Youth engagement in health
As the global population surpassed 7 billion in 2012, a little over 50% of it constituted those aged 30 years or younger (Johnston et al., Reference Johnston, Crilly, Black, Prescott and Mercer2019). The role of young people as key agents for social change, economic growth and technological innovation has long been recognised by the United Nations (UN) (Bulc et al., Reference Bulc, Al-Wahdani, Bustreo, Choonara, Demaio, Jácome, Lal, Odede, Orlic, Ramchandani and Walji2019; Marcus & Cunningham, Reference Marcus and Cunningham2016; United Nations, 2013). Evidence has shown that as educators, young people have the power to challenge negative attitudes in a manner that is both impactful and engaging, which makes them well positioned to drive change and influence their communities (Marshall, Reference Marshall2019; Struthers et al., Reference Struthers, Parmenter and Tilbury2019). The transformational potential of young people to drive progress towards universal health coverage can, however, only be achieved through participatory leadership (Bulc et al., Reference Bulc, Al-Wahdani, Bustreo, Choonara, Demaio, Jácome, Lal, Odede, Orlic, Ramchandani and Walji2019; Marcus & Cunningham, Reference Marcus and Cunningham2016). As such, youth engagement has never been more vital to ensure actions meet these generations’ needs and to help young people reach their potential.
Partnerships between young people and more senior experts to drive meaningful change have been led and facilitated by various organisations, including intergovernmental organisations, donors and foundations, agencies of the UN, and the World Health Organization (WHO) (Checkoway, Reference Checkoway2011; UN, 2013; Zeldin et al., Reference Zeldin, Christens and Powers2013). The UN has acknowledged the need to work for and with young people in achieving the Sustainable Development Goals (SDGs). With the launch of the UN Youth Strategy (Office of the Secretary-General’s Envoy on Youth, 2018) in 2018, the WHO committed to action on meaningful youth engagement. The WHO released a global report citing strategic recommendations, with emphasis on: (1) leadership; (2) country impact; (3) focusing global public goods on impact and (4) partnerships (WHO, 2018b). The review identified more than 60 organisations that are potential partners with WHO in young people’s engagement on health. However, funding to support young people’s enthusiasm and make space for this demographic remains a challenge. Knowing the challenges ahead, the report acknowledged the need to forge creative new partnerships with diverse organisations that engage with young people and to work with partners to identify and develop potentially innovative funding sources (WHO, 2018b). In the primary health care (PHC) space, youth-led organisations such as the International Federation of Medical Students’ Associations and International Pharmaceutical Students’ Federation maintain official partnerships with the WHO. Despite their indispensable contributions, youth voices in the global health policy-making arena have been limited (Lal et al., Reference Lal, Bulc, Bewa, Cassim, Choonara, Efendioglu, Germann, Hafeez, Iversen, Nishtar and OʼLeary2019). Groups such as the Young Primary Care Experts of the European Forum for Primary Care (You&EFPC), the Young Forum Gastein of the European Health Forum Gastein (YFG-EHFG) and the Youth Forum of the European Public Health Association (EUPHANxt) have passionately represented the youth spirit on the common public health agenda in the European region over a decade. Nevertheless, a youth movement with a global membership with diverse traits, skillsets and experiences that is able to create a collective momentum towards achieving goals of global interest neither existed nor was publicly envisioned by any public health organisation.
In light of this, the WHO launched the PHC Young Leaders’ Network (YLN; WHO, 2018c) at the Global Conference on PHC in Astana in 2018. The convening of young professionals as a community of practice (CoP) emphasised the key role of youth in improving PHC and delivering on the Astana Declaration (WHO, 2018a). CoPs typically comprise of mutual engagement, joint enterprise, shared repertoire, collective competence, shared identity, commitment to a cause, collective learning, thinking together and regular interactions (Li et al., Reference Li, Grimshaw, Nielsen, Judd, Coyte and Graham2009; Pyrko et al., Reference Pyrko, Dörfler and Eden2017; Wenger, Reference Wenger2011). The attributes, dynamics and activities of the YLN described in this paper portray how they comprise a CoP. This paper demonstrates the scope for young professional-led CoPs in fostering support systems for young leaders and strengthening the delivery of PHC at local, regional and global levels; with examples from the YLN.
The YLN CoP
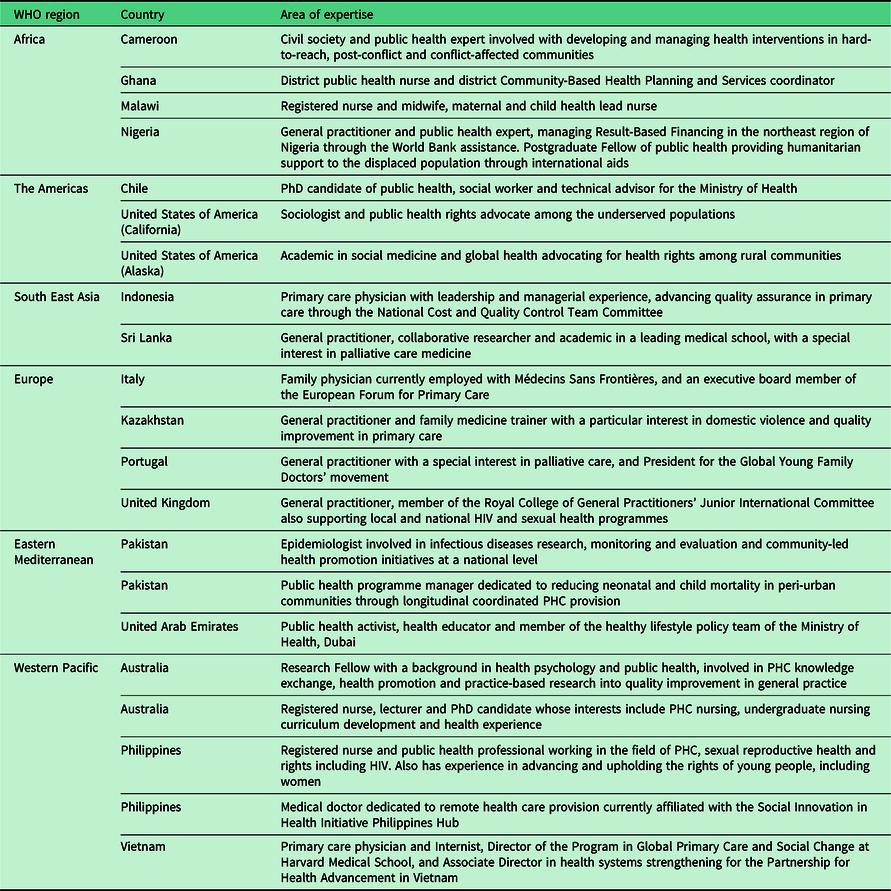
The YLN’s mission encompasses working individually and through interdisciplinary collaboration to advance the science and practice of PHC. This CoP was formed with two main ambitions: (1) to drive authentic engagement with youth in PHC and (2) to leverage meaningful engagement to improve PHC in the communities members work in. The 21 members were selected from over 2000 applicants as those who had demonstrated outstanding leadership qualities in PHC development in their respective regions. The YLN’s strength is the membership’s diverse expertise. Akin to PHC’s broad scope, the WHO recognised the importance of recruiting professionals from a variety of disciplines and socio-economic contexts across all six WHO regions (see Table 1).
Table 1 Composition of the inaugural Young Leaders’ Network
The YLN provides a unique PHC voice among those advocating for youth engagement (Bulc et al., Reference Bulc, Al-Wahdani, Bustreo, Choonara, Demaio, Jácome, Lal, Odede, Orlic, Ramchandani and Walji2019), but beyond that, it has an impact through members making changes in their own settings. It is important that youth movements such as this demonstrate not only what youth can do but what youth are already doing. Box 1 illustrates some of the successful strategies the YLN CoP adopted to produce positive outcomes during their term and as they continue engagement. These facilitators can be used to inform the development of similar networks in the future.
Box 1. Key elements in building a CoP to strengthen PHC
Facilitation (bringing together PHC professionals from around the world)
-
Influential organisational lead as initial coordinator
-
Group comprised of multidisciplinary, cross-country professionals
-
Opportunities to engage with senior experts/access to mentors
-
Provision of project opportunities (e.g., presentations, input to technical documents) and support for CoP-led projects (e.g., collaborative research)
-
Lead coordinator committed to listening openly to ideas presented by members
Activities (driving change to strengthen PHC)
-
Shared passion for PHC, vision and goals of achieving health for all
-
Developing professional identity
-
Cross-disciplinary learning underpinned by mutual respect and openness
-
Formal and informal methods for providing clinical and research advice to each other
-
Requesting feedback on WHO documents (e.g., Operational Framework)
-
Publishing regular blogs in WHO’s PHC newsletter, featuring YLN members’ work and perspectives
-
Ongoing training and skill development
-
Scaling up advocacy
-
Connecting with other youth-led agencies
Fit-for-purpose communication tools (exchanging ideas to inform future PHC initiatives)
-
Regular opportunities to connect
-
Face-to-face meetings facilitating a platform of support and opportunities to develop key connections
-
Informal gatherings
-
Use of web-based platforms for formal discussion fora
-
Use of social media (e.g., WhatsApp) for easy, rapid questions, sharing of resources and provision of support
The benefits of young professional-led CoPs for PHC
Specific attributes of the YLN manifest in significant impacts within and outside the CoP. For instance, involving young professionals with experience from critical frontlines of PHC practice, research and policy in different regions means a wealth of opportunities for members to learn from each other. These interactions enhance critical thinking, thus leading to developing sustainable solutions for the challenges within members’ own contexts (Withers et al., Reference Withers, Press, Wipfli, McCool, Chan, Jimba, Tremewan and Samet2016). A CoP not only benefits the members but also the communities to which they belong, by increasing social competence and embedding a sense of social responsibility.
The WHO engaged the network by supporting a number of diverse activities, including webinars, mentorship links and in-person meetings. These engagements have enhanced each members’ leadership skills and in turn have influenced their individual work and output in their respective countries. At a local level, CoPs such as the YLN offer insights into current training processes and frontline experiences of PHC service providers, researchers and policy-makers. They promote access to information about what works in PHC and which elements need strengthening. They also facilitate relationships between individuals; working in partnership with other CoP members allows individuals to build capacity and learn from others enacting similar programmes in different areas. For example, Rehan Adamjee from Pakistan works with a local non-governmental organisation, and the Aga Khan Medical College to deliver longitudinal, coordinated PHC services to communities on the outskirts of Karachi. The work has helped to reduce the under-5 mortality in these areas by 40% over a 4-year period. Rehan has leveraged insights from global professionals through the YLN, and through meeting other practitioners at global health events. His growing experience has helped him refine his work within his local community and expand it to new communities across Karachi. Similarly, Edmund Duodu is a District Public Health Nurse from Ghana who is currently providing crucial PHC services in hard-to-reach communities through his community-based organisation, ‘Divine Mother and Child Foundation’. Through the YLN, he has been able to meet and work with senior health officials in Ghana to drive local improvement strategies towards strengthening PHC.
Another young leader whose work experience in the YLN contributed to improving her work as a PHC professional is Victoria Gichohi. Victoria currently works as a health educator in the Los Angeles County Department of Public Health. In this role, Victoria has provided training to caregivers and health care administrators on the basics of COVID-19, which has been funded by a grant from the Centers for Disease Control and Prevention. Victoria has facilitated virtual training to over 200 participants in Los Angeles County. Through her participation in the YLN, she has gained the proper tools to support and assist this population. To date, Victoria stays passionate in helping underserved communities within Los Angeles, USA.
At a country or regional level, bringing together young professionals from diverse areas enhances knowledge exchange across countries. For example, Dr. Audu Lucky Emmanuel is a general practitioner who has served vulnerable populations in northeast Nigeria through humanitarian support and strengthening government institutions through performance-based financing. He led a team of PHC workers in rural Borno state, providing comprehensive PHC to those affected by the ongoing Boko Haram terrorist conflict. His YLN involvement has enabled him to study primary care in fragile health systems under one of the field’s global experts. Dr. Audu was able to link with global health professionals at the 2019 Primary Care 2030 Dialogue in Dubai. Through connecting with YLN member Dr. David Duong (physician, technical advisor and programme director), Dr. Audu was able to interact with PHC stakeholders from Kenya and also Vietnam, where he gained knowledge about innovative digital strategies being implemented in these regions, and took these lessons back to inform initiatives in his own region.
Certain resourceful collaborations the team members developed through attending the global health events have enabled ongoing benefits to their respective regions, beyond the YLN’s initial term. For instance, Dr. Chamath Fernando, a Sri Lankan academic General Practitioner, and a palliative care enthusiast, through the relationships he had formed with the International Association for Hospice Palliative Care through the years, is currently attracting expertise and guidance from a wealth of global primary palliative care clinicians and academics towards the development of a Postgraduate Diploma in Palliative Care for Sri Lankan General Practitioners. Furthermore, he anticipates working further with the Asia Pacific Primary Palliative Care Special Interest Group that was derived recently consequent to these collaborations, towards attaining regionally shared agendas.
CoPs can have global impact by connecting advocates around the world. For example, the YLN members represent 17 countries. This provides a glimpse into PHC in different contexts and enables the widespread, global dissemination of new information, new technologies and new skills. Technology facilitates regular communication within CoPs, mitigating the restraints imposed by geographical boundaries. For example, the YLN leverages social media such as WhatsApp for problem-solving. These tools are indispensable in allowing members to connect more liberally and rapidly thus mobilising support, advice and resources. For instance, as physician Dr. Andrea Canini sought advice to roll out an immunisation initiative within Sierra Leone, guidance came via WhatsApp from colleagues such as Lundi-Anne Omam Ngo Bibaa who had trialled similar approaches through her humanitarian work in Cameroon.
When needing a ‘deep dive’ into key policy or practice areas, formal platforms can be used for regular webinars and discussion fora. For example, during the COVID-19 crisis, the YLN members partnered with another international PHC programme for a webinar series, sharing insights on frontline experiences of pandemic responses and the future of PHC in the post-pandemic era (Harvard Medical School Center for Primary Care, 2020). This global series was evidence that once established, the YLN has remained viable (independent of WHO facilitation) and adaptable to the most pressing health issues in the world. The value of frontline PHC perspectives was highlighted in these webinars as members presented lessons from their experiences to rapidly problem-solve, share knowledge and adapt successful strategies to their different contexts. This was only possible by having strong connections and communications well established prior to the pandemic.
What is the future for youth-led PHC CoPs?
The YLN (and similar CoPs) must acknowledge some barriers in terms of sustainability. These include issues such as time commitment among already busy members, tackling time differences in trying to organise meetings, accounting for changes in priorities (e.g., shift away from a focus on SDGs to frontline support for COVID-19) and maintaining commitment without funding to support face-to-face connections or an ongoing facilitator to support regular meetings. However, young professional-led CoPs are underpinned by passion and determination to improve intergenerational futures. These barriers are thus overcome by agility; with activities such as supporting different means of connecting (i.e., social media, web-based communication forums that can be accessed when convenient to members), encouraging champions within CoPs to step up and take on a facilitation role when there is no longer a formal coordinator in place, and changing agendas to reflect current priorities/adapting goals to reflect the wider context. The YLN represents a community that is striving to make a real difference. While meetings are less frequent than in the initial stages, communication and shared activities continue, enabling progress.
Youth-led movements have great potential to inspire other young people, as well as future generations, to make meaningful contributions to their communities. By recruiting members from clinical, policy and academic settings, the YLN’s breadth of experience models young professionals’ diverse skillsets. It should be the goal of every youth network to continue communication with other youth groups and more experienced experts globally. By building connections now, young people can foster a larger worldwide network that is prepared to take on the significant PHC roles and responsibilities that await them.
Whilst there are rapid technological and scientific advancements to aid the delivery of PHC, there remain many challenges. One challenge is the pervasive spread of misinformation on social media platforms, such as with vaccinations (Smith & Graham, Reference Smith and Graham2019). In light of this, young leaders acknowledge their obligation to spread evidence-based information on trusted platforms that are easily accessible to communities. In this way, young PHC professionals remain embedded within the WHO Youth Engagement Strategy, with the WHO engaging young people through the design and delivery of global public goods and in innovative partnership-driven platforms where they can continue sharing experiences whilst driving change (WHO, 2018b).
Through their research, education and training, or direct fieldwork, it is the young leaders’ goal to continue their involvement in addressing PHC workforce shortages by decreasing siloes through the integration of care teams (i.e., allied health, social care, community health workers, civil society and tertiary care), training communities and health care workers in emergency preparedness and response, engaging communities in building resilience, and presenting innovative strategies to improve accessibility to aspects of PHC with limited resources (e.g., palliative care), in various contexts.
Conclusion
Globally, it is recognised that young people have the responsibility for continuously advocating to improve PHC at global, regional and local levels in order to influence change within their communities from a grassroots level. As an innovative CoP with demonstrated benefits to individuals, communities and the global youth movement, the YLN offers a powerful example of how youth can be meaningfully engaged in strengthening PHC.
The CoP model’s strengths are that it is dynamic, flexible and driven by passionate young PHC advocates, particularly valuable when facing PHC challenges such as the COVID-19 crisis. CoP members can continue to work tirelessly in both individual and collaborative capacities to (a) increase PHC’s visibility and (b) bring PHC closer to their communities.
Potential weaknesses or challenges are in ensuring sustainability within a changing context and limited facilitation support. However, determination, shared identity, agility and commitment allow CoP members to strive together to achieve a better future for PHC. Another challenge of the YLN is that of continuous online engagement with the entire CoP. The time difference between continents contributes to limiting group engagement. However, with a clear plan and group facilitator, this challenge can be overcome.
Moving forward, the YLN seeks opportunities to continue meaningful engagement with other active youth groups and experts in the field working towards the SDGs, to form a broader base and find shared, innovative solutions to PHC challenges. Collaboration and engagement with other active youth groups might contribute towards sustaining the YLN CoP.
PHC has never been more important than in the current climate of the COVID-19 pandemic. While this threatens the focus for young leaders, it also presents a chance to advocate strongly in a time where the whole world is talking about health. For the YLN, there is a desire to use the foundation of the CoP to share knowledge, evidence and resources to inform clinical and public health activities, policy initiatives, health activism and research projects that would serve to advance the science and practice of PHC and improve health outcomes for communities globally.
Acknowledgements
The authors would like to acknowledge the broader WHO PHC Young Leaders’ Network and our YLN facilitators at the WHO.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors. However, the YLN activities from 2018 to 2019 were funded by WHO.
Conflicts of interest
The authors are all members of the YLN.
Authors’ contributions
All authors made substantial contributions to the conception and design of this work. They were involved in drafting the manuscript, revising it critically for important intellectual content and giving final approval of the version to be published. Each author has participated sufficiently in the work to take public responsibility for appropriate portions of the content. The authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethical standards
All YLN members cited in this paper gave consent for their information to be used.




