Introduction
Numerous psychopathological outcomes have been studied following trauma in children, including PTSD or acute stress disorder (ASD), depression, conduct and behavioral difficulties, separation anxiety, phobias, and generalized anxiety disorder (GAD). Research typically focuses on PTSD, with other psychopathology studied as comorbidities or secondary outcomes of PTSD (Goenjian et al., Reference Goenjian, Pynoos, Steinberg, Najarian, Asarnow, Karayan and Fairbanks1995). However, research in adults indicates that individuals may develop other disorders, such as phobias or depression, and not just PTSD symptoms (Ehring, Ehlers, & Glucksman, Reference Ehring, Ehlers and Glucksman2008; O'Donnell, Creamer, & Pattison, Reference O'Donnell, Creamer and Pattison2004).
In response to concerns that PTSD doesn't encapsulate the full extent of reactions to more repeated or severe forms of trauma exposure, the 11th edition of the International Classification of Diseases (ICD-11) included ‘complex PTSD’ (CPTSD) as a new diagnosis. To meet criteria for a CPTSD diagnosis, in addition to the core PTSD criteria (re-experiencing, avoidance, and perceived threat), three CPTSD-specific symptom clusters known as disturbances in self-organization (DSO) must be met: affect dysregulation, negative self-concept, and interpersonal difficulties. Childhood interpersonal trauma is a risk factor for developing CPTSD compared to PTSD, with a dose-response type relationship where exposure to multiple forms of interpersonal trauma increases risk of CPTSD (Hyland et al., Reference Hyland, Murphy, Shevlin, Vallieres, McElroy, Elklit and Cloitre2017a). However, it has been argued that CPTSD can develop in response to a single traumatic stressor (Maercker et al., Reference Maercker, Brewin, Bryant, Cloitre, van Ommeren, Jones and Reed2013); multiple traumas may therefore be best conceptualized as a risk factor, rather than a requirement, for CPTSD (Hyland et al., Reference Hyland, Shevlin, Elklit, Murphy, Vallieres, Garvert and Cloitre2017b; Sachser, Keller, & Goldbeck, Reference Sachser, Keller and Goldbeck2017).
Most research has focused on confirming CPTSD as a valid diagnosis and distinct from PTSD in adults (Cloitre, Garvert, Brewin, Bryant, & Maercker, Reference Cloitre, Garvert, Brewin, Bryant and Maercker2013; Cloitre, Garvert, Weiss, Carlson, & Bryant, Reference Cloitre, Garvert, Weiss, Carlson and Bryant2014; Elklit, Hyland, & Shevlin, Reference Elklit, Hyland and Shevlin2014; Knefel & Lueger-Schuster, Reference Knefel and Lueger-Schuster2013; Knefel, Garvert, Cloitre, & Lueger-Schuster, Reference Knefel, Garvert, Cloitre and Lueger-Schuster2015; Perkonigg et al., Reference Perkonigg, Hofler, Cloitre, Wittchen, Trautmann and Maercker2016). Two studies have validated CPTSD in children and adolescents (Perkonigg et al., Reference Perkonigg, Hofler, Cloitre, Wittchen, Trautmann and Maercker2016; Sachser et al., Reference Sachser, Keller and Goldbeck2017).
Ehring et al. (Reference Ehring, Ehlers and Glucksman2008) highlighted the need to investigate predictors differentiating between the development of various psychopathological presentations following trauma. They demonstrated the utility of cognitive theories of emotional disorders in differentiating between PTSD, travel phobia, and depression in adults following motor-vehicle accidents. To date, no study has utilized similar methodology to assess predictive models in understanding the risk factors of youth developing psychopathology following trauma.
Models and predictors of PTSD and CPTSD
The evidence available for psychosocial predictors of PTSD in children is variable, with meta-analyses indicating the need for further assessment. Social support, prior life events, low intelligence, socioeconomic status, low self-esteem, and female gender were shown as consistent predictors of PTSD, but with only small to medium effect sizes, and younger age was found not to be a predictor of PTSD in youth (Cox, Kenardy, & Hendrikz, Reference Cox, Kenardy and Hendrikz2008; Trickey, Siddaway, Meiser-Stedman, Serpell, & Field, Reference Trickey, Siddaway, Meiser-Stedman, Serpell and Field2012).
Various psychosocial risk factors are considered in relation to adult CPTSD, including multiple prior traumas, interpersonal traumas, and interpersonal stressful life events (Herman, Reference Herman, Everly and Lating1995; Hyland et al., Reference Hyland, Murphy, Shevlin, Vallieres, McElroy, Elklit and Cloitre2017a), but research assessing these as CPTSD predictors is limited. Exposure to child abuse and multiple types of abuse increases an adult's likelihood of CPTSD v. PTSD (Cloitre et al., Reference Cloitre, Garvert, Brewin, Bryant and Maercker2013; Powers et al., Reference Powers, Fani, Carter, Cross, Cloitre and Bradley2017). In youth, female gender and interpersonal trauma predict CPTSD v. PTSD (Sachser et al., Reference Sachser, Keller and Goldbeck2017).
Ehlers and Clark (Reference Ehlers and Clark2000), Foa, Steketee, and Rothbaum (Reference Foa, Steketee and Rothbaum1989), and Brewin, Dalgleish, and Joseph (Reference Brewin, Dalgleish and Joseph1996) proposed cognitive models of PTSD in which trauma memories and associated cognitive processes are key. Poor social support, prior or ongoing trauma, aversive secondary emotions, trauma severity, and prior psychopathology are risk factors to inhibition of adaptive processing of trauma memories, and thus PTSD.
The predictive power of the cognitive model has been demonstrated in children experiencing road traffic accidents (RTAs); 53–65% of the variance in PTSD symptoms was predicted by models including data-driven processing, negative appraisals of the trauma, rumination, and thought suppression (Ehlers, Mayou, & Bryant, Reference Ehlers, Mayou and Bryant2003; Meiser-Stedman, Dalgleish, Glucksman, Yule, & Smith, Reference Meiser-Stedman, Dalgleish, Glucksman, Yule and Smith2009a; Stallard & Smith, Reference Stallard and Smith2007). Cognitive models are also thought to be disorder specific in predicting the psychopathology outcomes of experiencing a trauma; despite overlaps in symptoms and risk factors across PTSD, depression, and other anxiety disorders, cognitive factors differentiate whether an individual may develop one disorder presentation over another (Ehring et al., Reference Ehring, Ehlers and Glucksman2008). For example, poor trauma memory quality is likely to be mostly strongly associated with PTSD over depression or anxiety, and safety-seeking behaviors are thought to be present for PTSD and anxiety but not for depression. Other key cognitive mechanisms such appraisals and rumination may be strongly related to both PTSD and depression. However, data from adult studies is supportive of a role for disorder-specific content for each process: PTSD is more associated with trauma-specific appraisals (perceiving intrusive memories as a sign of permanent psychological damage) and rumination (asking why the trauma happened, what might have been done differently), while depression is more associated with mood-specific appraisals (such as perceptions of worthlessness) and rumination (a persistent focus on the reasons why someone might have low mood) (Beierl, Böllinghaus, Clark, Glucksman, & Ehlers, Reference Beierl, Böllinghaus, Clark, Glucksman and Ehlers2020; Ehring et al., Reference Ehring, Ehlers and Glucksman2008; Kleim, Ehlers, & Glucksman, Reference Kleim, Ehlers and Glucksman2012). The identification of such processes has implications for treatment, e.g. the importance of memory processing (through techniques such as imaginal reliving, in vivo or elaborating a trauma narrative) for the successful treatment for PTSD and the need to address mood-related rumination for the treatment of depression.
Both objective and subjective appraisals of event severity have been researched, with poor differentiation and little consistency in what constitutes markers of severity (Trickey et al., Reference Trickey, Siddaway, Meiser-Stedman, Serpell and Field2012). Recent research demonstrates that markers of event severity may include: interpersonal (v. non-interpersonal) trauma; the event resulting in a death; injury severity; levels of pain; and peritraumatic dissociation, perceived threat, fear, and panic responses (Cox et al., Reference Cox, Kenardy and Hendrikz2008; Ozer, Best, Lipsey, & Weiss, Reference Ozer, Best, Lipsey and Weiss2003; Saxe et al., Reference Saxe, Stoddard, Hall, Chawla, Lopez, Sheridan and Yehuda2005; Trickey et al., Reference Trickey, Siddaway, Meiser-Stedman, Serpell and Field2012; Vogt, King, & King, Reference Vogt, King, King, Friedman, Keane and Resick2007).
Aims of the current study
There have been few studies comparing predictive models across psychopathological outcomes of trauma, and none focused on youth. This, alongside the addition of CPTSD as a diagnostic category, warrants exploration of predictors of psychopathological outcomes of trauma-exposed youth.
The present study used data collected from a prospective longitudinal study of PTSD in children and adolescents following a recent trauma. Data pertaining to the course of DSM-IV, DSM-5, ICD-10, and ICD-11 PTSD and CPTSD has been reported (Elliott et al., Reference Elliott, McKinnon, Dixon, Boyle, Murphy, Dahm and Hitchcock2021; Meiser-Stedman et al., Reference Meiser-Stedman, McKinnon, Dixon, Boyle, Smith and Dalgleish2017), as has data regarding the trajectory of PTSD symptoms (Meiser-Stedman et al., Reference Meiser-Stedman, Mckinnon, Dixon, Boyle, Smith and Dalgleish2019). The present study aimed to identify risk factors for PTSD, CPTSD, depression, and anxiety at follow up. Specifically, the goodness of fit of predictive models of PTSD and CPTSD in youth, in comparison to depression and anxiety, were assessed, and predictors of these disorders explored. Predictive models were developed based on psychosocial factors, cognitive factors, subjective event severity, and objective event severity factors.
Hypotheses
Firstly, it was hypothesized that peri- and post-trauma factors would be greater predictors of PTSD and CPTSD than pre-trauma psychosocial factors. Secondly, it was hypothesized that the cognitive model would have the best model fit in predicting PTSD and CPTSD. Finally, it was hypothesized that the cognitive model would have more power than other models in differentiating between PTSD, CPTSD, depression, and anxiety as trauma outcomes in youth.
Methods
Participants
Two hundred and sixty 8–17-year-olds were consecutively recruited from four Emergency Departments (ED) in the East of England between September 2010 and April 2013, who were identified by research nurses as presenting due to a single event trauma (e.g. a motor vehicle collision or assault), defined in accordance with DSM-V criteria (American Psychiatric Association, 2013), i.e. ‘exposure to actual or threatened death, serious injury, or sexual violence’.
Staff identified 774 eligible children; 168 (21.7%) could not be contacted; of 605 families contacted, 315 (52%) did not wish to participate, 30 (5%) did not meet eligibility criteria, and 260 (43%) agreed to participate. Initial assessments at two weeks post-trauma (T1) were completed by 226 participants, and 234 completed the assessment at nine weeks post-trauma (T2), with 260 participating in at least one timepoint. There were no significant differences between responders and non-responders on age, gender, ethnicity, or measures of injury severity and hospital treatment. However, responders were more likely than non-responders to experience more pain, admission to hospital, and to have experienced an assault (v. other) trauma (Meiser-Stedman et al., Reference Meiser-Stedman, McKinnon, Dixon, Boyle, Smith and Dalgleish2017).
Inclusion criteria were: exposure to a single discrete traumatic stressor defined in accordance with DSM-V criteria. Exclusion criteria were: intellectual disability; non-fluency in English; unconsciousness longer than 15 min following the event; a history of brain damage or moderate to severe traumatic brain injury as a result of the trauma; assaults involving a caregiver/close relative as the assailant; ongoing exposure to threat; any significant risk of self-harm or A&E attendance resulting from deliberate self-harm; being under the care of social services or a child protection issue related to the presentation; any current symptoms of PTSD following a previous trauma; unable to gain consent from parent/guardian. No participants were excluded based on their presentation being due to ongoing trauma. See online Supplementary Table S1 for data pertaining to the number of young people excluded based on each exclusion criterion.
Measures
Self-report questionnaires and structured interviews were completed by parents and children two weeks post-trauma and hospital data was gathered by nurses in the ED at point of admission. See online Supplementary Table S2 for a summary of measures.
Psychosocial factors
Participant demographic data were collated with admission information from the hospital, including trauma type and injury characteristics. Parents' education level was categorized as those achieving up to GCSE or equivalent and those achieving higher education or training. Parents were asked about prior traumas experienced over their child's lifetime and life stressors over the past year using a list of possible events (see online Supplementary Table S3) taken from the Posttraumatic Diagnostic Scale (PDS-5; Foa, Cashman, Jaycox, & Perry, Reference Foa, Cashman, Jaycox and Perry1997; Foa et al., Reference Foa, McLean, Zang, Zhong, Powers, Kauffman and Knowles2016); total number of prior traumas and life stressors were used as putative predictor variables. Prior poor well-being was identified by parents answering positively to: ‘Before the trauma, have you had concerns for your child's emotional well-being (e.g. anxiety, depression, or emotional problems)?’. Children's perception of their social support and quality of their relationships was assessed using a self-report questionnaire, the Multidimensional Scale of Perceived Social Support (MSPSS: Zimet, Dahlem, Zimet, & Farley, Reference Zimet, Dahlem, Zimet and Farley1988; Cronbach's α = 0.93).
Cognitive factors
The cognitive model included cognitive processing during the trauma (Children's Data-Driven Processing Questionnaire [CDDPQ]: McKinnon, Nixon, & Brewer, Reference McKinnon, Nixon and Brewer2008; Cronbach's α = 0.89); negative trauma-related appraisals (Child Post-traumatic Cognitions Inventory [CPTCI]: Meiser-Stedman et al., Reference Meiser-Stedman, Dalgleish, Glucksman, Yule and Smith2009a; Cronbach's α = 0.95); trauma memory quality (Trauma Memory Quality Questionnaire [TMQQ]: Meiser-Stedman, Smith, Yule, & Dalgleish, Reference Meiser-Stedman, Smith, Yule and Dalgleish2007; Cronbach's α = 0.83); post-traumatic dissociation (four-item questonnaire; Cronbach's α = 0.78); trauma-related rumination (three-item scale, Cronbach's α = 0.77); and self-blame (two-item scale, with Cronbach's α = 0.91; Meiser-Stedman et al., Reference Meiser-Stedman, McKinnon, Dixon, Boyle, Smith and Dalgleish2017).
Subjective event severity
This model focused on peritraumatic processes, including: panic responses (Child Peritraumatic Panic scale (CPP): Meiser-Stedman et al., Reference Meiser-Stedman, McKinnon, Dixon, Boyle, Smith and Dalgleish2017; Cronbach's α = 0.72); peritraumatic dissociation (four-item questionnaire; Cronbach's α = 0.67); and three items entered individually assessing peritraumatic perceived threat and fear (Meiser-Stedman et al., Reference Meiser-Stedman, Dalgleish, Glucksman, Yule and Smith2009a, Reference Meiser-Stedman, Smith, Bryant, Salmon, Yule, Dalgleish and Nixon2009b; Cronbach's α = 0.76).
Objective event severity
This model used information gathered from the child's presentation at the ED including the number of injuries sustained, whether they had sustained a head injury, whether they were given opiate pain-relief in ED, and whether they were admitted to hospital. The child's rating of pain during the event was included (‘How much pain were you in at the time of the accident?’ with Likert responses on a four-point scale).
Assessment of outcomes
Outcomes were assessed at nine weeks post-trauma. PTSD symptoms were assessed using items from the Child PTSD Symptoms Scale (CPSS; Foa, Johnson, Feeny, & Treadwell, Reference Foa, Johnson, Feeny and Treadwell2001). CPTSD DSO (disturbances of self-organization) symptoms were assessed using items drawn from the CPSS, the CPTCI (Meiser-Stedman et al., Reference Meiser-Stedman, Smith, Bryant, Salmon, Yule, Dalgleish and Nixon2009b) and the self-blame questionnaire items (Meiser-Stedman et al., Reference Meiser-Stedman, McKinnon, Dixon, Boyle, Smith and Dalgleish2017), with PTSD and CPTSD diagnoses following the ICD-11 criteria derived from these; a symptom was present if the corresponding item scored one or higher (once per week or more, Sachser et al., Reference Sachser, Keller and Goldbeck2017). Continuous measures for these outcomes were also derived: a nine-item PTSD measure from the CPSS (possible score range 0–27) and an eight-item CPTSD-DSO measure using items from the CPSS, CPTCI, and self-blame items (possible score range 0–24), excluding core PTSD symptoms to prevent multicollinearity. The internal consistency was Cronbach's α = 0.90 and 0.78 for the PTSD and CPTSD-DSO scales, respectively. The PTSD scale score showed good correlation (Pearson's correlation coefficient = 0.61) with a diagnostic measure of DSM-IV PTSD, assessed by the Children's PTSD Inventory (Saigh et al., Reference Saigh, Yasik, Oberfield, Green, Halamandaris, Rubenstein and McHugh2000) semi-structured interview. The correlation between the PTSD scale and the CPTSD-DSO scale was 0.63. Full diagnostic criteria were used to identify frequencies of likely PTSD and CPTSD diagnoses at week nine. See online Supplementary Table S4 for item list and construct derivation.
The Short Mood and Feelings Questionnaire (SMFQ, Angold, Costello, Messer, & Pickles, Reference Angold, Costello, Messer and Pickles1995; Cronbach's α = 0.92) was used to assess depression symptoms, with a score of 8 or above indicating ‘likely depression’. The Spence Children's Anxiety Scale (SCAS; Spence, Reference Spence1998) Generalised Anxiety Disorder (GAD) subscale (Cronbach's α = 0.87) was used to assess GAD symptoms, with computed t scores above 60 indicating ‘likely GAD’. These are well-validated measures in children and adolescents (Sharp, Goodyer, & Croudace, Reference Sharp, Goodyer and Croudace2006; Spence, Barrett, & Turner, Reference Spence, Barrett and Turner2003).
Study procedure
The study was approved by the UK National Research Ethics Service, Cambridgeshire 1 Research Ethics Committee (10/H0304/11). Participants were recruited after presenting at an ED; parents/caregivers of children who met eligibility criteria were contacted by letter enclosing information sheets and contacted by telephone one week after ED attendance. Informed consent from the parent and assent from the child was gained if eligibility criteria were met. Approximately two weeks following their trauma (T1), participants and parents were interviewed via telephone and asked to complete self-report questionnaires. Participants were assessed a second time approximately nine weeks post-trauma (T2), with the same interview and self-report measures.
Analyses
Data processing and analysis was completed in Stata/IC Version 13.1 (StataCorp, Reference Statacorp2013) and R 4.3.1, including the use of the simpleboot package (Peng, Reference Peng2019). Missing data codes were assigned to ensure correct treatment of missing data by Stata. Stata uses complete case analysis by default (observations with any missing data are excluded), which is a valid method of treating missing data if it is deemed ‘missing at random’ (MAR) and if data missingness is independent of the outcome of interest. Due to different numbers of participants at each timepoint, many observations were ‘missing’ in the predictor or outcome variables. Data available from ED admissions were also variable. t tests were run to confirm no significant differences in outcome measures between participants with missing and complete data and there were no significant differences between complete cases and non-complete cases across both time points. Therefore, complete case analysis was deemed valid. Some differences in the model goodness of fit statistics may have partially reflected the different number of observations included in the analysis.
Pre-analysis screening of the normality, skew, and homoscedasticity of the data was completed. Many variables were skewed, residuals were not normally distributed, and the variance of residuals was heteroscedastic, violating parametric test assumptions, therefore non-parametric or other appropriate considerations were made.
Spearman's rank correlation coefficients (rho) were used to ascertain association strength between all continuous variables, and point biserial correlation coefficients were computed for dichotomous variables to identify correlations between predictor variables and outcome variables and identify any multicollinearity between predictor variables. For predictive model analysis, non-parametric adjustments were made to multiple linear regression models using bootstrapping, allowing for estimation of coefficients and standard errors (Chernick, Reference Chernick2008). To generate standardized coefficients, variables were transformed into standardized formation, and the regression was re-run to generate a beta coefficient equivalent (Acock, Reference Acock2008). Both unstandardized and standardized coefficients are reported.
The predictive power and goodness of fit of the predictor models were compared by computing Akaike and Bayesian Information Criteria (AIC and BIC) and adjusted R-squared values. Low AIC and BIC values indicate better model fit, and higher R 2 values indicate a greater proportion of variance accounted for by the predictor variables (Akaike, Reference Akaike, Parzen, Tanabe and Kitagawa1998; Raftery, Reference Raftery1995).
Statistical power
N > / = 50 + 8 m (where m = number of predictors) was used to calculate the required sample size for a reasonably powered multiple regression analysis (Green, Reference Green1991). For seven predictor variables, 106 participants would be required. To detect a large effect size with seven predictor variables and a power of 0.8 (alpha = 0.05) using a parametric multiple correlation analysis, 44 participants are required, and to detect a medium effect size, 103 participants are required (Green, Reference Green1991). A minimum of 189 participants were included in the analyses and no more than seven predictor variables were used in each model.
Results
Sample characteristics
Of the 260 participants, 118 (45%) had experienced a road traffic collision, 43 (17%) an assault, 82 (32%) an accidental injury, 15 (6%) a dog attack, and 2 (1%) had an acute medical emergency. Sample characteristics including age (mean 13.9 years), gender (43.5% female), psychosocial features, trauma characteristics, and predictor and outcome variables are summarized in Table 1.
Table 1. Correlations between week two predictor variables and outcomes at week nine post trauma

Note. *p < 0.05, **p < 0.01, ***p < 0.001.
At nine weeks post-trauma, 55 (23.5%) participants met criteria for PTSD, 20 (8.5%) exhibited CPTSD DSO (disturbances of self-organization) symptoms, and 12 (5.2%) met criteria for full CPTSD, according to the measures generated in accordance with ICD-11 criteria (See online Supplementary Table S5). Fifty-six individuals (23.9%) scored highly on the SMFQ to indicate likely depression, and 25 (10.7%) scored highly on the SCAS subscale to indicate likely GAD (see Fig. 1). The requirement for core PTSD symptoms alongside DSO symptoms to meet CPTSD diagnostic criteria meant that, by definition, no participants would fall into the ‘CPTSD only’ category. Eighty-four participants (36%) met the threshold for at least one of the four diagnoses at T2.
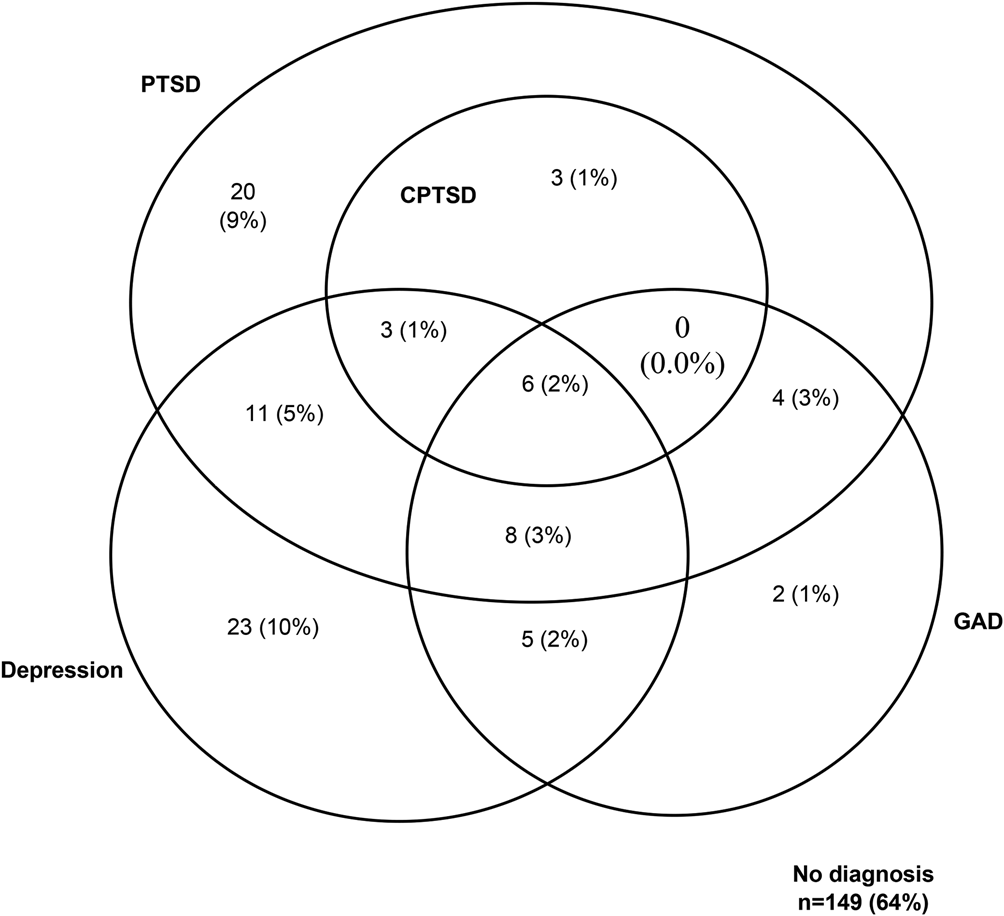
Fig. 1. Venn diagram summarizing number of participants meeting criteria for likely diagnoses of PTSD, CPTSD, depression, and GAD at nine weeks post-trauma.
Correlates of psychopathology
The correlation statistics between T1 putative predictor variables and the four T2 outcome variables are displayed in Table 1. Cognitive variables and subjective event severity factors showed the highest correlations with the four psychopathology outcome variables. Trauma memory qualities and trauma-related appraisals were the highest correlated of the predictor factors with PTSD (rs = 0.58). Appraisals and rumination were the highest correlated factors with CPTSD (rs > 0.46). Depression and GAD scores were also most highly correlated with trauma-related appraisals and rumination (rs > 0.55).
Predictors of PTSD
The psychosocial model was significant and accounted for 5.4% of the variance in PTSD symptom severity (adjusted R 2 = 0.054; see Table 2 for all model fit statistics), with female gender (β = 0.14) and interpersonal index trauma (β = 0.26) as significant predictors (see online Supplementary Table S6). The objective event severity model was significant and accounted for the smallest variance (adjusted R 2 = 0.03) in PTSD symptom severity of all four models, with pain being the only significant predictor (β = 0.21). The subjective event severity model accounted for 33% of variance (adjusted R 2 = 0.33); panic (β = 0.37), feeling scared (β = 0.15) and dissociation (β = 0.23) during the trauma were significant predictors of PTSD. The cognitive model accounted for the greatest variance in PTSD symptom severity (adjusted R 2 = 0.55); greater post-traumatic dissociation (β = 0.17), poorer trauma memory quality (β = 0.20) and maladaptive appraisals of the trauma (β = 0.33) were associated with increased PTSD symptoms. See Table 3 for summary of variables accounting for unique variance in PTSD and the other three outcomes.
Table 2. Overall goodness of fit and model statistics for multiple linear regression analyses of predictors of each disorder

SES, Subjective event severity; OES, Objective event severity. Model with fit indices suggesting the best goodness of fit and highest variance in outcome accounted for highlighted in bold. N observations included in each model analysis varied as such: psychosocial n = 194; cognitive n = 201; SES n = 202; OES n = 189.
Table 3. Variables accounting for unique variance for each outcome
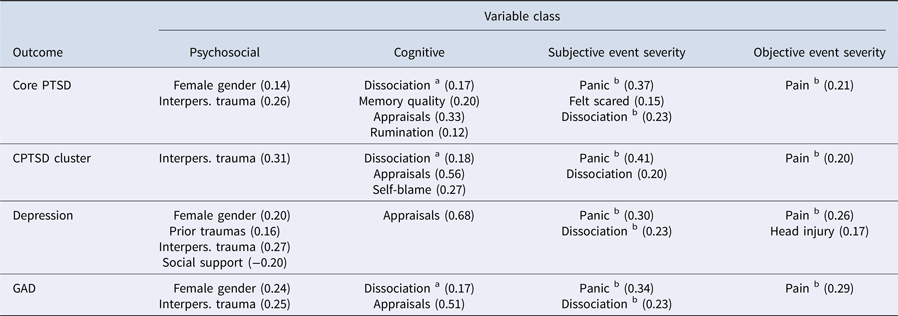
Note. aOngoing; b Peri-traumatic. Standardized regression (i.e. beta) coefficients are displayed in parentheses.
Predictors of CPTSD
The psychosocial model was significant and accounted for greater (13%) variance in DSO symptom severity (adjusted R 2 = 0.13) than PTSD (see online Supplementary Table S7). Experiencing interpersonal index trauma (β = 0.31) was associated with increased DSO symptoms. Within the subjective event severity model, panic (β = 0.41) and dissociation (β = 0.20) were significant predictors of later DSO symptoms; this model again accounting for greater variance (adjusted R 2 = 0.29) than the objective model (adjusted R 2 = 0.04), where only pain (β = 0.20) accounted for unique variance. A large proportion of variance was accounted for by the cognitive model (adjusted R 2 = 0.59), with post-traumatic dissociation (β = 0.18), maladaptive appraisals (β = 0.56) and self-blame (β = 0.14) acting as significant predictors.
Predictors of depression
Female gender (β = 0.20), prior traumas (β = 0.16), interpersonal index trauma (β = 0.27), and poorer perceived social support (β = −0.20) were significant predictors of later depression in the psychosocial model (adjusted R 2 = 0.13; see online Supplementary Table S8). Within the cognitive model, only increased maladaptive trauma appraisals was a significant predictor of later depression symptoms, with a large coefficient (β = 0.68), but the model still accounted for 56% of the variance in depression at week nine (adjusted R 2 = 0.56). Panic (β = 0.30) and dissociation during the trauma (β = 0.23) were significant predictors within the subjective event severity model (adjusted R 2 = 0.24); pain (β = 0.26) and sustaining a head injury (β = 0.17) were significant predictors within the objective event severity model (adjusted R 2 = 0.08).
Predictors of GAD
Female gender (β = 0.24) and experiencing an interpersonal index trauma (β = 0.25) significantly predicted later GAD symptoms in the psychosocial model (adjusted R 2 = 0.13; see online Supplementary Table S9). The cognitive model showed strong predictive power (adjusted R 2 = 0.56), with trauma appraisals (β = 0.51) and dissociation (β = 0.17) significant predictors. The subjective event severity model accounted for the second greatest amount of variance in symptoms (adjusted R 2 = 0.28), with panic (β = 0.34) and peritraumatic dissociation (β = 0.23) as significant predictors. Within the objective event severity model (adjusted R 2 = 0.09), increased pain was a significant predictor of GAD symptom severity (β = 0.29).
Overall model comparisons
Table 2 summarizes the goodness of fit statistics for each model predicting each disorder. Each model was significant. The cognitive model consistently accounted for the greatest variance in symptoms and achieved the best (lowest) AIC and BIC statistics. The subjective event severity model was consistently the second best-fitting model, followed by the psychosocial model. Comparison across disorders indicates that the psychosocial model was comparably stronger in predicting CPTSD, depression, and GAD but weaker in predicting PTSD. The subjective event severity model was stronger in predicting core PTSD and weakest in predicting depression, and the objective model was comparable in predicting depression and GAD but weakest in predicting core PTSD.
Sensitivity analyses
Further models were evaluated to confirm the robustness of our findings. Given the strong relationship between exposure to interpersonal violence and PTSD (Alisic et al., Reference Alisic, Zalta, Van Wesel, Larsen, Hafstad, Hassanpour and Smid2014), the cognitive, subjective event severity, and objective event severity models were re-run, but with interpersonal index event also included in the model. The addition of interpersonal index did not add more than 2% additional variance explained to any of the cognitive models. An additional 5% of variance was accounted for when adding interpersonal violence to the subjective event severity model for CPTSD, but for other outcomes there was only 2–3% variance accounted for. The objective event severity models were improved by 2–8%, with the model for CPTSD the most strongly improved (see online Supplementary Table S10 for revised model fit statistics). Interpersonal index event accounted for unique variance in several models (the objective and subjective event severity models for PTSD, depression and GAD; all revised CPTSD models); moreover, no variables that previously accounted for unique variance lost their significance, with the exception of head injury in the objective event severity model for depression (see online Supplementary Tables S11–S14).
Further models were run to evaluate whether the cognitive model was as robust even when psychosocial processes were included in the same model. Adding psychosocial processes to the cognitive model did not increase the proportion of variance explained by more than 2% for each outcome (see online Supplementary Table S10); moreover, no cognitive variables that previously accounted for unique variance in an outcome ceased to do so (see online Supplementary Tables S15–S18). The same process was repeated but entering the subjective event severity variables alongside the cognitive variables. These models did not account for much additional variance compared to the cognitive variables alone model (see online Supplementary Table S10); the cognitive variables that previously accounted for unique variance continued to do so (see online Supplementary Tables S19–S22).
Discussion
Overall findings
In youth exposed to single event trauma, longitudinal models comprising peri- and post-traumatic factors were more powerful predictors of all mental health outcomes than the psychosocial model (primarily pre-trauma factors) at a two month follow up assessment. The cognitive model provided the best model fit for PTSD and CPTSD, and cognitive factors were more powerful predictors than event-related measures. These findings were consistent with our first two hypotheses. However, the cognitive model also derived the best model fit over other models for depression and GAD; this generalized power did not support hypothesis three (that the cognitive model would differentiate between disorders). Overall, poor disorder specificity was indicated, with a similar pattern of goodness of fit indices and some overlap in significant predictors of disorders.
Understanding CPTSD in children
As a relatively new diagnosis, there are few studies of CPTSD in youth. This study provides some evidence for PTSD and CPTSD being related but distinct presentations in youth, with different predictors and correlates. Trauma memory quality and rumination were not related to CPTSD symptoms in our regression models but were related to PTSD; self-blame accounted for unique variance on CPTSD but not PTSD. Theories of CPTSD have referred to the role of disruption of attachments which leads to the DSO symptoms (Cloitre et al., Reference Cloitre, Stolbach, Herman, van der Kolk, Pynoos, Wang and Petkova2009). This was not supported in our data, however; while social support was modestly negatively correlated with CPTSD symptoms (i.e. a potential protective effect) social support did not play a role in our regression model of CPTSD. Female gender and prior poor well-being were not found to be predictive of CPTSD in our regression model, in contrast to previous research (e.g. Sachser et al., Reference Sachser, Keller and Goldbeck2017), although this may be due to features of the sample or the well-being measure.
The predictive power of the cognitive model
The cognitive model of predictors based on Ehlers and Clark's (Reference Ehlers and Clark2000) model of PTSD demonstrated the best model fit indices and greatest proportion of variance accounted for in PTSD, CPTSD, depression, and GAD. Maladaptive appraisals of a traumatic event were a strong cognitive predictor of all disorders, but variation in the significance and strength of other cognitive predictors highlighted some differentiation in the predictive power and applicability of this model to different disorders. For example, all cognitive factors had significant or near to significant roles in predicting greater likelihood of ‘core’ PTSD symptoms, whereas data-driven processing, trauma memory quality, and rumination had no effect in predicting CPTSD symptoms; moreover, self-blame was only related to CPTSD symptoms. This finding supports the validity of ‘core’ and ‘complex’ PTSD as distinct presentations and the use of cognitive behavioral therapy to effectively treat a range of diagnoses experienced by young people (Jensen et al., Reference Jensen, Holt, Ormhaug, Egeland, Granly, Hoaas and Wentzel-Larsen2014; Rith-Najarian et al., Reference Rith-Najarian, Mesri, Park, Sun, Chavira and Chorpita2019). Similarly, only greater trauma-related misappraisals were significantly predictive of depression and GAD. Interestingly, rumination appeared to have the most relevance as a predictive factor for core PTSD and showed little predictive value for depression. Rumination is a cognitive process which has been implicated as a core maintaining feature of both GAD and depression (Papageorgiou, Reference Papageorgiou, Davey and Wells2006); it showed a significant correlation with depressive symptoms but appeared not to predict severity of symptoms nine weeks post-trauma when set against other cognitive factors.
The cognitive model of PTSD may be challenged due to its similar estimates of variance accounted for and model fit indices for all disorders, suggesting poor specificity. However, all disorders studied have theoretical models implicating cognitive factors, with overlap across disorder specific models. The model specificity and goodness of fit results within this research may have reflected greater differences between disorders had we developed different models defining more specific cognitive features of each disorder a priori, demonstrated by Ehring et al. (Reference Ehring, Ehlers and Glucksman2008). This highlights the importance of assessing if children present with maladaptive cognitive processes given their transdiagnostic significance, and exploring these processes to elucidate to which specific symptoms they may be most vulnerable.
Psychosocial and event-related predictors of psychopathology following trauma
Experiencing an interpersonal index trauma (rather than an RTA or other accidental injury) appeared to lead to increased risk for all psychopathology. Younger age was not a significant predictor of any disorder, consistent with Trickey et al. (Reference Trickey, Siddaway, Meiser-Stedman, Serpell and Field2012). Both CPTSD and depression were predicted by poor perceived social support, highlighting the relevance of good interpersonal networks as a protective factor. Experiencing prior traumas also predicted CPTSD and depression but not GAD or PTSD; multiple childhood traumas have been implicated in developmental research exploring later psychopathology, in a dose-response relationship (e.g. Steine et al. Reference Steine, Winje, Krystal, Bjorvatn, Milde, Grønli and Pallesen2017; Turgoose, Wilkinson, Shevlin, & Karatzias, Reference Turgoose, Wilkinson, Shevlin and Karatzias2024). The development of GAD and PTSD may be less related to a disruption in development caused by early traumas.
There was a clear distinction between the relative predictive power of objective v. subjective event severity markers, with subjective experiences of greater fear, panic, and perceived threat during the trauma showing greater relevance in predicting later psychopathology than markers of injury severity or requirement for hospital admission. Perceived life threat was not found to be predictive of any disorders, in contrast to previous research (e.g. Cox et al., Reference Cox, Kenardy and Hendrikz2008). Feeling scared, panicked, or dissociating at the time of the event appeared more important, suggesting the emotional experience and fear response is more indicative of later psychopathology than threat appraisals. Peritraumatic pain was a significant predictor of all disorders, although this was measured post-trauma due to limited hospital data, and so could have been a proxy of the child's post-traumatic appraisal of the event.
Limitations and future directions
While this study is novel, a larger sample may have allowed for the use of structural equation modelling methods to identify outcomes more coherently; it could be that the four outcomes considered here do not accurately represent the range of symptoms that participants experienced. When planning for this study, CPTSD was not yet a diagnostic category, meaning a validated measure of CPTSD was not available. Our study supports a distinction between PTSD and CPTSD within youth, and the importance of assessing and treating maladaptive cognitive processes to potentially reduce the distressing symptoms of CPTSD, PTSD, depression, or anxiety. This field requires further exploration. In particular, we would stress that the nature of the present sample (i.e. children and adolescents recruited from emergency departments) means our findings cannot be generalized to children with multiple trauma exposure (e.g. maltreatment) or other forms of single event trauma (e.g. witnessing an event happening to someone else). Moreover, in seeking to evaluate the role of a wide range of event-related, psychosocial and cognitive process variables, some of the measures used were brief and may not have captured important aspects of the factor being considered (e.g. life stressors in the year prior to the index trauma was based on a frequency of events, and may not have captured the significance or impact of any specific life event).
Conclusions
These findings present a key addition to understanding the predictors of PTSD and related disorders in youth. The results support the cognitive model of PTSD, but also highlight a lack of disorder specificity of the model. Consideration of disorder-specific cognitions, or the prediction of an overall ‘distress’ factor post-trauma, may be pertinent in further exploration. Overall, the significance of subjective peritraumatic factors and post-traumatic cognitive processes consistently demonstrated the importance of assessing how a child experienced an event in understanding their potential susceptibility to psychopathological symptoms.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291724001648
Acknowledgements
This study was funded through a Medical Research Council (MRC) Clinician Scientist Fellowship awarded to Richard Meiser-Stedman (G0802821). T.D. was funded by the MRC. The authors gratefully acknowledge the support of the National Institute of Health Research Clinical Research Network (NIHR CRN). R.M.S., A.M., P.S. and T.D. train mental health professionals in the use of trauma-focused cognitive-behavioral therapies for the treatment of PTSD. The remaining authors have declared that they have no competing or potential conflicts of interest.
Funding statement
This study was funded through a Medical Research Council (MRC) Clinician Scientist Fellowship awarded to Richard Meiser-Stedman (G0802821). T.D. was funded by the MRC.







