Air travel is now widely available and used by large numbers of people. Heathrow Airport, for example, served more than 50 million passengers to about 200 destinations worldwide in 1998. There are only few studies addressing the psychiatric problems associated with air travel. Anxiety is common among air travellers (Reference Iljon FOREMAN and IljonIljon Foreman & Iljon, 1994; Reference McIntosh, Swanson and PowerMclntosh et al, 1998). Serious psychiatric disturbances have been observed (Reference Miller and ZarconeMiller & Zarcone, 1968; Reference ShapiroShapiro, 1976; Reference Jauhar and WellerJauhar & Weller, 1982; Reference Lowe-PONSFORD and BeggLowe-Ponsford & Begg, 1996) but the frequency of severe psychiatric disturbances at international airports is largely unknown. The aim of this study was to assess frequency, presentation and safety implications of profound psychiatric disturbances at Heathrow Airport.
Method
Subject selection
Adult patients (age >16 years) who were admitted from Heathrow Airport after being detained by Heathrow police between 1 March 1995 and 28 February 1999 were included. All patients appeared to be suffering from mental disorder and in immediate need of care and control to the police. They were taken to a place of safety under Section 136 of the Mental Health Act 1983 and admitted to Hillingdon Hospital after assessment by a psychiatrist and a social worker. Hillingdon Hospital served as the place of safety for Heathrow Airport; we were therefore in the position to obtain complete data on this patient population. We used an electronic database from the contracts and information department of the hospital and data regarding patients from Heathrow Airport from our bed manager (M.A.). For each patient we verified the admission from Heathrow Airport under Section 136 using the social worker's report. The identified names were cross-checked with a list of mental health assessments provided by social services. To minimise the chance that patients had been taken to another hospital (in violation of the policy) we contacted the doctors who are involved in Mental Health Act assessments, the bed managers of neighbouring hospitals, Heathrow police and social services.
Data collection
The following data were collected: name, gender, age, date of admission, date of discharge, ICD—10 diagnosis (World Health Organization, 1992), nationality, circumstance of admission, arrival from where, clinical presentation (psychotic, violent, aggressive, wandering, deliberate self-harm (actual or threatened), incident that happened in the air, disrupting air travel, self-neglect, repetitive presentation, other) and follow-up arrangements. Information on the clinical presentation and travel details was obtained from the approved social worker's report. This standardised report contained the following sub-headings: (a) reason for referral; (b) family and home situation; (c) social factors; (d) cultural factors; (e) details of interview; (f) consultation with doctors; (g) consultations with nearest relative/others; (h) alternatives considered; and (i) risk assessment/conclusions.
Classification of mental disorder
At the time of discharge the patient's mental disorder was coded by the treating psychiatrist using the ICD—10 classification of mental and behavioural disorders (World Health Organization, 1992).
Patients not included in this study
This study does not include people with mental health problems who had been dealt with by other passenger services such as stewardesses, etc.; those not suffering from mental illness and who were arrested and charged for criminal offences; those who presented to the hospital voluntarily without police involvement and were admitted without formal Mental Health Act assessment (‘informal admissions’) and; persons who were initially detained by Heathrow police but where a mental health assessment revealed that contained detention was not justified.
Results
Two hundred and ninety people were brought to Hillingdon Hospital by Heathrow police, of whom 220 were admitted, 153 on Section 2 of the Mental Health Act. Data were incomplete in 30 patients, who were excluded, leaving 190 for further analysis. One patient was admitted twice.
Demographic data
The mean age was 36.8 years (s.d. 12.13). Eighty-one patients (43%) were female, 109 (57%) were male. One hundred and thirty-seven patients (72%) were nationals in European states. Thirty-one patients (16%) were nationals in states in North or South America. Thirteen patients (7%) were nationals in states in India, South East Asia, the Pacific region or Australia. Nine patients (5%) were from the Middle East or Africa.
Sixty-eight patients (one-third of all Section 136 admissions) were detained by the police after their arrival by plane. In the same period 98 200 000 passengers had arrived at Heathrow Airport (6.93 admission per 10 million arriving passengers). Patients were arriving from different regions; the admission rates from different regions were similar (admission rate 3.2 per 10 million arriving passengers from Africa and Middle East, 4.7 per 10 million from Asia, 7.3 per 10 million from America and 7.9 per 10 million from Europe).
One-hundred and twenty-two patients (two-thirds of all admissions) had entered Heathrow Airport from within the UK. In the same period 98 030 000 passengers had departed from Heathrow Airport (1.22 admission per 1 million departing passengers). Thus, the admission rate was about five times higher in patients arriving from within the UK than in patients arriving by plane. Taking patients arriving by plane and patients arriving from the UK together, there were 9.68 admission per 10 million passengers from Heathrow Airport.
Clinical presentation
Fig. 1 shows the clinical presentation. The most common presentations were psychotic or bizarre behaviour, aggression and wandering. Bizarre behaviour at the airport often caused security concerns. For example, sniffer dogs were used to recover a patient's clothes that he had buried in rabbit holes. Another patient caused security concerns because of refusal to board the plane after the luggage had been loaded on the plane. Violent behaviour was reported only in 14% of patients (1.3 in million passengers), threatening self-harm or inflicting minor self-harm (i.e. superficial cutting) occurred in 11% or 1 in 10 million passengers. Wandering was the third most frequent clinical presentation. Twenty per cent of patients presented as ‘wandering’. Of all wandering patients 50% had psychotic symptoms in addition to wandering, 20% were aggressive and/or violent. Schizophrenia or schizotypal disorder were the most common diagnoses in wandering patients.
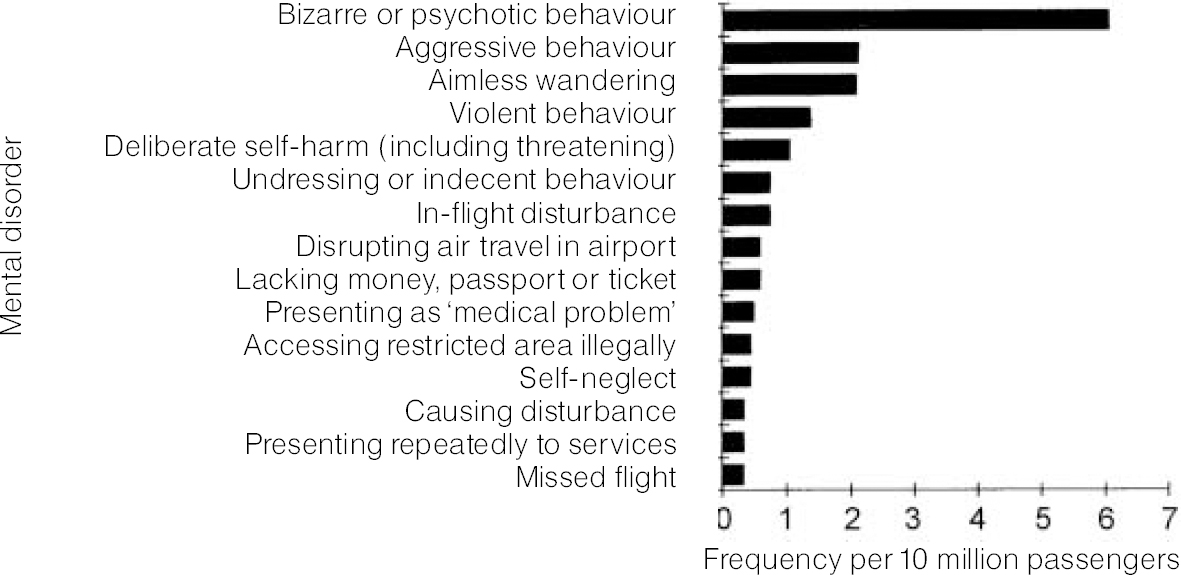
Fig. 1 Presentation of mental disorders at Heathrow Airport per 10 million passengers
Fourteen of 68 arriving patients (21%) had caused in-flight disturbances. Most common was aggressive behaviour (seven patients); one patient with mania tried to open the door during the flight. Less severe incidents include pouring water over a fellow traveller; screaming; and undressing in the toilet. Nine patients had schizophrenia or a schizotypal disorder, five patients had mania. There was no increase of incidents per year over the study period.
Psychiatric diagnosis
Fig. 2 shows the spectrum and frequency of mental illnesses in patients from Heathrow Airport.
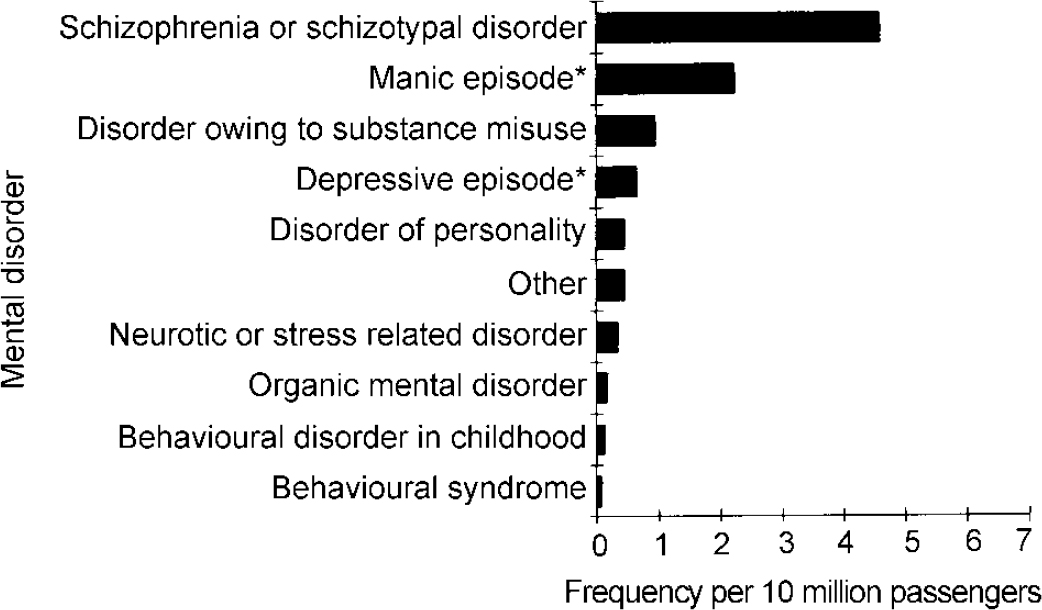
Fig. 2 Frequency of presentations of mental illness at Heathrow Airport per 10 million passengers *Single episode or in the context of a bipolar affective disorder.
Follow-up arrangements
The mean stay was 9.75 days (s.d. 14.4), median 6 days. The distribution of stay in the hospital was skewed (skew 4.08), with a high proportion staying less than a week (52%). Eighty (42%) patients were transferred to another psychiatric hospital in the UK or overseas for further treatment. Fifty-five patients required repatriation to an overseas destination with an escort from the Hillingdon Hospital.
Discussion
Our data show that compulsory psychiatric emergency admissions from Heathrow Airport are, compared with the large number of air travellers, only rarely required. Only about one person in 1 million passengers required emergency psychiatric admission after detention by the police. The majority of patients presented with bizarre and at times disruptive, but not dangerous, behaviour. Wandering was a frequent and important symptom of mental illness at Heathrow Airport. This finding is in agreement with Shapiro (Reference Shapiro1982).
Our study demonstrated that patients admitted under Section 136 from Heathrow Airport frequently had severe mental illness. This result is very similar to the result of a study performed approximately 18 years ago at the same airport. In that study 50% of admitted patients had schizophrenia and 29% had affective disorder (Reference Jauhar and WellerJauhar & Weller, 1982). In a study on patients from Kennedy Airport in New York, 74% had schizophrenia and 5% had an affective disorder (Reference ShapiroShapiro, 1976). The differences between the UK and American studies may be owing to differences in the diagnostic classification (Reference Gurland, Fleiss and CooperGurland et al, 1970). Nevertheless, both studies agreed with our study admitted patients from international airports frequently have severe mental illness. This finding is not merely a reflection of the subject selection; in an inner-London area (Reference SpenceSpence, 1995) the same selection criteria as our study were applied (detention by the police under Mental Health Act involving the same police force) but personality disorder was the primary diagnosis in about 30% of patients — far more than in our study. The different findings may reflect a different pattern of behaviour of patients with psychosis and personality disorder, the former having the tendency to travel (Reference ØdegaardØdegaard, 1932).
Patients only rarely caused in-flight disturbances. The frequency of in-flight disturbances caused by patients with mental illness in our study was much smaller than the reported frequency of physical medical emergencies in-flight; 1.4 psychiatric in-flight incidents per 10 million arriving passengers, as opposed to three in-flight medical emergencies per 100 000 arriving passengers (Reference Cummins and SchubachCummins & Schubach, 1989; Reference Speizer, Rennie and BretonSpeizer et al, 1989).
The frequency of all serious events caused by patients with mental illness, such as violent behaviour, disrupting air travel, deliberate self-harm, threatening self-harm and accessing restricted areas illegally, taken together, was four per 10 million passengers. This is well below the frequency of physical medical disorders at international airports, which have been reported to be about four per 10 000 passengers (Reference Antunano and AquinoAntunano & Aquino, 1989).
In conclusion, emergency admissions from Heathrow Airport and disturbances at the airport or in-flight were overall rare compared with the large numbers of travellers. A high proportion of patients from the airport suffered from schizophrenia or schizotypal disorder and mania. Follow-up studies could address the question of whether migratory tendencies persisted and whether these patients form a diagnostic entity. Airport wandering was a non-specific, but frequent sign of serious mental illness, which should be recognised.
Acknowledgements
We would like to acknowledge Sandy Van Brummen, Hillingdon Social Services and Richard Wainwright, BAA Research.





eLetters
No eLetters have been published for this article.