Despite modest improvements in past decades, the nutritional status of women of reproductive age in Bangladesh remains alarming. In 2007, nearly one-third of women were undernourished with a BMI of <18·5 kg/m2 ( 1 ). Moreover, the prevalence of anaemia among women is still at a very high level. In 2010, the prevalence of anaemia was 48 % in women of reproductive age in Bangladesh( Reference Stevens, Finucane and De-Regil 2 ). To date, the major determinants of undernutrition and anaemia among women in poorer settings are assumed to be related to women’s behavioural and psychosocial risk factors and to overall socio-economic changes in the household and society( Reference Bitew and Telake 3 – Reference Rahman, Nakamura and Seino 6 ). However, the role that bio-demographic factors play in women’s nutritional status is less understood. Women’s high-risk fertility behaviours, largely in the form of short birth spacing, higher number of total live births, and too-early or too-late childbearing pattern, is considered to be one of the main bio-demographic risk factors that might influence women’s nutritional status. Since early marriage is common and there is a social expectation to have a child soon after marriage, a higher prevalence of teenage pregnancies is persistent in Bangladesh. According to the Bangladesh Demographic and Health Survey report, in 2007 half of women aged 25–49 years had their first birth by age 18 years and 12 % had their first birth by age 15 years. Bangladesh also has the highest percentage of births with an interval of less than 24 months (15·1 %)( 1 ).
A growing literature links various components of high-risk fertility behaviours to adverse child health outcomes( Reference Adekanmbi, Kayode and Uthman 7 – Reference Hsieh, Liou and Hsu 10 ). However, the literature on consequences of high-risk fertility behaviours on women’s nutritional patterns is limited. Investigators have documented the association of women’s chronic undernutrition and anaemia with short birth interval (<24 months) and with increasing birth order( Reference Noha and Sakina 11 – Reference Kefyalew and Abdullah 13 ). Scholars also noted that women who were married at the age of 18 years or less are more likely to be undernourished and anaemic than those who were married at the age of 18 years or more( Reference Saba, Gebremeskel and Ashenafi 14 , Reference Goli, Rammohan and Singh 15 ). In addition, researchers noted that the prevalence of chronic undernutrition is higher among older mothers (over 34 years at the time of delivery)( Reference Rahman and Nasrin 16 ). Although such evidence supports the consideration of various exposures of high-risk fertility behaviours as a high-priority maternal health concern, no studies have assessed the relationship between a combination of those exposures and the nutritional disadvantages of women. Therefore, analysis is needed for a clearer understanding of the separate and combined influences of maternal high-risk fertility behaviours and their association with chronic undernutrition and anaemia among women of reproductive age for the development of effective prevention programming in Bangladesh. Based on these considerations, we aimed to further this important area of inquiry by addressing whether an association exists between maternal high-risk fertility behaviours and the likelihood of (i) chronic undernutrition, (ii) anaemia and (iii) the coexistence of anaemia and undernutrition among women of reproductive age in a nationally representative sample of Bangladesh, where chronic undernutrition and anaemia are endemic.
Methods
Data sources
The current cross-sectional study used data from the Bangladesh Demographic and Health Survey (BDHS) 2011 conducted under the authority of the National Institute for Population Research and Training (NIPORT) of the Ministry of Health and Family( 17 ). A stratified, multistage cluster sample of 600 primary sampling units was constructed (207 in urban areas and 393 in rural areas). The primary sampling units were derived from a sampling frame created for the 2001 Bangladeshi census. The BDHS uses extensive interviewer training, standardized measurement tools and techniques, an identical core questionnaire and instrument pre-testing to ensure standardization and comparability across diverse sites and times.
The participants were evaluated by interviewers and biomarker staff (health technicians or nurses), who visited, interviewed and collected data at the participants’ household. Biomarker staff and interviewers were provided training (classroom training and practical experience) according to a manual developed for the survey. Contents of training included building rapport with a respondent, conducting a successful interview, anthropometry measurements, blood test using HemoCue 201+ and disposal of hazardous waste. Trained data collectors performed face-to-face interviews with an adult member in each of the 17 141 selected households to obtain demographic information about the household and family members, achieving a household response rate of 98 %. The high response rate for the BDHS was attributed to the rigorous training of field staff and close supervision of the fieldwork. Moreover, numerous efforts were made during the fieldwork to ensure high response rates: interviewers were trained to maintain motivation with longer questionnaires, probe for responses, clarify ambiguous questions, perform multiple revisits to the households, and to control the order of the questions. Fieldwork was monitored through visits by representatives from the US Agency for International Development, MEASURE DHS and NIPORT using additional quality control teams. In addition, to achieve the target number of sample units, non-response rates for sample units were estimated from past surveys at the time of the sample design and were then used to determine the required number of units to be selected( 17 ).
The 2011 BDHS used five questionnaires. The questionnaires were drafted in English and were then translated into Bangla, the national language of Bangladesh. The translations were reviewed by experts and volunteers, and a pilot study was conducted as a validation exercise. Of the 18 222 eligible women in the households that were surveyed, 98 % participated in a survey of maternal and child health behaviours and outcomes. The anaemia module was a relatively new addition to 2011 BDHS and was administered to one-third of the eligible households. Anaemia measurements were obtained from 5902 ever-married women aged 15–49 years, of which 95 % of the measurements were completed. Because in the BDHS high-risk fertility behaviours were measured only for those women whose children were born in the 5 years preceding the survey, in our analyses we excluded childless women and included only ever-married women aged 15–49 years living with the last-born child younger than 5 years (n 2197; Fig. 1).
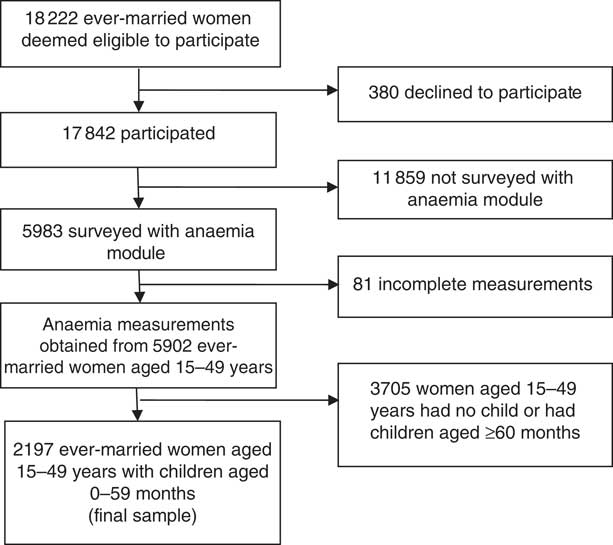
Fig. 1 From the original anaemia module of 5983 eligible women aged 15–49 years, we obtained a final sample of 2197 for the present study, 2011 Bangladesh Demographic and Health Survey
Outcomes
Three outcomes were analysed in the present study: (i) chronic undernutrition; (ii) anaemia; and (iii) the coexistence of anaemia and undernutrition. The 2011 BDHS measured the height and weight of all women aged 15–49 years who had ever married. Trained investigators weighed each woman by using a solar-powered scale with an accuracy of ±100 g, and height was measured by using an adjustable board calibrated in millimetres and theoretically accurate to 1 mm. BMI, calculated as weight in kilograms divided by the square of height in metres, was used to assess chronic undernutrition. We chose BMI to assess undernutrition of mothers because it does not require a reference table from a well-nourished population. BMI <18·5 kg/m2 was used to define chronic undernutrition as recommended by the WHO for populations from the Indian subcontinent( 18 ). BMI≥25·0 kg/m2 usually indicates overweight and BMI≥30·0 kg/m2 indicates obesity.
Anaemia (Hb) level was measured in g/dl, operationalized as a categorical variable by predefined cut-off points for mild, moderate and severe anaemia recommended by the WHO( 17 ). For non-pregnant women, any anaemia was defined as Hb<12 g/dl, and for pregnant women as <11 g/dl. Mild anaemia was defined as 10–11·9 g/dl for non-pregnant women and 10–10·9 g/dl for pregnant women. Moderate/severe anaemia was defined as Hb <10 g/dl. Both non-pregnant and pregnant women were included in the analysis. A binary variable was created to define any anaemia (composite variable of mild, moderate and severe anaemia). Anaemia testing was conducted by specially trained personnel who were part of the survey team. The finger-prick tests were carried out in the homes of the respondents and blood samples were tested immediately using a portable hand-held HemoCue testing system. We also defined a binary variable for the coexistence of anaemia and undernutrition. For the biomarker examination, in some cases if the results were found abnormal, participants were re-tested with a second finger-prick test. If the first and second tests were discordant, a third confirmatory test was administered in an independent laboratory( 17 ).
Exposure
Maternal high-risk fertility behaviours were the exposure of interest in the current study. We applied the definition of ‘high-risk fertility behaviours’ adopted by the 2011 BDHS( 17 ). We considered three parameters, maternal age at the time of delivery, birth order and birth interval, to define the high-risk fertility behaviours. Three exposure variables were defined for this analysis: (i) any high-risk fertility behaviour v. none; (ii) exposure to different categories of high-risk fertility behaviours v. none (defined as exposure to single high-risk category v. none and multiple high-risk categories v. none); and (iii) the specific types of high-risk fertility behaviours v. none. The presence of any of the following four conditions was termed a single high-risk fertility behaviour: (i) mothers aged less than 18 years at the time of delivery; (ii) mothers aged over 34 years at the time of delivery; (iii) latest child born less than 24 months after the previous birth; and (iv) latest child of order three or higher. Combinations of two or more single conditions are referred to as multiple high-risk categories.
Control variables
We included several sociodemographic variables that are theoretically and empirically linked to maternal high-risk fertility behaviours and undernutrition among women of reproductive age( Reference Noha and Sakina 11 – Reference Rahman and Nasrin 16 ). We classified participants by their current age into empirically important groups: younger (15–24 years), middle aged (25–34 years) or older (35–49 years). The women’s educational level was defined in terms of the formal education system of Bangladesh: no education (0 year), primary (1–5 years) or secondary or higher (6 years or more). Place of residence was categorized as rural v. urban. After consultation with experts, the Demographic and Health Surveys use a standardized approach to measure women’s decision-making autonomy( Reference Kishor and Subaiya 19 ). The 2011 BDHS stated that to ensure the validity and reliability of data collected regarding women’s decision-making autonomy, fieldworkers underwent careful training in different aspects of interview techniques and the questionnaires were pre-tested in pilot studies. Moreover, to make valid cross-national comparisons, the questionnaire that was used to measure women’s decision-making autonomy in the BDHS included the same criteria and methods used in all cultural contexts( 17 ). To obtain information on the measure of women’s decision-making autonomy, the BDHS asked the following questions: (i) ‘Who has final say on making large household purchases?’; (ii) ‘Who has final say on making household purchases for daily needs?’; (iii) ‘Who has final say on the woman’s own health care?’; and (iv) ‘Who has final say on visits to family or relatives?’ In each of the questions, responses were coded as: (i) respondent; (ii) respondent and husband/partner jointly; (iii) respondent and someone else; (iv) husband/partner; or (v) someone else in the household. To assess the respondent’s autonomy, binary variables were created for each of the questions by merging responses (i), (ii) and (iii) into one category as having decision-making power and merging responses (iv) and (v) into one category which indicates no decision-making power. The Cronbach’s α for this measure was 0·69.
We created a variable for maternal occupation and classified women according to whether they were not working or were working in a manual, non-manual or agricultural profession. Total number of household members was classified in tertiles (2–4, 5–6 or 7+). Types of delivery were categorized as normal v. caesarean. Religion was categorized as Muslim or non-Muslim. The BDHS wealth index was constructed from data on household assets, including ownership of durable goods (such as televisions and bicycles) and dwelling characteristics (such as source of drinking-water, sanitation facilities and construction materials). Each asset was assigned a weight (factor score) generated through principal component analysis, and the resulting asset scores were standardized in relation to a standard normal distribution with a mean of 0 and an sd of 1( 17 ). Each household was then assigned a score for each asset and the scores were summed by household. The household population was then divided into three groups of equal size: poor, middle or rich, based on the wealth index score of the household in which the household members were living. We classified maternal height into two categories: <145 or ≥145 cm. The cut-off point for short stature is considered as <145 cm for height, because most studies from the South Asian region and other developing countries have used this cut-off for screening high-risk women( Reference Bhaskar, Deo and Neupane 20 , Reference Subramanian, Ackerson and Davey Smith 21 ).
Analytical methods
Descriptive analyses are presented first, to provide general information on the characteristics of the study population. We used a generalized estimating equation–modified Poisson regression approach with robust error variance with a clustered variable option( Reference Zou 22 ) to produce direct assessments of the risk ratios (RR). We created three fully adjusted regression models to analyse each binary outcome variable (chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition), with each model containing different high-risk fertility behaviours predictors (any v. no risk; separate effects of single high-risk and multiple high-risk v. no risk; specific types of high-risk v. no risk). We entered all the covariates simultaneously into the multiple regression models. Spearman correlation coefficients among the independent variables were examined to determine possible collinearity. Place of residence was not included in any adjusted analyses due to high correlations with both wealth index (r=−0·45) and maternal education level (r=0·51).
We estimated the RR to assess the strength of the associations and used the 95 % CI for significance testing. Significance for all analyses was set at P<0·05. The proportion of undernutrition, anaemia and the coexistence of anaemia and undernutrition attributable to maternal high-risk fertility behaviours was estimated from the frequency of any high-risk and the RR were obtained in the multivariate model using the expression: {[p×(RR–1)]/[1+p×(RR–1)]}×100, where p = prevalence of any high-risk fertility behaviours and RR = associated outcome effect size( Reference Greenland and Drescher 23 ). Sample weights were used for all analyses and statistical testing was performed in the statistical software package Stata for Windows release 11.0).
Ethical considerations
The data collection procedures for the BDHS 2011 were carried out with the approval of the ORC Macro Institutional Review Board. The survey protocol was reviewed and approved by the National Ethics Review Committee of the Bangladesh Ministry of Health and Family Welfare. Before starting the interview, informed consent was obtained from individual respondents followed by an oral explanation by interviewers according to the guidelines of the BDHS. The BDHS does not require a third person to witness the consent interview. In general, literate participants are asked to read and sign a consent form, while the form is read out to illiterate participants, who then give verbal consent. With the addition of anaemia testing, the BDHS added two further consent forms; one sought consent to draw blood and test it for anaemia, while the second sought consent to pass the names of individuals with severe anaemia on to health authorities for follow-up.
Respondents were informed of the voluntary nature of the survey, the purpose of use of the gathered data (assessment of health needs and planning health services), the confidentiality of results of the individual interview and biomarker examination, and that the examination was free of charge. After testing for anaemia, the BDHS teams gave results on the spot and referred women to health clinics where necessary. Severe cases were also referred directly to clinic staff, but there was no further follow-up. The blood testing was anonymous. No names or other contact information were recorded on the samples. In some cases, if a woman wanted to consult her husband before giving permission, the interviewer made an appointment to return to the household later at an agreed-upon time.
Results
Descriptive statistics
Table 1 shows the sociodemographic, biomarker and high-risk fertility behaviours characteristics of the study sample. A total of 2197 women of reproductive age were included in the current study. Approximately half of the participants (49·9 %) were 15–24 years old, 18·7 % had no education, 91·3 % were Muslim and 77·1 % lived in rural areas. Of the women, 20·1 % had no decision-making autonomy. Regarding their occupation status, 89·7 % of the women had no jobs and 30·5 % lived in a household with two to four members.
Table 1 Sociodemographic, biomarker and high-risk fertility behaviours characteristic of the study participants; ever-married women aged 15–49 years living with at least one child younger than 5 years, 2011 Bangladesh Demographic and Health Survey (n 2197)

Numbers are unweighted; percentages are weighted.
† Aspects of family decisions a woman participated alone or jointly in making.
‡ BMI categories were chronic undernourished (<18·5 kg/m2), normal (18·5–24 9 kg/m2) and overweight/obese (≥25·0 kg/m2).
From the total sample population, 31·0 % of the women were defined as rich, 33·9 % belonged to the middle band of wealth and 35·1 % were defined as poor. Regarding nutritional status, 60·8 % of the women were considered to be of normal weight, 27·7 % were undernourished or thin (BMI<18·5 kg/m2) and 11·5 % were overweight or obese (BMI≥25·0 kg/m2). Overall, 13·6 % of women fell below the stature cut-off of 145 cm. The prevalence of anaemia in our study sample was 43·7 %. Approximately 14 % of the participants were both chronically undernourished and anaemic.
A substantial percentage of women were exposed to have high-risk fertility behaviours (41·8 %); 33·0 % were at single high-risk and 8·8 % were at multiple high-risk. The most common single high-risk category was mother’s younger age at birth (younger than 18 years) followed by a birth order of three or more. The most common multiple high-risk of fertility behaviours was mothers’ age at birth more than 34 years and birth order of three or more (4·0 %).
Table 2 shows the sociodemographic and biomarker differential on high-risk fertility behaviours of married Bangladeshi women. The prevalence of any high-risk fertility behaviours, single high-risk fertility behaviours and multiple high-risk fertility behaviours was higher among the chronically undernourished or anaemic or women who were both chronically undernourished and anaemic.
Table 2 Descriptive statistics of study participants according to different forms of high-risk fertility behaviours; ever-married women aged 15–49 years living with at least one child younger than 5 years, 2011 Bangladesh Demographic and Health Survey (n 2197)

† Aspects of family decisions a woman participated alone or jointly in making.
‡ BMI categories were chronic undernourished (<18·5 kg/m2), normal (18·5–24·9 kg/m2) and overweight/obese (≥25·0 kg/m2).
Multivariate analyses
Table 3 shows the adjusted risk ratios (ARR) for chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition according to the high-risk fertility behaviours. After adjusting for relevant covariates, high-risk fertility behaviours increased the risk of chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition by 22 % (% increase=[(ARR–1) ×100], e.g. (1·22–1)×100=22 % increase in risk), 12 % and 52 %, respectively. Relative to women who were not falling in any high-risk categories, women who fell in a single high-risk category had 1·19 times (95 % CI 1·00, 1·42) increased likelihood of chronic undernutrition and 1·46 times (95 % CI 1·11, 1·92) increased likelihood of the coexistence of anaemia and undernutrition.
Table 3 Adjusted risk ratios (ARR) for associations between different forms of high-risk fertility behaviours and chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition among study participants; ever-married women aged 15–49 years living with at least one child younger than 5 years, 2011 Bangladesh Demographic and Health Survey (n 2197)
Ref., reference category.
*P<0·001, **P<0·01, ***P<0·05.
† Adjusted for anaemia.
‡ Adjusted for chronic undernutrition.
§ Models were adjusted for maternal age, education, maternal decision-making autonomy, maternal occupation, residence, number of household members, maternal height, type of delivery, pregnancy intention and current use of contraception.
|| Includes the categories: age at birth <18 years and birth order ≥3; age at birth <18 years, birth order ≥3 and birth interval <24 months.
¶ Includes the categories: age at birth >34 years and birth order ≥3; age at birth >34 years, birth order ≥3 and birth interval <24 months.
A significant association was observed between multiple high-risk fertility behaviours and chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition. Regarding specific types of high-risk categories, significant associations were observed for mothers having a birth order of three or more and maternal age at birth over 34 years and having a birth order of three or more with chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition. In addition, a significant association was observed for a preceding birth interval of less than 24 months and having a birth order of three or more with anaemia.
Population-attributable risk fractions
Calculations based on population-attributable risk estimates suggested that chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition would decrease by 8·4, 4·8 and 17·9 %, respectively, if any high-risk fertility behaviours were eliminated in Bangladesh.
Discussion
To the best our knowledge, the present study is the first of the relationship between separate and combined influences of high-risk fertility behaviours and chronic undernutrition and anaemia among women in Bangladesh. Findings from this large representative survey indicated that approximately 42 % of married woman in Bangladesh were subject to at least one of the high-risk fertility behaviours. This extremely high prevalence rate confirms that high-risk fertility behaviours are alarmingly commonplace in this impoverished South Asian nation, potentially affecting the health of a majority of Bangladeshi women. Findings also revealed that, despite economic growth and a reduction in poverty over the past decade, chronic undernutrition among women was still rampant in Bangladesh (27·7 %). This observed rate is higher than in some neighbouring countries of South Asia, including Nepal (18 %) and Pakistan (14·1 %)( 24 , 25 ). The observed rate of chronic undernutrition is also even eclipsing that in many countries of sub-Saharan Africa including Ghana (8·6 %), Nigeria (11·4 %), Kenya (12·3 %) and Namibia (13·8 %)( 26 – 29 ). The prevalence of anaemia in our study population was 43·7 %, which is higher than levels reported in many other developing and developed countries (7·7–32·8 %)( Reference Massot and Vanderpas 30 – Reference Pala and Dundar 32 ). However, the level of anaemia found in our study is similar to that found in some countries in the South Asian region among women of reproductive age including India (54 %), Pakistan (51 %) and Nepal (35 %)( 1 , 24 , 25 ) and some countries in sub-Saharan Africa including Ghana (58·7 %) and Tanzania (40·1 %)( 26 , 33 ).
The present study further revealed an elevated fortuity of chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition among women who were subject to one of the high-risk fertility behaviours categories in Bangladesh. Our findings of the association between high-risk fertility behaviours and chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition among women strongly suggest that high-risk fertility behaviours threaten not only the health and well-being of children of the women but also the women’s own health. Importantly, because the present analyses were adjusted for potential confounders, these effects persist after consideration of demographic characteristics, multiple domains of socio-economic status, household characteristics and maternal characteristics that are strong confounders of fertility and nutritional status. Our findings of the association between high-risk fertility behaviours and chronic undernutrition and anaemia among women build on previous work that demonstrates a range of negative health consequences of various determinants of high-risk fertility behaviours on women( Reference Noha and Sakina 11 – Reference Rahman and Nasrin 16 ) and children( Reference Adekanmbi, Kayode and Uthman 7 – Reference Hsieh, Liou and Hsu 10 ).
There are many mechanisms through which high-risk fertility behaviours could be related to increased likelihood for chronic undernutrition and anaemia among women. Closely spaced pregnancies do not give a mother enough time to recover from the physical stress of one pregnancy before moving on to the next, and stress, in turn, can increase oxidative stress( Reference Epel, Blackburn and Lin 34 , Reference Hapuarachchi, Chalmers and Winefield 35 ) and metabolic levels( Reference Irie, Asami and Nagata 36 ), risk factors for undernutrition. Pregnancy and breast-feeding can deplete the stores of essential nutrients, such as Fe and folate. Closely spaced pregnancies are often associated with the mother having little time to regain lost fat and nutrient stores, therefore affecting her health and nutritional status(37). Besides, too many births are also associated with inappropriate care of the mother herself, making her vulnerable to further undernutrition and disease( Reference Adebowale, Adepoj and Fagbamigbe 12 ). Early childbearing can lead to severe blood loss during childbirth, so anaemia is common( Reference Kefyalew and Abdullah 13 ). Early childbearing can also affect the nutritional status of women indirectly. First, it adversely affects educational attainment, because early marriage is cited as an important factor for school and college dropouts among girls in developing countries( Reference Goli, Rammohan and Singh 15 , Reference Rah, Christian and Shamim 38 ). Further, low level of education impacts on work status and leads to lower income and low autonomy, which together affect nutritional purchasing power, nutritional intake behaviour and outcomes( Reference Rah 39 ). Moreover, certain behavioural risk factors, such as failure to use health-care services and socio-economic disadvantage, are more common in women who have closely spaced pregnancies, a higher number of total live births, or a too-early or too-late childbearing pattern( Reference Srivastava, Mahmood and Mishra 40 ). These risk factors might explain the link between high-risk fertility behaviours and nutritional disadvantages for mothers.
Another new important finding is that multiple high-risk fertility behaviours appeared to have more profound consequences on the outcomes that were measured. There seems to be a dose–response relationship observed between the types of high-risk fertility behaviours and women’s nutritional disadvantages. This is in line with previous observations, according to which exposure to multiple high-risk fertility behaviours predicts higher levels of depressive symptoms, higher levels of biological vulnerability, receiving inappropriate preventive and curative services, and performing inadequate breast-feeding practices( Reference Rutstein and Rebecca 41 , Reference Rahman, Nakamura and Seino 42 ), all of which may, in turn, facilitate women’s chronic undernutrition and anaemia.
The main strength of the present study is that the data came from a large government survey; a relevant subset was extracted consisting of married women aged 15–49 years, who were living with their last born children in the 5 years preceding the survey, giving a large sample size. The size provided the study with good statistical power and the data contained information on potential confounding factors with a low proportion of missing information.
We note several important caveats to the findings presented here. First, our exposure variables are based on self-report, which is vulnerable to social desirability and recall biases. However, in order to avoid such biases, analyses were restricted to women living with their last children born in the 5 years preceding the survey. Second, the analyses are cross-sectional and causality cannot be assumed. Prospective investigation is needed to better evaluate the effects of high-risk fertility behaviours on women’s health outcomes. Finally, the study can be criticized for using an indirect measure of household wealth. However, because it is hard to obtain reliable income and expenditure data in developing countries like Bangladesh, an asset-based index is generally considered a good proxy for household wealth status.
In spite of these limitations, our study brings to light important information that could serve as a basis for reducing the likelihood of chronic undernutrition and anaemia among women of reproductive age in Bangladesh. Our results may also be relevant in other resource-limited settings where maternal undernutrition and anaemia are common, and they may be of interest to clinicians assessing women with problems related to nutritional status.
Conclusions
Maternal high-risk fertility behaviours are shockingly frequent practices among women in Bangladesh, which likely affects the health of the women. The high-risk fertility behaviours are important predictors of the increased likelihood of women’s chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition. Our findings underscore the calls for avoiding high-risk fertility behaviours, which are largely in the form of short birth spacing, higher number of total live births, and too-early or too-late childbearing pattern, in order to reduce the likelihood of chronic undernutrition, anaemia and the coexistence of anaemia and undernutrition among women of reproductive age. Investigation of the causal link between high-risk fertility behaviours and women’s nutritional outcomes will be critical to developing interventions to improve women’s nutritional status, which is a public health research priority.
Acknowledgements
Acknowledgements: The authors are grateful to MEASURE DHS for providing the data set. In addition, they would like to acknowledge all individuals and institutions in Bangladesh involved in the implementation of the 2011 BDHS. Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: The authors declare that they have no competing interests. Authorship: M.R. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: M.R.; acquisition of data: M.R.; statistical analysis: M.R., M.J.I., S.E.H., M.N.H., Y.M.S., N.H.C.D., S.A.-S., T.N.S.; analysis and interpretation of data: M.R., M.J.I., S.E.H., M.N.H., Y.M.S., N.H.C.D., S.A.-S.; drafting of the manuscript: M.R.; critical revision of the manuscript for important intellectual content: M.R., M.J.I., S.E.H., M.N.H., Y.M.S., N.H.C.D., S.A.-S., T.N.S., M.G.M., M.R.I. Ethics of human subject participation: Data collection procedures for the BDHS were carried out with the approval of the ORC Macro Institutional Review Board. The survey protocol was reviewed and approved by the National Ethics Review Committee of the Bangladesh Ministry of Health and Family Welfare. Informed consent was obtained from all individual respondents before starting the interview.







