference Lin, Evans and Koffman2019). PC not only improves quality of life but also provides effective symptom control, increases patient and family satisfaction with care, reduces health-care costs, and promotes a less aggressive treatment approach (Kavalieratos et al. Reference Kavalieratos, Corbelli and Zhang2016; McDonald et al. Reference McDonald, Swami and Hannon2017; Temel et al. Reference Temel, Greer and Muzikansky2010; Zimmermann et al. Reference Zimmermann, Swami and Krzyzanowska2014). ACP is not just a formal documentation of a patient’s end-of-life treatment preferences but rather a means of facilitating communication between the patient, their family, and health-care providers. It explores the patient’s understanding of the disease and prognosis, clarifying treatment goals and assisting in decision-making (Matsuoka et al. Reference Matsuoka, Kunitomi and Nishizaki2018). Anticipating care needs enables effective interventions through education and longitudinal follow-up, preventing symptom flares, reducing hospitalizations, filling information gaps, and mitigating difficulties in the end-of-life process (Hui et al. Reference Hui, Hannon and Zimmermann2018; Patel and Lyons Reference Patel and Lyons2020).
Despite the potential benefits of PC, more than half of patients who would benefit from it do not receive PC, due to refusal (Bazargan and Bazargan-Hejazi Reference Bazargan and Bazargan-Hejazi2021; Huynh and Moore Reference Huynh and Moore2021). Moreover, discussions about ACP with patients diagnosed with cancer are not occurring, which further reduces the opportunity for patients to choose PC (Dinescu Reference Dinescu2021; Lin et al. Reference Lin, Evans and Koffman2019). The main barriers to these discussions are the lack of information about the potential benefits of PC, difficulties that health professionals face in openly discussing disease progression, and stigmas surrounding the term “palliative care” held by patients. Additionally, when there is a lack of trust in the doctor–patient relationship, engaging in meaningful dialogue about probable outcomes and patient preferences becomes a challenging task (Lin et al. Reference Lin, Evans and Koffman2019; Rugno et al. Reference Rugno, Paiva and Nunes2014; Santos Neto et al. Reference Santos Neto, Paiva and de Lima2021).
While alternative models of ACP have only recently started to emerge in Brazil, most of the discussions occur within structured PC services staffed by health-care professionals trained in this field. Unfortunately, the limited availability of PC services in the country leads to infrequent conversations about ACP. The deeply ingrained paternalistic health-care culture in Brazil presents a significant hurdle for ACP, as it diminishes patient autonomy, discourages active patient participation in health-care decisions, and can exacerbate health disparities (Tardelli et al. Reference Tardelli, Forte and Vidal2023).
Although there are barriers to referral and initiation of PC, adequate knowledge about PC and low levels of stigma can minimize them (Cai and Lalani Reference Cai and Lalani2022; Chen et al. Reference Chen, Kuo and Lin2022; Rugno et al. Reference Rugno, Paiva and Nunes2014; Santos Neto et al. Reference Santos Neto, Paiva and de Lima2021). As stigmas are reduced, discussions about ACP become possible. When these discussions lead to choices, they facilitate early PC integration. Encouraging conversations about what is a priority for patients in their current and future care not only identifies and removes stigmas but also increases treatment effectiveness, patient autonomy, and is essential to facilitate shared decision-making and problem-solving later on (Dias et al. Reference Dias, Bezerra and Barra2022). Therefore, there is a growing need to increase awareness and understanding of PC and ACP as key factors of public-health priority (McIlfatrick et al. Reference McIlfatrick, Slater and Beck2021; Whitelaw and Clark Reference Whitelaw and Clark2019).
Comprehension of the disease is a crucial aspect of patients’ overall health. Knowing the stage of cancer, treatment options, and possible adverse effects may empower patients to make decisions that align with their personal goals, preferences, and values (Johnson et al. Reference Johnson, Butow and Kerridge2018; Yoo et al. Reference Yoo, Lee and Kang2020). A previous study found that patients who had a good understanding of their incurable illness were associated with physician orders for life-sustaining treatment, preferences for ACP, less aggressive care, and were more likely to have discussed their care with their families (Yoo et al. Reference Yoo, Lee and Kang2020). However, oncologists and PC physicians still view patient autonomy as “freedom from interference.” They prioritize care, relationships, and a “good death” over autonomy and are hesitant to empower patients to comprehension and make decisions (Johnson et al. Reference Johnson, Butow and Kerridge2018).
Several studies have been conducted exploring interventions and strategies to improve cancer patients’ understanding of PC and ACP (Case et al. Reference Case, Epstein and Gustin2022; Malhotra and Ramakrishnan Reference Malhotra and Ramakrishnan2022). However, determining how and when patients want to learn about these topics may be an even more practical approach to fostering ACP engagement, shared decision-making, and early referral to PC. Therefore, this study aims to identify the characteristics of patients who are most likely to engage in discussions about PC and ACP, as well as to assess their preferences for the optimal timing and method of discussing these topics.
Methods
Study design
A 2-phase mixed-methods study was conducted combining the strengths of qualitative and quantitative methodologies to obtain deeper understanding and evaluated at 2 distinct moments: (1) Phase 1, in person, quantitative; (2) Phase 2, video call, qualitative.
In the first phase, evaluations were conducted in person using assessment tools to investigate sociodemographic and clinical characteristics, knowledge about PC and ACP, decision-making capacity, and levels of barriers and stigmas among the patients. At the end of these evaluations, the patients received a leaflet containing technical and illustrated information about PC and ACP (contents: What is ACP? Why is ACP important? Who is ACP for? Step-by-step of ACP; What are PC? Who are PC for? Why are PC important?). The purpose of this instructional material was to impart essential knowledge and minimize response bias related to the inquiry of “how” and “when.”
Between 7 and 14 days after the data collection, all patients who participated in the first phase were invited to participate in the qualitative interview via video call. The qualitative method followed the Consolidated Criteria for Qualitative Research Reports (Tong et al. Reference Tong, Sainsbury and Craig2007).
Participants
Women with breast cancer, aged between 18 and 75 years, with knowledge of the cancer diagnosis, in both outpatient or inpatient treatment settings, with Eastern Cooperative Oncologic Group Performance Status (ECOG-PS) ≤2, and ability to respond to the data collection were included in the study. Participants who presented difficulties in making online connections by video calls or any significant auditory, visual or verbal language deficit were excluded.
Data collection and analysis
Quantitative phase
The participants were recruited from the Women’s Outpatient Clinic and Chemotherapy Infusion Center, based on eligibility criteria. They completed sociodemographic and clinical questionnaires developed by the researchers, as well as a questionnaire assessing comprehension and decision-making capacity (CMDq-PC/ACP) (Trevizan et al. Reference Trevizan, Paiva and Julião2023), the Scale of Knowledge and Stigmas concerning PC (EsCE-CP19) (developed by the authors, manuscript under review), and 2 checklists assessing participants’ awareness about PC and ACP. After the data collection phase, patients were provided with an educational leaflet about PC and ACP, aimed at reducing potential biases in their responses to qualitative questions. At the end of Phase 1, patients were informed about the details of the second phase and were given the option to participate if they felt comfortable doing so. Participants were divided into 2 groups: those who participated in both phases of the study and those who participated in Phase 1 only (refused Phase 2). Exploratory quantitative data analysis was performed using IBM SPSS Statistics 23 software. Data with p-values <0.05 were considered statistically significant.
Qualitative phase
After 7 to 14 days, the patients who participated in the first survey (n = 115) were contacted to schedule their participation in the qualitative phase. Semi-structured interviews were conducted by the first author (FBT), a clinical psychologist with extensive experience and a master’s degree in health psychology. The patients (n = 61) completed the same questionnaires as in the first phase and then responded to 6 guiding questions: “Do you know what PC and ACP are?” “When is the most appropriate time to discuss PC and ACP?” and “What is the most appropriate way to discuss PC and ACP?”
The interviews were conducted exclusively via video call and were recorded, transcribed by an assistant researcher, and then deleted. Bardin’s discourse analysis method was used for qualitative data analysis (Bardin Reference Bardin2016). Content analysis was performed independently by the researchers FBT and LFdA. Subsequently, with the presence of another researcher (BSRP), peer review was performed until consensus was reached.
Results
In Phase 1, a total of 115 participants completed questionnaires related to PC and ACP. All participants who completed the first phase were invited to participate in the subsequent qualitative phase. Of them, only 53.04% (61 out of 115) completed both phases of the study, while the remaining 46.96% (n = 54) declined to participate in the second phase (Figure 1).
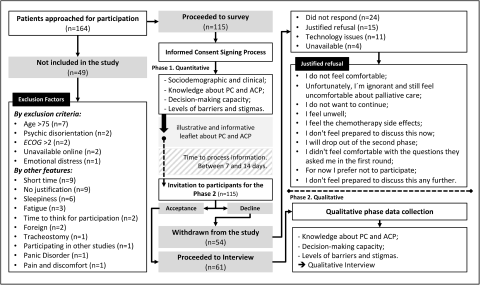
Figure 1. Flowchart of mixed-methods design representation and changes in the number of participants through the phases.
The sociodemographic and clinical characteristics of the participants are outlined in Table 1.
Table 1. Sociodemographic and clinical characterization compared patients who participated in the both study phases and who refused the second moment (only Phase 1)

SD = standard deviation; N = number of participants; inc. = incomplete; comp. = complete.
Statistical calculation:
a Mann–Whitney test.
b Pearson’s chi-squared test.
c Fisher’s exact test.
Participants who completed both phases were more frequently married (78.7% vs. 59.3%, p = 0.024), had higher educational levels (higher education: 34.4% vs. 18.5%, p = 0.027), and more years of schooling (more than 10 years: 80.3% vs. 53.7%, p = 0.012) in comparison with patients who refused Phase 2. On the other hand, patients who declined to participate in the second phase were more likely to have an advanced-stage cancer (45.9% vs. 77.8%, p = 0.001) and were receiving a systemic palliative treatment (59.0% vs. 79.6%, p = 0.049) compared with patients who participated in both phases.
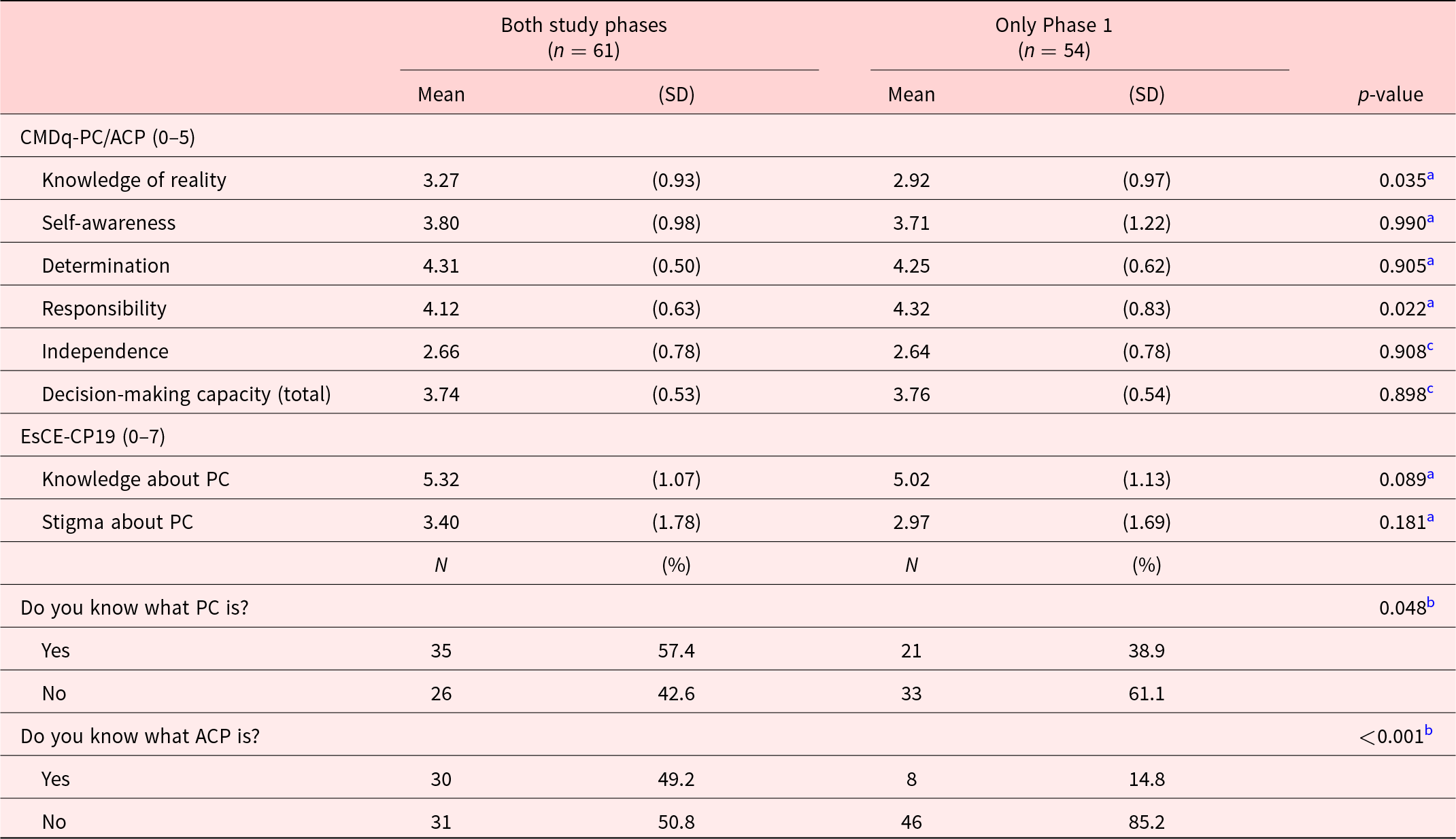
Regarding their levels of comprehension, decision-making capacity, stigmas, barriers, and awareness about PC and ACP, the patients who participated in both phases were compared to those who declined Phase 2, as shown in Table 2.
Table 2. Comparison of levels of comprehension, decision-making capacity, stigmas, barriers, and awareness regarding PC and ACP between patients who participated in both phases and who refused the second moment (only Phase 1)
N = number of participants; M = mean; SD = standard deviation; CDMCq-PC-ACP = comprehension and decision-making capacity questionnaire; EsCE-CP19 = Palliative Care Knowledge and Stigma Scale; PC = palliative care; ACP = advance care planning.
Statistical calculation:
a Mann–Whitney test.
b Pearson’s chi-squared test.
c Student’s t-test.
A statistically significant higher level of “knowledge of reality” (3.27 vs. 2.92, p = 0.035), and, interestingly, a lower level of “Responsibility” (4.12 vs. 4.32, p = 0.022) were observed in patients who participated in both phases compared with patients who refused Phase 2. When comparing levels of awareness of PC and ACP, differences were observed between the 2 groups in terms of their awareness about CP (57.4% vs. 38.9%, p = 0.048) and ACP (49.2% vs. 14.8%, p < 0.001, Table 2). In addition, patients who declined to participate in the second phase of the study had less knowledge about PC and ACP than patients who participated in both study phases.
Synthesizing the findings, it is suggested that patients’ personal and clinical profiles, along with their knowledge and attitudes toward PC and ACP, may influence their willingness to discuss these topics (Figure 2).
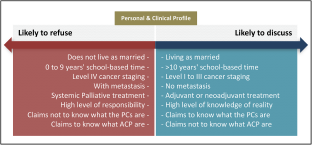
Figure 2. Characteristics of cancer patients more likely to accept or refuse PC and ACP discussions from the quantitative phase.
Subsequently, analyses were conducted in the sample of patients who participated in both phases (n = 61).
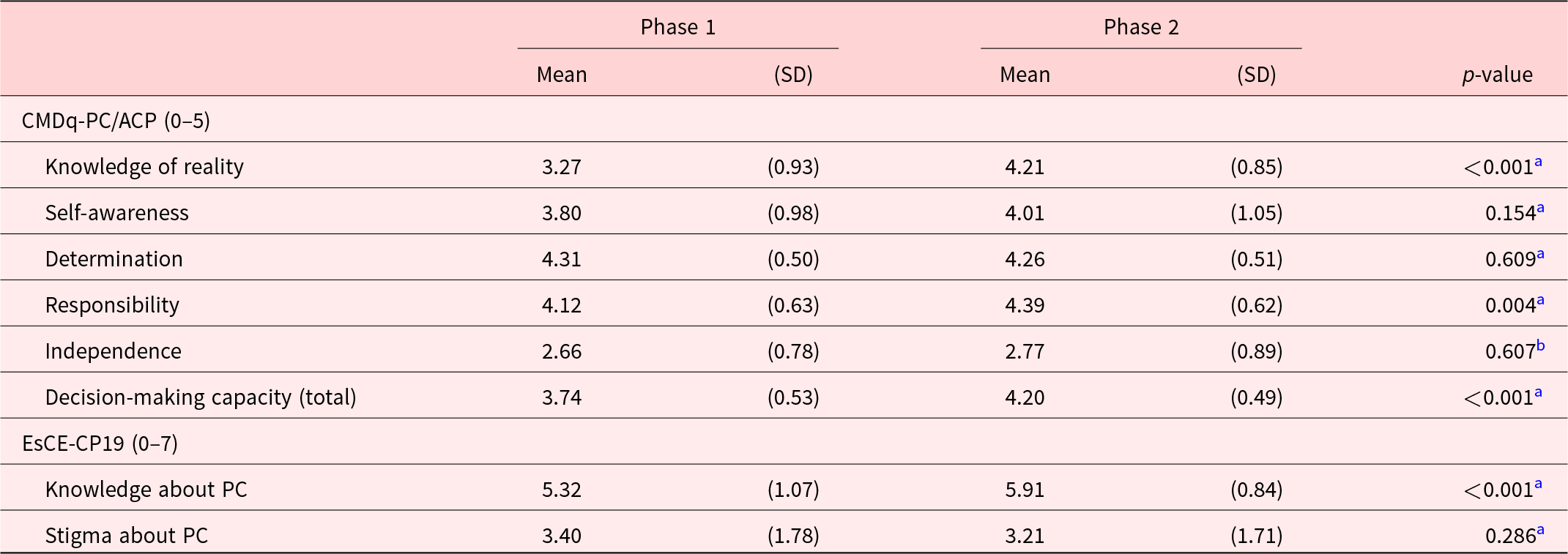
Initially, the participants were reassessed in the same domains evaluated in Phase 1 (Table 3).
Table 3. Comparison of comprehension, decision-making capacity, stigmas, barriers, and knowledge about PC and ACP over time between paired samples (n = 61)
N = number of participants; SD = standard deviation; CDMCq-PC-ACP = comprehension and decision-making capacity questionnaire; EsCE-CP19 = Palliative Care Knowledge and Stigma Scale.
Statistical calculation:
a Wilcoxon test.
b Student’s t-test.
A statistically significant improvement in patients’ “Knowledge of reality” from Phase 1 to Phase 2 (means 3.27 and 4.21, respectively; p < 0.001) was observed. Furthermore, the patients’ “Knowledge about PC” also made significant progress (means 5.32 and 5.91, respectively; p < 0.001), as identified by the EsCE-CP19 score, during that same interval. Additionally, there was a considerable increase in patient’ “decision-making capability” and “responsibility” over time (p < 0.001 and p = 0.004, respectively).
After completing the questionnaires in Phase 2, a total of 61 patients were asked qualitative guiding questions. Their answers were recorded transcribed in full, and a brief Bardin’s discourse analysis (Bardin Reference Bardin2016) was conducted. The related responses underwent a content analysis, which involved developing a systematic category system in 3 phases: pre-analysis, where researchers initially contacted and thoroughly read transcripts; exploration, selecting coding and classification units based on word meanings; and processing results by drawing inferences and interpretations to uncover hidden meanings. Following these steps, the researchers were able to systematically analyze the qualitative data and derive 5 significant categories that represent the main convergent themes and concepts of the text, as shown in the categories provided.
Timing is key – discussing PC and ACP at the right time and in the right way
Timing was critical in initiating discussions about PC and ACP, and patients stressed the importance of identifying the right time to ensure a clear understanding of diagnosis, prognosis, and treatment options. Starting these discussions early may reduce the risk of unnecessary suffering and distress by allowing patients to make informed decisions about their care. “With discussions being initiated earlier, they will not be as afraid and will not be thinking: ‘I am going to die, there is no hope.’ Therefore, we should initiate these conversations from the beginning, so that the person suffers less and understands what PC entails” (Patient 23).
Breaking the taboo – demystifying PC and ACP for patients
The patients in the study faced challenges in discussing PC and ACP due to misconceptions and societal taboos surrounding these topics. Providing clear explanations about the benefits of PC and ACP and addressing any misconceptions may help to break down these taboos and provide comfort for patients. “At first, it can be very overwhelming and frightening. However, people react differently – some may be frightened, while others may find it comforting. From the second consultation onwards, the patient is in a better state of mind, and not too much information stays in their head. There’s a lot of information to take in” (Patient 38).
Empowering patients – giving clear explanations and ensuring autonomy in PC and ACP discussions
Participants emphasized the importance of being empowered to make informed decisions about their care, including a clear understanding of the benefits and risks of PC and ACP. This allowed them to have greater control over their health care and make choices that were aligned with their values and preference. “It’s an advanced planning that ensures you don’t leave the decision in the hands of your family or doctors. For instance, at end-of-life, I wouldn’t want to be intubated […]. ACP is what I need to do so that neither my family nor doctors would make that decision for me because it’s not what I want” (Patient 71).
From misunderstandings to understanding – eliminating misconceptions about PC and ACP
Misunderstandings about PC and ACP prevented patients from receiving the necessary care and support. Providing accurate information is crucial in eliminating myths and misconceptions. “I used to think: ‘Palliative care? There’s nothing more that can be done for this person.’ However, this learning opportunity has shown me that it’s not quite like that” (Patient 35). “My guidance has greatly improved, and with the assistance of the ACP, people are able to live with more dignity” (Patient 53).
Open communication – discussing PC and ACP throughout the cancer journey
Open communication is crucial as patients preferred to discuss PC and ACP throughout their disease, to ensure necessary information for informed decisions. Discussing these topics can improve quality of life and reduce suffering. “When doctors provide care, they may say: ‘[…] You have been diagnosed with cancer, but do not worry, you will receive chemotherapy, radiation therapy, and we also have PC at the hospital, which is for pain management and quality of life. Regardless of how far your disease progresses or whether it can be cured, we will take care of you, your pain, and your emotions.’ This helps to put the person at comfort” (Participant 71).
A conceptual model was developed addressing the appropriate and inappropriate ways and moments to discuss PC and ACP with patients at different stages of cancer diagnosis and treatment (Figure 3).
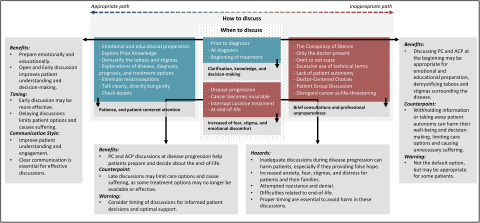
Figure 3. Conceptual model by the qualitative phase of the most appropriate time, and how the discussion about CP and ACP should be done.
Discussion
The study aimed to identify patients who were likely to discuss PC and ACP and their preferred timing and approach. Most patients with breast cancer preferred to begin discussing these topics early in their treatment journey, to alleviate fear, anxiety and receive support and guidance (Dans et al. Reference Dans, Kutner and Agarwal2021; Masi et al. Reference Masi, Gomez-Rexrode and Bardin2019; Tang et al. Reference Tang, Chen and Wen2019). Initially, some patients associated PC with death and were afraid, but they found it helpful and reassuring after learning more. Patients believed physicians should proactively discuss ACP and PC, which could improve knowledge, hope, overall well-being, and decision-making ability (Cohen et al. Reference Cohen, Althouse and Arnold2022; Masi et al. Reference Masi, Gomez-Rexrode and Bardin2019).
Marital status and level of education may influence individuals’ willingness to discuss PC and ACP. Married participants were more likely to discuss their care, suggesting that being married may provide advantages in addressing these issues compared to those who are not married. This may be due to the presence of a spouse who may provide emotional support or the sense of belonging and connection that comes from being in a committed relationship (Stegmann et al. Reference Stegmann, Geerse and Tange2020).
Additionally, education levels may indicate a greater interest in understanding of the importance of engaging in these discussions (Yoo et al. Reference Yoo, Lee and Kang2020). These findings are consistent with a study (Ejem et al. Reference Ejem, Dionne-Odom and Turkman2018), which found that highly educated women prefer a collaborative approach to decision-making. The absence of education and information regarding ACP affects the general population in Brazil (Tardelli et al. Reference Tardelli, Forte and Vidal2023). A recent cross-sectional survey conducted in the Southern region of the country revealed that only 2 individuals out of 48 patients attending an outpatient clinic at a teaching hospital were aware of ACP (Guirro et al. Reference Guirro, Ferreira and Vinne2022). Given the current challenges facing Brazilian society, such as the growing aging of the population and the increase in chronic diseases, the implementation of ACP and the discussion about PC are imperative for patient knowledge and, consequently, shared and humanized care (Dias et al. Reference Dias, Bezerra and Barra2022).
Patients with advanced cancer (including higher TNM stage and presence of distant metastasis) may be more hesitant to engage in these discussions. Women with advanced breast cancer feel less capable of making decisions on their own as the disease progresses, preferring a less active role (Ejem et al. Reference Ejem, Dionne-Odom and Turkman2018). A significant aspect to consider is the fear associated with discussing disease progression and death. Many patients experience apprehension when confronted with the prospect of their illness worsening or facing the end-of-life. This fear often stems from the uncertainty of the future, the emotional distress of confronting mortality, and the potential impact on loved ones. Furthermore, a lack of acceptance of the disease and the adoption of strategies, such as avoidance and denial, can further hinder open and honest conversations about prognosis and end-of-life preferences (Bergerot et al. Reference Bergerot, Philip and Bergerot2022; Pijnappel et al. Reference Pijnappel, Dijksterhuis and Sprangers2022). This is an essential consideration for health-care providers who need to develop or adjust interventions to encourage patient participation in such discussions based on their clinical condition. As an advanced disease stage may reduce patient engagement, these characteristics may reinforce the significance of initiating discussions at an early stage.
The results also reveal that patients with a better knowledge of reality about PC and ACP may be more willing to participate in discussions related to these topics because they have a clearer understanding of the benefits and importance of these conversations. They may also feel more confident in their ability to make informed decisions about their care and future (Hou et al. Reference Hou, Lu and Yang2021). On the other hand, patients who perceive a higher level of responsibility, such as being the primary provider for their family, may feel overwhelmed by the prospect of making such important decisions and may be more inclined to refuse or postpone these discussions. They may also feel a sense of duty or obligation to continue fighting the disease, which can make it difficult to consider PC or ACP. In addition, a large number of patients have confidence in their family members or health-care providers to make appropriate decisions on their behalf, even if they haven’t explicitly communicated their health-care preferences to them (Hou et al. Reference Hou, Lu and Yang2021).
The results obtained in the group or patients that participated in both study phases showed a significant improvement in patients’ knowledge of reality, responsibility, decision-making capacity, and awareness about PC. However, there was no significant difference in the stigma associated with PC. While education about PC and ACP may effectively improve patients’ knowledge of these topics (Cattagni Kleiner et al. Reference Cattagni Kleiner, Santos-Eggimann and Fustinoni2019), this educational approach alone may not be sufficient to reduce the stigma associated with PC and ACP as processes related to death and dying. Thus, to reduce stigmas and improve patient engagement, health-care teams should also address the emotional barriers that prevent patients from participating in discussions about their own care (Stegmann et al. Reference Stegmann, Geerse and Tange2020). A previous study indicates that to improve the process of making informed choices regarding PC and ACP, it is necessary to expand the scope of performance status beyond physical well-being and take into account psychosocial requirements and cognitive status as well (Kida et al. Reference Kida, Olver and Yennu2021).
In addition to knowledge, understanding these barriers can aid in better comprehending the disease process and treatment options, thereby increasing patients’ ability to make informed choices and take responsibility for their care (Cattagni Kleiner et al. Reference Cattagni Kleiner, Santos-Eggimann and Fustinoni2019; Santos Neto et al. Reference Santos Neto, Paiva and de Lima2021). Additional efforts are required to provide educational or supportive measures to physicians, aimed at improving their ability to offer emotional support or convey empathy during significant discussions (Stegmann et al. Reference Stegmann, Geerse and Tange2020).
The performed analysis indicated that stigma toward PC was negatively correlated with several other variables, indicating that individuals may feel ashamed or embarrassment, leading them to avoid seeking help or openly discussing their treatment options. In a brief qualitative discourse analysis, fear, stigmas, and taboos about PC and ACP were generally related to difficult topics such as illness, death, and dying (Grant et al. Reference Grant, Back and Dettmar2021). Because of this, while some patients prefer to be informed about the possibility of PC from the beginning, others may feel overwhelmed and prefer to focus on treatment.
The timing of these conversations is crucial and should be customized to meet the psychological state and individual needs of each patient. However, delaying these conversations until the later stages of the disease may leave patients feeling unprepared and caught off guard, with insufficient time to process and accept the situation. It is generally agreed that such conversations should not be postponed until the last moment, as this could lead to false hope or panic. Therefore, timely communication and education can contribute to improving the quality of life of patients and their families.
It is important to note that some patients may not be ready to discuss PC right away, and the timing may depend on the individual patient’s emotional state and readiness to accept the information. Therefore, doctors should approach the conversation about PC and ACP in a compassionate and empathetic manner, taking into consideration the patient’s needs and preferences (Cattagni Kleiner et al. Reference Cattagni Kleiner, Santos-Eggimann and Fustinoni2019). Patients appreciate honesty and transparency from their doctors. Additionally, it is important to offer ongoing support and resources to patients and their families throughout the PC and ACP process.
In conclusion, the main impact of these discussions emphasizes the importance of patient-centered communication in cancer treatment. Discussing PC and ACP with patients early and openly respects their autonomy and preferences and provides emotional and educational support throughout the disease trajectory. By doing so, patients may cope with the challenges of cancer and achieve a better decision-making capacity during their journey.
The study has some limitations, such as the discontinuation of some patients in the second phase. However, this loss was expected, especially in studies with this type of patient evaluation profile, which did not compromise the sample size for qualitative analysis, which was satisfactory. Another limitation was the inclusion of only female patients with breast cancer, which could reduce the generalizability of the results due to possible differences in evaluations in male patients or those with other types of cancer. The study was conducted at only 1 oncology treatment center. However, the hospital where the research was conducted serves patients from all 5 regions of Brazil and is a reference in oncology care in Latin America. Future studies are necessary to evaluate education strategies that can increase patient knowledge about PC and ACP, contributing to the minimization of knowledge barriers related to these topics.
Acknowledgments
The authors would like to express our gratitude to the Barretos Cancer Hospital, particularly the team of doctors, nurses, and nursing technicians at the Chemotherapy Infusion Center. They would also like to thank all the patients who participated in the study, as well as their family members who provided necessary support, especially during the second phase. Lastly, the authors extend a special thanks to the members of the GPQual for their unwavering and invaluable support.
Funding
This work was supported by the National Council for Scientific and Technological Development (CNPq) [BSRP, grant number 313601/2021-6] and São Paulo Research Foundation (FAPESP) [LFdA, grant number 2022/03842-1].
Competing interests
Nothing to disclose.
Ethical approval
All study processes were approved by the Ethics and Research Committee of the Hospital de Câncer de Barretos, under registration number 4.987.629.









