Background
Estimates of becoming a parent range from 39% to 63% among individuals with psychosis (Campbell et al., Reference Campbell, Hanlon, Poon, Paolini, Stone, Galletly and Cohen2012; Dazzan et al., Reference Dazzan, Lappin, Heslin, Donoghue, Lomas, Reininghaus and Morgan2020; Howard, Kumar, & Thornicroft, Reference Howard, Kumar and Thornicroft2001; Maybery & Reupert, Reference Maybery and Reupert2018; Radley, Barlow, & Johns, Reference Radley, Barlow and Johns2022a) with men and women diagnosed with schizophrenia having a 90% and 82% lower fertility rate than that of the general population, respectively (Laursen & Munk-Olsen, Reference Laursen and Munk-Olsen2010). Parents who have been diagnosed with severe mental illness may also experience more challenges associated with parenting than parents without mental health problems (Howard, Thornicroft, Salmon, & Appleby, Reference Howard, Thornicroft, Salmon and Appleby2004; Matheson et al., Reference Matheson, Kariuki, Green, Dean, Harris, Tzoumakis and Laurens2017; Radley, Barlow, & Johns, Reference Radley, Barlow and Johns2022b). From a small sample study, parents diagnosed with schizophrenia are more hostile and critical in their parenting style with increased expressed emotions (Gregg, Calam, Drake, & Wolfenden, Reference Gregg, Calam, Drake and Wolfenden2021). Also, parent–child relationships tend to be non-hierarchical with role reversal, where children are more responsible for their mentally ill parent (Boström & Strand, Reference Boström and Strand2021). Also, low socioeconomic position, single caregiver status, and having a partner who may also be diagnosed with a mental disorder (i.e. assortative mating [Greve et al., Reference Greve, Uher, Als, Jepsen, Mortensen, Gantriis and Mors2021]) are all factors associated with an increased risk of poor parenting (Hammond & Lipsedge, Reference Hammond and Lipsedge2015). However, it is essential to note that in a national Australian survey among individuals living with psychosis, the majority (76.6%) of parents provided good quality care for their children (Campbell et al., Reference Campbell, Hanlon, Poon, Paolini, Stone, Galletly and Cohen2012). Also, in a study from the UK, more than 70% of mothers with psychosis hospitalized in psychiatric mother and baby units were discharged with no further supervision and no significant parenting problems (Howard et al., Reference Howard, Thornicroft, Salmon and Appleby2004). After stratification by diagnosis, the majority of mothers with schizophrenia also left the unit without supervision (Howard et al., Reference Howard, Thornicroft, Salmon and Appleby2004). Still, a nationwide study from Denmark found an increased risk of having children (<18 years of age) placed in out-of-home care with a cumulative risk of 40% among mothers and 20% risk among fathers diagnosed with psychotic disorders (Ranning, Laursen, Thorup, Hjorthøj, & Nordentoft, Reference Ranning, Laursen, Thorup, Hjorthøj and Nordentoft2015). Also, families of parents with severe mental illness have elevated levels of unhealthy family functioning compared to the general population (Friedmann, Ph, Ryan, & Keitner, Reference Friedmann, Ph, Ryan and Keitner1997), and unhealthy family functioning in families affected by parental severe mental illness is associated with increased risk of relapse into acute phases of mental illness and lower recovery rates (Staccini, Tomba, Grandi, & Keitner, Reference Staccini, Tomba, Grandi and Keitner2015). Still, an association between parental symptom decline and improvement in parenting has been found (Kahng, Oyserman, Bybee, & Mowbray, Reference Kahng, Oyserman, Bybee and Mowbray2008).
As of now, few studies have been conducted investigating the long-term clinical outcomes among parents diagnosed with schizophrenia spectrum disorders. Originally, the participants in this study took part in the OPUS randomized controlled trial from 1998–2000, initiated to investigate early intervention services in psychosis compared to treatment as usual or hospital-based treatment (Jorgensen et al., Reference Jorgensen, Nordentoft, Abel, Gouliaev, Jeppesen and Kassow2000). Since no significant differences were found between the groups on long-term clinical outcomes, the trial participants have been merged into one cohort (Hansen et al., Reference Hansen, Starzer, Nilsson, Hjorthøj, Albert and Nordentoft2023). This study aimed to investigate clinical illness course among parents and non-parents as well as family-related outcomes in a clinical sample followed over 20 years after a diagnosis with a first-episode of schizophrenia spectrum disorder.
Method
Settings
From 1998 to 2000, the OPUS randomized controlled trial included 578 participants diagnosed with a schizophrenia spectrum disorder in accordance with the International Classification of Diseases, 10th revision (ICD-10) (World Health Organization, 1993); F20–F25, F28–F29. Participants were between 18 and 45 years of age and had not received more than 12 weeks of consecutive antipsychotic treatment. Originally, the OPUS trial was designed to investigate early intervention services (i.e. an integrated psycho-social treatment program carried out by a multidisciplinary team and lasted for two years) compared to the available community mental health treatment or hospital-based treatment (see Fig. 1). Detailed descriptions of the trial have been provided in previous publications (Bertelsen et al., Reference Bertelsen, Jeppesen, Petersen, Thorup, Øhlenschlæger, Le Quach and Nordentoft2008; Thorup et al., Reference Thorup, Petersen, Jeppesen, Øhlenschlæger, Christensen, Krarup and Nordentoft2005). Over the years, multiple follow-up studies have been conducted (Bertelsen et al., Reference Bertelsen, Jeppesen, Petersen, Thorup, Øhlenschlæger, Le Quach and Nordentoft2008; Gry Secher et al., Reference Gry Secher, Hjorthøj, Austin, Thorup, Jeppesen, Mors and Nordentoft2015; Hansen et al., Reference Hansen, Starzer, Nilsson, Hjorthøj, Albert and Nordentoft2023; Petersen et al., Reference Petersen, Jeppesen and Thorup2005a, Reference Petersen, Nordentoft, Jeppesen, Øhlenschlæger, Thorup, Christensen and Jørgensen2005b).
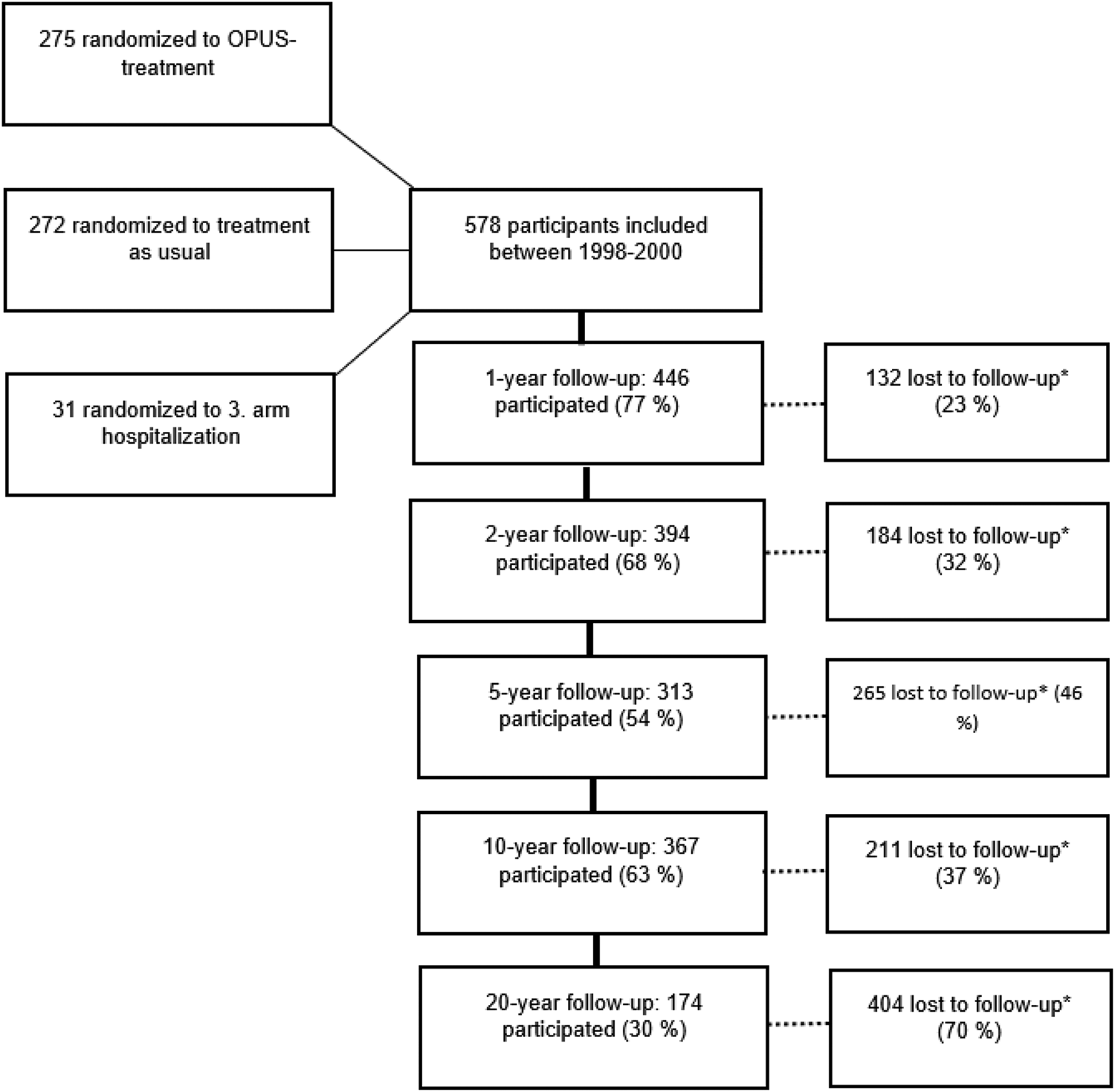
Figure 1. Flow-chart of participation through 20 years. *Number of lost to follow-up refers only to the specific follow-up year and participants could continue to be contacted and contribute to the study longitudinally.
Participants
We were able to recruit 174 participants from the original clinical sample of 578 with first-episode schizophrenia spectrum disorders in the 20-year follow-up assessment (See Fig. 1 for a flow-chart of participation over 20 years). For this study, we divided the clinical sample into two groups: 75 participants who had become parents before the 20-year follow-up (e.g. legal parents with or without custody) and 99 participants who had never become parents. Furthermore, we used the Danish registers (since this is a source of data free of attrition) to collect longitudinal data on all participants in the original OPUS trial, gathering a cohort of 219 individuals registered as parents and 359 registered as having no offspring. Written and informed consent was obtained from all participants, and compensation, including paid transportation, was offered in relation to the clinical interviews.
Clinical data assessment
Independent trained research assistants conducted the 20-year clinical interviews. (A) The Schedule for Clinical Assessment in Neuropsychiatry (SCAN 2.1) (Wing, Sartorius, & Üstun, Reference Wing, Sartorius and Üstun1998) was used to establish the main diagnosis within the schizophrenia spectrum by the ICD-10 (World Health Organization, 1993); F20–F25, F28–F29. (B) The Scale for Assessment of Positive Symptoms (SAPS) (Andreasen, Flaum, Swayze, Tyrrell, & Arndt, Reference Andreasen, Flaum, Swayze, Tyrrell and Arndt1990) and (C) the Scale for Assessment of Negative Symptoms (SANS) (Andreasen, Reference Andreasen1989) was used to assess psychopathology including global scores on two domains on SAPS (i.e. hallucinations and delusions) and four domains on SANS (i.e. affective flattening or blunting, alogia, avolition/apathy, and anhedonia/asociality). (D) Disorganized symptoms were measured using two domains from the SAPS (i.e. bizarre behavior and formal thought disorder) and one domain from the SANS (i.e. inappropriate affect). (E) The Global Assessment of Functioning (GAF) (Aas, Reference Aas2010). (F) the Personal and Social Performance Scale (PSP) (Tegeler & Juckel, Reference Tegeler and Juckel2007) were used to assess the level of functioning with both scales ranging between 0 and 100, where higher scores indicate better functioning. (G) Socio-demographic factors were evaluated by participants' self-report. (H) At baseline, pre-morbid social and academic functioning was assessed using the Pre-morbid Adjustment Scale (PAS) (Brill, Reichenberg, Weiser, & Rabinowitz, Reference Brill, Reichenberg, Weiser and Rabinowitz2008).
In addition, for all participants at the 20-year follow-up (I) quality of life was measured in four domains (physical health, psychological, social relationship, and environment) with the WHO Quality of Life-BREF (WHOQoL-Bref) (The WHOQOL Group, 1996; von Knorring, Reference von Knorring2001). (J) Symptom remission was defined as a score of 2 or less on all items on the Scale for Assessment for Positive Symptoms (SAPS) and Scale for Assessment of Negative Symptoms (SANS) for at least six consecutive months in accordance with the Remission in Schizophrenia Working Group (Andreasen et al., Reference Andreasen, Carpenter, Kane, Lasser, Marder and Weinberger2005). (K) Clinical recovery was defined as no psychotic episode, no psychiatric hospitalizations, no use of supported accommodation for two consecutive years before follow-up, currently studying or working, and a GAF-F score of 60 or more.
For the parental subgroup, we also aimed to investigate parenting behavior and caregiving capacities. Therefore, we included the following questionnaires: (L) The general functioning subscale (12 items) in the family assessment device (FAD) (Miller, Ryan, Keitner, Bishop, & Epstein, Reference Miller, Ryan, Keitner, Bishop and Epstein2000; Ridenour, Daley, & Reich, Reference Ridenour, Daley and Reich1999; Staccini et al., Reference Staccini, Tomba, Grandi and Keitner2015) was used to evaluate self-reported family functioning by parents with children (<18 years) living at home. Each item was scored on a four-point scale, with lower scores implying better family functioning. A cut-off score of ⩾2 equals unhealthy family functioning. (M) The Parental Stress Scale (PSS) (18 items) scored with a five-point scale (i.e. 1: strongly disagree, 2: disagree, 3: undecided, 4: agree, and 5: strongly agree) was used to measure levels of parental stress associated with raising children (<18 years of age) (Pontoppidan, Nielsen, & Kristensen, Reference Pontoppidan, Nielsen and Kristensen2018). The following eight items (i.e. items 1-, 2-, 5-, 6-, 7-, 8-, 17-, and 18) were reversely scored. A total score across all items was calculated, with scores ranging from 18 to 90 and higher scores implying higher stress levels associated with parenting. (N) The parent version of The Strengths and Difficulties Questionnaire (SDQ-DAN) (Five scales with five items each including prosocial scale, emotional problems scale, conduct problems scale, hyperactivity, and peer problems scale) (Obel et al., Reference Obel, Heiervang, Rodriguez, Heyerdahl, Smedje, Sourander and Olsen2004) was used to assess the parent's impression of the mental health of children aged 4–16 years for the past six months before the 20-year follow-up. A total difficulty score was generated by adding all the scales (except the prosocial scale) with a cut-off point of ⩾ 17, considered a high difficulty score.
Longitudinal register data
We used the Danish registers, with complete follow-up on all participants on a range of relevant outcomes: (O) The Danish Civil Registration System (Pedersen, Reference Pedersen2011) with continuous information on addresses and vital status as well as family units, including registration of legal parents. (P) Information about psychiatric service use, including the number of days of psychiatric hospitalizations, contact to psychiatric emergency rooms, and the number of outpatient contacts, were extracted from the Danish Psychiatric Central Register (Mors, Perto, & Mortensen, Reference Mors, Perto and Mortensen2011), (Q) Vocational status, part-time and full employment was extracted from the DREAM database (Statistics Denmark, n.d.).
Statistical analyses
Variables comparing parents to non-parents were tested individually using a t test if the variable was continuous or ordinal, or a χ2 test if the variable was categorical. We used Mann–Whitney's U test to test differences in continuous data with skewed distributions.
To investigate baseline predictors of parenthood, we conducted univariate logistic regression analyses (See eTable 1 and 2 in the supplement material) with the level of significance set to p = 0.05. Due to obvious reasons, we excluded all individuals who had become parents before first diagnosis (i.e. before study initiation/baseline). Afterward, we did a multivariate logistic regression including all significant variables from the univariate regression analyses, and then we used backward elimination to find significant predictors of parenthood. The variable, duration of untreated psychosis (DUP), was not included in the analyses due to high percentages of missing data at baseline.
Ethical standards
The authors assert that all procedures contributing to the OPUS trial have been approved by the Regional Ethical Scientific Committee (Protocol nr.: 17023873) and by the Danish data protection agency (RHP-2017-047, I-Suite nr: 05855) complying with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Furthermore, the trial has been registered at ClinicalTrials.gov NCT00157313.
Results
In the entire cohort of 578 trial participants, 219 (38%) individuals were registered as parents in the Danish registers. Of those who participated in the 20-year follow-up, 75 individuals (43%) had become parents to 135 children at the 20-year follow-up. Of these, 20 individuals had already become parents before the first diagnosis. Overall, 27 participants with offspring at the 20-year follow-up had one child, 36 had two children, and 12 had three children. At the time of the 20-year follow-up, the age of the children ranged from 2 to 45 years, and of these 72 (53.3%) children (aged < 18 years) were living with the participating parent, 19 (14.1%), were living with another parent or biological family, 8 (5.9%) were living in out-of-home care (e.g. foster care or institution), and the rest of the children were adult individuals (>18 years) living either at or away from home (n = 36, 26.7%). A total of 29 (38.7%) parents had self-reported single-caregiver status and lived alone with their children. For our sample, predictors of parenthood at baseline were younger age, being in a relationship, better premorbid social functioning, and higher levels of global functioning (See eTable 1 and 2 in the supplemental material).
20-year clinical interview data
At the 20-year follow-up, significantly more participants who had become parents were females, were in a relationship, and were working or studying (41.3% v. 21.2%, p = 0.004) compared to non-parents (Table 1). Furthermore, parents had significantly lower -psychotic, -negative, and -disorganized symptom scores compared to non-parents (Table 1). Also, significantly fewer parents were in treatment with antipsychotic medication compared to non-parents (Table 1). Parents also had significantly higher personal and social performance scores (i.e. an estimate of daily functioning) in the previous month, and more parents were in remission of both negative and psychotic symptoms as well as in clinical recovery (Table 1). Finally, we found a higher self-reported quality of life among parents than non-parents (Table 1). When investigating global assessment scores of functioning, participants who had become parents after first diagnosis had, on average, a higher global function over 20 years than participants who had become parents before first diagnosis and non-parents (Fig. 2). When post hoc exploring participants who had become parents before first diagnosis, the majority were females (54%) and diagnosed with schizophrenia (65%) with a mean (s.d.) age of 32.8 (6.3) years at baseline compared to 25.4 (5.6) years for the rest of the clinical cohort. Also, when descriptively post hoc exploring gender differences, men without offspring, on average, had the lowest scores of global functioning followed by women without offspring, respectively, over 20 years (see Supplemental material eFig. 1).
Table 1. Clinical characteristics and longitudinal register-based data among parents and non-parents at the 20-year follow-up
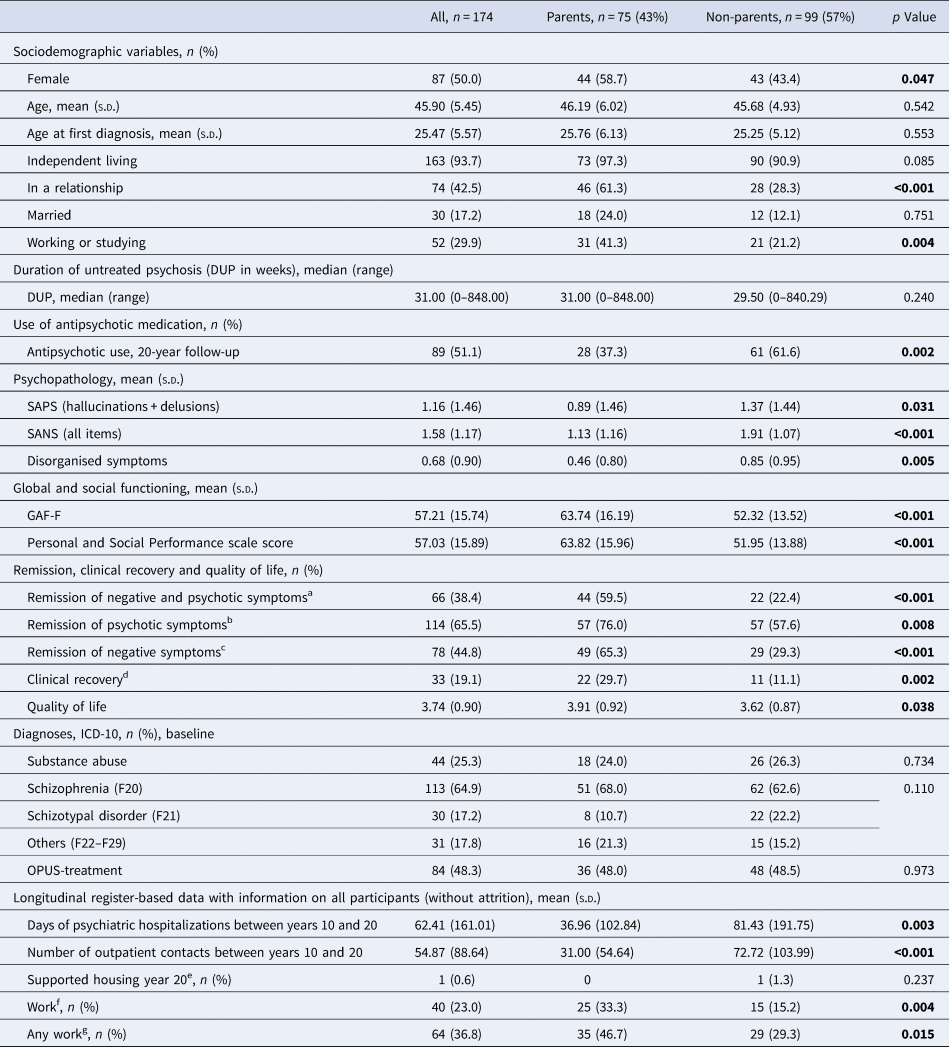
Abbreviations: GAF-F, Global Assessment of Functioning Scale; PAS, DUP, Duration of Untreated Psychosis; SAPS, scale for Assessment for Positive Symptoms; SANS, Scale for Assessment of Negative Symptoms; ICD-10, International Statistical Classification of Diseases, Tenth Revision, OPUS, two-year intensive early intervention program.
a Remission of psychotic and negative symptoms was defined as a score of 2 or less on all items on the Scale for Assessment for Positive Symptoms (SAPS) and Scale for Assessment of Negative Symptoms (SANS) for at least six months in accordance with the Remission in Schizophrenia Working Group.
b Remission of psychotic symptoms: defined as a score of 2 or less on all items on the Scale for Assessment of Positive Symptoms (SAPS) for at least six months in accordance with the Remission in Schizophrenia Working Group.
c Remission of negative symptoms: defined as a score of 2 or less on all items on the Scale for Assessment of Negative Symptoms (SANS) for at least six months in accordance with the Remission in Schizophrenia Working Group.
d Clinical recovery: defined as no psychotic episode, no psychiatric hospitalizations, and no supported accommodation for two consecutive years before follow-up, currently studying or working, and a GAF-F score of 60 or more.
e Use of supported housing facilities and homeless shelters at the previous year up to the 20-year follow-up.
f In full-time employment without supported employment benefits 50% of the past year before the 20-year follow-up.
g Full- or part-time employment (with/ without supported employment benefits) 50% of the past year before the 20-year follow-up.
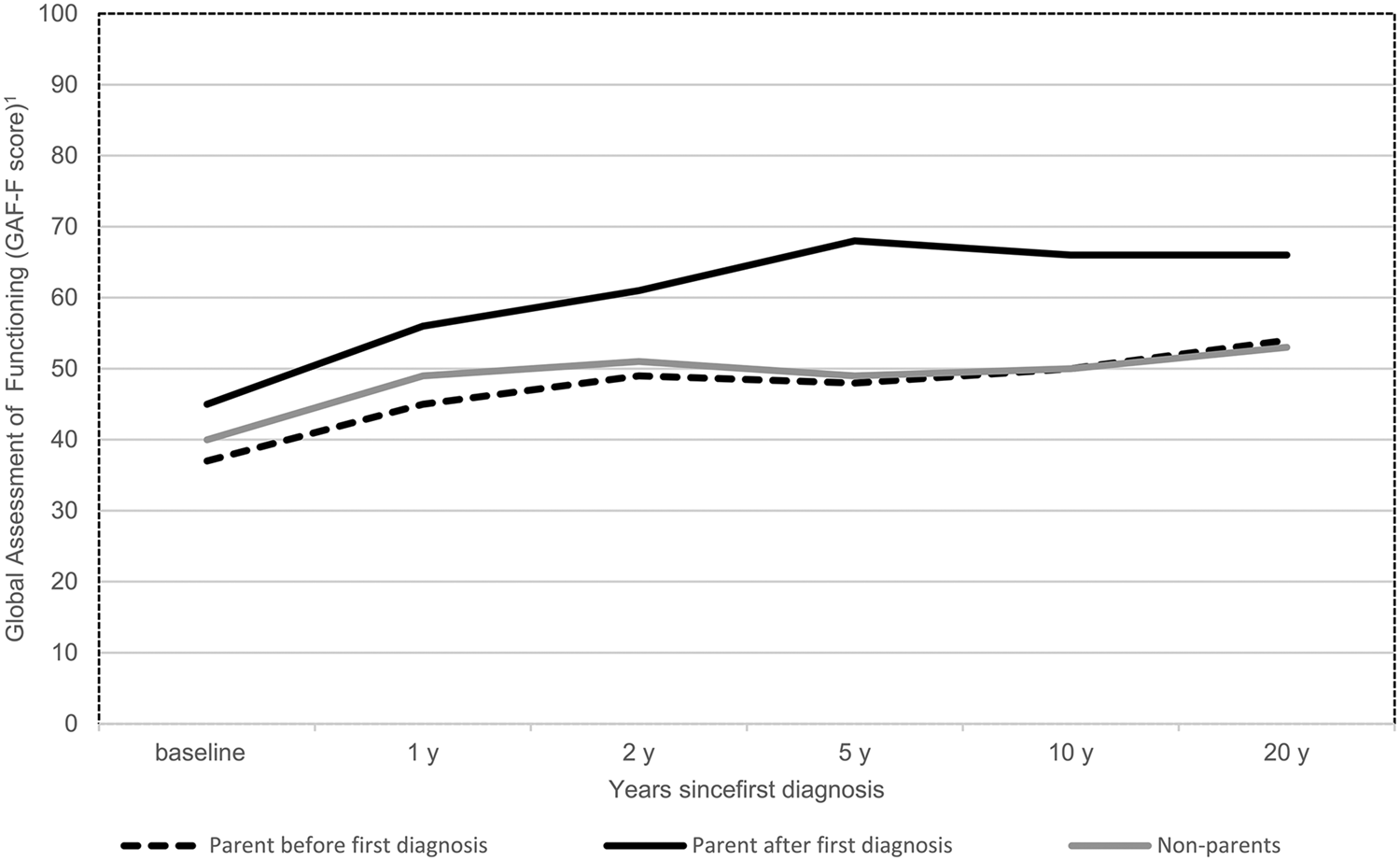
Figure 2. Global Assessment of Functioning (Functional scale) among parents before and after first diagnosis (i.e. onset of first-episode schizophrenia spectrum disorder) and non-parents over 20 years*.
*This figure is descriptive and stratifies between individuals who have become parents before first diagnosis and after and those without offspring (non-parents).
1 GAF-F, Global Assessment of Functioning scale ranging from 0 to 100 with higher scores indicating better global functional performance.
Register-based outcomes at the 20-year follow-up
Parents and non-parents at the 20-year follow-up also differed on longitudinal register data (Table 1). We found that parents had significantly fewer outpatient contacts between 10 and 20 years of follow-up and significantly fewer days of psychiatric hospitalizations than non-parents at the 20-year follow-up (Table 1). Also, regarding employment, more parents were in part- or full-time employment the last year before the 20-year follow-up (Table 1).
Clinical baseline characteristics of the participants at the 20-year follow-up
Looking retrospectively at the baseline demographics, those who had become parents at the 20-year follow-up, were more likely to be in a relationship or married than participants who had not become parents (See e Table 3 in the supplemental material). Those who had become parents also differed significantly on premorbid social adaptation and with higher psychotic symptoms at baseline than non-parents at the 20-year follow-up (eTable 3). At baseline, 68% of the parents were diagnosed with schizophrenia, 10.7% with schizotypal disorders, and 21.3% with other diagnoses within the schizophrenia spectrum, with no significant differences from those who have not become parents (Table 1).
Attrition at the 20-year follow-up
Significant differences in baseline characteristics were found between 20-year follow-up participants (n = 174) and non-participants (n = 404). Participants in follow-up were younger at study initiation, (p = 0.002), more females participated and more had completed high school compared to non-participants (See eTable 4 in the Supplemental material). Also, participants had lower negative and disorganized symptom scores (eTable 4). Participants also had a higher global functioning score and lower global symptom scores than non-participants (eTable 4).
For the entire cohort of 578 trial participants, no differences were found in psychiatric hospitalizations, number of outpatient contacts, and use of supported housing facilities between participating parents in the 20 years follow-up (n = 75) and non-participating parents (n = 144) as well as for participants without children and non-participants without children at the 20-year follow-up (eTable 5). Groups only differed in employment, where fewer non-participating parents were in part- or full-time employment the previous year before the 20-year follow-up compared to participating parents. (eTable 5). The same was found among participants without children and non-participants without children at the 20-year follow-up (eTable 5).
Evaluation of family functioning among families with children aged <18 years
Evaluating the global family functioning with the family assessment device, 14 families (28.6%) out of 49 had unhealthy family functioning (Table 2). When comparing parents in remission of psychotic and negative symptoms to parents in non-remission, no significant differences were found between the groups.
Table 2. Parental stress and general family functioning were reported by 75 parents with children (<18 years of age) living at home
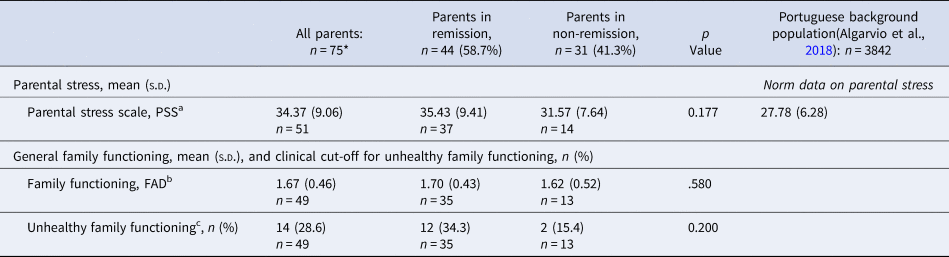
PSS, Parental Stress Scale; FAD, The general Functioning subscale of the Family Assessment Device.
Norm data, children aged 3–10 years.
a Parental stress scale with possible scores ranging from 18 to 90 and higher scores implying higher stress levels.
b The general functioning subscale of the family assessment device (FAD), lower scores implying better family functioning.
c A clinical cut-off score of ⩾ 2 equals unhealthy family functioning on the FAD.
*n: number of parents reporting on parental stress and general family functioning scales.
Evaluation of parental stress among parents with children aged < 18 years
A mean (s.d.) of 34.37 (9.06) was found on the Parental Stress Scale (18 items) for parents with children aged <18 years (Table 2). Furthermore, when comparing parents in remission of psychotic and negative symptoms to parents in non-remission, no significant differences were found between the groups.
Evaluation of the parent's impression of the mental health of children aged 4–16 years
Based on parents' evaluation of their child's/children's mental health with the Strengths and Difficulties Questionnaire (SDQ-DAN), varying difficulty scores were found between first-, second- and third-born children (Table 3). In total, a high difficulty score was detected for seven children (Table 3).
Table 3. Parent's impression of the mental health of children aged 4–16 years based on the parent version of the Strengths and Difficulties Questionnaire
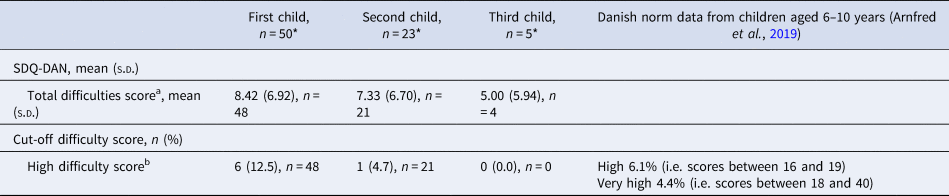
SDQ-DAN, The parent version of the Danish Strengths and Difficulties Questionnaire, includes five scales (i.e. prosocial scale, emotional problems scale, conduct problems scale, hyperactivity, and peer problems scale) with five items each,.
a The total difficulties score was generated by adding all the scales (except the prosocial scale) with scores ranging from 0 to 40.
b High difficulty score is defined by a cut-off point of ⩾17 on the total difficulty score.
*n: number of parents reporting the mental health of their children aged 4–16 years.
Discussion
A total of 219 (38%) individuals out of the 578 original clinical sample with first-episode schizophrenia spectrum disorders included in the OPUS trial between 1998 and 2000 had become parents to one or more children before the 20-year follow-up which is in line with previous estimates of parenthood (Campbell et al., Reference Campbell, Hanlon, Poon, Paolini, Stone, Galletly and Cohen2012; Radley et al., Reference Radley, Barlow and Johns2022a). From the clinical sample of 174 individuals assessed at the 20-year follow-up, 75 (43%) participants had become parents. Of these, 20 participants had already become a parent before the first diagnosis 20 years ago. In context, on average, 84% of the Danish background population had become parents to one or more children. Also, approximately 57% of the aged-matched Danish population were married compared to 17% in this clinical cohort (‘Statistikbanken – Data Og Tal,’ n.d.). Overall, parents assessed at the 20-year follow-up performed significantly better on several clinical outcomes than non-parents. They had significantly lower psychotic, negative, and disorganized symptom scores, and significantly more parents were in remission of both psychotic and negative symptoms and clinical recovery than non-parents, and they reported a significantly higher quality of life than non-parents at the 20-year follow-up. Furthermore, no significant differences between parents and non-parents regarding diagnoses within the schizophrenia spectrum were found. Interestingly, significantly more parents were not in treatment with antipsychotics compared to non-parents. Yet again, this might imply that illness course among parents is better and more favorable, despite no differences in diagnoses compared to non-parents. We might have expected that more individuals diagnosed with schizotypal disorders would have become parents, but in our study, they do not differentiate from those diagnosed with schizophrenia. Still, this finding could also be due to small numbers.
When descriptively investigating global functioning between parents before and after first diagnosis and non-parents over 20 years, the timing of becoming a parent was relevant. Participants who had become parents after first diagnosis scored above 60 on average on the Global Assessment of Functioning Scale, implying moderate to mild social, occupational, or school functioning difficulties. Participants who had become parents before first diagnosis scored, on average, less than 60, indicating moderate to severe impairments of functioning over 20 years compared to individuals who had become parents after first diagnosis. This demonstrates that those who had become parents after the first- episode of schizophrenia and most likely after psychosis treatment, on average, have more favorable outcomes than those who have become parents before and non-parents. When differentiating between genders, we found men without offspring to have the lowest global functioning over 20 years, followed by women without offspring. On average, individuals with offspring, regardless of gender, had equal global functioning at the 20-year follow.
Looking at baseline characteristics, significantly more females had become a parent, and more were in a relationship or married compared to non-parents. Participants who had become parents at the 20-year follow-up had significantly better premorbid social adaptation at baseline. Since premorbid social adaptation is associated with good outcomes by itself (Cole, Apud, Weinberger, & Dickinson, Reference Cole, Apud, Weinberger and Dickinson2012), we argue that those who become parents after first diagnosis may have better long-term outcomes simply because they have better premorbid functioning and are most likely also the ones with less severe illness course. This might imply that parenthood is probably not a predictor of positive long-term outcomes; rather, it is more likely that those who become parents after first diagnosis already had favorable outcomes. In prediction analysis on parenthood, we also found younger age, being in a relationship (i.e. married/having a partner), better premorbid social adaptation, and higher global functioning levels at baseline to be associated with becoming a parent, which is in line with the previous literature (Howard et al., Reference Howard, Kumar and Thornicroft2001; Radley et al., Reference Radley, Barlow and Johns2022a; Schrank, Moran, Borghi, & Priebe, Reference Schrank, Moran, Borghi and Priebe2015).
Several studies have investigated the living conditions of children born to parents with severe mental illness (Rasic, Hajek, Alda, & Uher, Reference Rasic, Hajek, Alda and Uher2014; Thorup et al., Reference Thorup, Jepsen, Ellersgaard, Burton, Christiani, Hemager and Nordentoft2015, Reference Thorup, Laursen, Munk-Olsen, Ranning, Mortensen, Plessen and Nordentoft2017), but few large-scale studies have examined the family-related outcomes among parents diagnosed with schizophrenia spectrum disorders. In our sample, 14 out of 49 parents (28.6%) reported unhealthy scores on the Family Assessment Device (FAD) (Miller et al., Reference Miller, Ryan, Keitner, Bishop and Epstein2000; Ridenour et al., Reference Ridenour, Daley and Reich1999; Staccini et al., Reference Staccini, Tomba, Grandi and Keitner2015). This suggests that having a family member diagnosed with schizophrenia spectrum disorders has an impact on family functioning. Also, unhealthy scores on FAD have been found to correlate with emotional stress and high burden among parents with schizophrenia (Staccini et al., Reference Staccini, Tomba, Grandi and Keitner2015). We would have suspected that parents in non-remission would report higher scores on the FAD. Surprisingly, no significant differences were found in family functioning, comparing parents in remission of psychotic and negative symptoms to parents in non-remission. When interpreting these results, we should be cautious due to the small sample size. Also, outcomes might be biased by self-report (Kristensen, Lauritzen, Handegård, & Reedtz, Reference Kristensen, Lauritzen, Handegård and Reedtz2023), indicating that parents in non-remission fear negative social consequences such as custody loss and fear of being judged or stigma, which has been well documented in several studies (Harries, Smith, Gregg, & Wittkowski, Reference Harries, Smith, Gregg and Wittkowski2023). Also, it might be hypothesized that parents with the fewest resources are the ones who most likely do not answer the parental questionnaires, generating missing data for those with the most unfavorable outcomes.
Also when evaluating parental stress among parents with children aged <18 years, a mean score of 34.37 was found on the Parental Stress Scale, with possible scores ranging from 18 to 90. A validation study of a Portuguese background population, including 3842 parents of children aged 3 to 10 years, found a mean score of 27.78 on the parental stress scale (Algarvio, Leal, & Maroco, Reference Algarvio, Leal and Maroco2018). This indicates that the parents in our sample tend to be moderately more stressed on average compared to a representable European general population of parents. Or since the children of the parents reporting parental stress in our sample were between 2 and 17 years of age, it might also imply that, on average, it is more stressful to be a parent to older children compared to minor children (i.e. age 3–10 years). Yet, again, we found no significant differences comparing parental stress scores among parents in remission of psychotic and negative symptoms to parents in non-remission. As previously discussed, these results should be interpreted cautiously due to self-report bias and self-stigma. Also, lack of parental self-awareness and poor insight should be considered when interpreting these results.
When evaluating parent's impression of mental health with the Strengths and Difficulties Questionaire of children aged 4–16 years, our results mirror those of the Danish High Risk and Resilience Study (VIA-7) (Spang et al., Reference Spang, Thorup, Ellersgaard, Hemager, Christiani, Burton and Plessen2022) reporting on high-risk children (aged seven years) of parents with schizophrenia and comparing these to matched children and their parents without mental disorders. The authors report significantly higher scores between the high-risk children and the matched control children on the total difficulty score as well as on the four difficulty scales (i.e. emotional problems scale, conduct problems scale, hyperactivity, and peer problems scale), indicating more daily life difficulties among children to parents with schizophrenia. If our study had had a matched control population, we would expect the same results as in the VIA-7 study. As of now, there are no official Danish norms for cut-off scores on the total difficulty scale, but in the background population, approximately 6% of Danish children aged 6–10 years had a high difficulty score ranging from 16 to 19 (Arnfred et al., Reference Arnfred, Svendsen, Rask, Jeppesen, Fensbo, Houmann and Bilenberg2019) and 4.4% of danish children had a very high difficulty score (i.e. scores between 18 and 40). In our sample, seven out of 69 children (10%) had a high difficulty score with a cut-off point of 17 or above. It is impossible to compare our results to those of the general population directly. Still, it might indicate that children in our sample do not experience more daily life difficulties than the Danish background children aged 6–10.
All of these results indicate that parents diagnosed with schizophrenia spectrum disorders have more favorable long-term outcomes than their counterparts without children (non-parents) as long as they have become parents after the first diagnosis. Still, parents experience possible challenges and difficulties regarding caregiving and parental stress, and a minority of their children face daily life difficulties potentially affecting their mental health and well-being.
In perspective, these results underline the importance of gaining a family-focused approach when forming interventions directed at parents with severe mental illness. Currently, there are very few evidence-based interventions focusing on improvement in parental caregiving abilities (Radley, Grant, & Barlow, Reference Radley, Grant and Barlow2021). However, convincing effects have been found from the recovery-oriented intervention ‘Let's talk about Children’ which is an add-on treatment offered with the standard treatment received by parents with mental illness (Reupert, Price-Robertson, & Maybery, Reference Reupert, Price-Robertson and Maybery2017). Of clinical implication, parental symptom decline is associated with improvement in parenting (Kahng et al., Reference Kahng, Oyserman, Bybee and Mowbray2008), and in addition to this, a recent network meta-analysis emphasized that almost all family interventions were superior in reducing psychotic relapse among individuals diagnosed with schizophrenia (Rodolico et al., Reference Rodolico, Bighelli, Avanzato, Concerto, Cutrufelli, Mineo and Leucht2022). Therefore, more qualitative studies are crucial to conduct to identify the possible challenges and needs of the parents when diagnosed with first-episode schizophrenia spectrum disorder (Wahl, Bruland, Bauer, Okan, & Lenz, Reference Wahl, Bruland, Bauer, Okan and Lenz2017). Individuals who are already parents at psychosis onset and their children should receive extra attention and continued support oriented in adult mental health services and thereby potentially enhance the well-being of both children and parents.
There are several shortcomings in the design of this study: widespread age of the children, different terms of living arrangements of the children, e.g., living at home, shared custody, foster care, institutionalized, etc. Reflecting on the representativity and attrition bias is crucial in long-term follow-up studies. In drop-out analyses, we found significant differences in baseline characteristics among participants at the 20-year follow-up and non-participants. Participants were younger, more females participated, and more had completed high school at baseline compared to non-participants. Also, participants had lower negative- and disorganized symptoms and were doing better in function and on symptom global assessment scores than non-participants at baseline. Due to this, we combined the clinical interview data with longitudinal register data (free of attrition) to investigate differences between participating and non-participating parents at the 20-year follow-up. Non-participating parents differed significantly, with fewer in part-time and full-time employment compared to participating parents. No significant differences were found in psychiatric hospitalizations, outpatient contacts, and use of supported housing facilities. Still, these findings imply that those with more favorable outcomes were more likely to participate in the 20-year follow-up. Also, results should be interpreted cautiously due to multiple cross-sectional comparisons between parents and non-parents. However, we find these results relevant in a family-related context. Since these associations are understudied among parents with schizophrenia spectrum disorders, we would rather report few false positives than miss out on important parental findings.
Conclusions
A total of 38% of individuals diagnosed with schizophrenia spectrum disorders had become parents at 20 years of follow-up. Compared to non-parents at the 20-year follow-up, parents did significantly better on several favorable outcomes, including global and social functioning, symptom severity, remission status, clinical recovery, and quality of life. Different timing of becoming a parent is crucial since participants becoming parents after a first diagnosis of schizophrenia spectrum disorder had better global functioning than participants becoming parents before first diagnosis
and non-parents. They also had significantly fewer outpatient contacts and psychiatric hospitalizations and were more often employed than non-parents. Still, parents with schizophrenia spectrum disorders face challenges, reflected by 28.6% of the parents reporting unhealthy family functioning and moderately more stress and by 10% of the children experiencing daily life difficulties.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291724000680
Acknowledgements
We thank our coworkers Lise Mariegaard, MSc (psychologist), Merete Birk, RN (nurse and research assistant), Heidi Dorthe Jensen (nurse and research assistant), and Nikolaj Kjær Høier (MscR Psychiatry), who were part of the clinical assessment team at the Research Unit of the Mental Health Centre and assessed the clinical interviews at 20-year follow-up. Finally, we are grateful to the trial participants who generously shared their personal stories and provided the clinical data in this study.
Author contributions
Carsten Hjorthøj, PhD, and Helene Gjervig Hansen, MD, had full access to all data in this study and took responsibility for the integrity of the data and the accuracy of the data analyses. Helene Gjervig Hansen designed the study and wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Funding statement
The project was funded by restricted grants from the Tryg Foundation (ID: 121654), Lundbeck Foundation, and Helse Fonden (ID: 19-B-0130). The sponsors had no role in acquiring the data, interpreting the results, or deciding to publish the findings.
Competing interests
The authors have none to report








