During the first year of life, the infant is growing fast and adequate nutrition is essential for optimal growth and health. Breast milk provides important immunological and growth-modulating factors and all nutrients in sufficient amounts to cover the infant’s nutritional needs for the first 6 months, with the exception of vitamin D( Reference Butte, Lopez-Alarcon and Garza 1 ). Exclusive breast-feeding for the infant’s first 4–6 months has been associated with a reduced risk of infant morbidity and mortality from infections( Reference Hornell, Lagstrom and Lande 2 ). Long-term benefits of breast-feeding include reduced risk of overweight/obesity, diabetes and high blood pressure, as well as increased intelligence quotient( 3 – Reference Kelishadi and Farajian 6 ). On this basis, international agencies such as WHO, as well as Norwegian health authorities, recommend exclusive breast-feeding the first 6 months of life followed by a combination of continued breast-feeding and gradual introduction of appropriate complementary foods( 7 , 8 ).
The prevalence of breast-feeding in Norway and other Scandinavian countries is generally high compared with other industrialized countries, such as the UK and France( Reference Ibanez, Martin and Denantes 9 ). The Norwegian national dietary surveys among infants conducted in 1998 and 2006 documented high breast-feeding rates in Norway( Reference Lande, Andersen and Baerug 10 , Reference Kristiansen, Lande and Overby 11 ). The last survey reported that 10 % of infants were exclusively breast-fed and 82 % were breast-fed at 6 months of age( Reference Kristiansen, Lande and Overby 11 ). However, these studies only included mothers born in Scandinavia. A more recent national survey in 2013, including mothers born outside Scandinavia, reported that 3 % of all participating infants were exclusively breast-fed and 77 % were breast-fed at 6 months of age( Reference Lande and Helleve 12 ). Nine per cent of the participating mothers were born outside Europe but the study did not disaggregate the results with regard to the mother’s country of birth.
In recent decades, the population of immigrants and Norwegian-born to immigrant parents has increased rapidly. Numbers from 2014 showed that immigrants constituted about 13 % of the Norwegian population, while individuals who were Norwegian-born to immigrant parents accounted for 2·6 %( 13 ). The largest populations of immigrants and Norwegian-born to immigrant parents were in Oslo, constituting 32 % of the capital’s entire population. The proportions were also high in certain areas of the counties of Akershus and Buskerud( 13 ). The two non-Western immigrant groups with the highest birth rates in Norway in the last few years have been from Somalia and Iraq (Statistics Norway, Population 1 January 2012 and 2013 and Changes in 2012, by Immigration Category and Country Background, Absolute Numbers, personal communication, 2013).
A number of studies have shown that breast-feeding patterns can differ profoundly between ethnic subgroups in a society and these differences may be influenced by several factors, such as cultural contexts and country of residence( Reference Castro, Layte and Kearney 14 – Reference Schmied, Olley and Burns 19 ). Studies specifically investigating the infant feeding practices among those with immigrant backgrounds have been called for by the Norwegian Directorate for Health( Reference Lande, Andersen and Bærug 20 ).
The main objective of the present study was to examine the prevalence of exclusive breast-feeding and breast-feeding and complementary feeding practices among Norwegian-born infants of Somali and Iraqi origin during the first 6 months of life. A secondary objective was to identify factors associated with exclusive breast-feeding and breast-feeding practices in this group of children.
Methods
Participants and design
A cross-sectional survey was carried out during the period of March 2013 through February 2014 in the Norwegian counties of Oslo, Akershus and Buskerud. Mothers born in Somalia or Iraq and living in one of these counties, and who had a 6-month-old infant, were eligible for inclusion. Children on special diets due to serious illnesses or conditions were excluded from the study. If the mother had twins or triplets, only one of the children was included by random selection. Identification of the eligible mothers was done through: (i) selected child health centres in Oslo, Akershus and Buskerud, where nurses were asked to inform eligible mothers about the study and to submit their contact information if the mothers were interested in learning more; and (ii) lists obtained from the National Population Register showing eligible mothers living in Oslo, Akershus and Buskerud who had given birth between August 2012 and July 2013. The lists were used for: (i) sending information letters to registered addresses about a month before the child turned 6 months old; (ii) making follow-up calls to mothers with registered telephone numbers if no response to the information letter was received; and (iii) visiting the mothers at their registered addresses if they were not reached by letter or telephone. The last approach was only used during the last 3 months of the recruitment period, in order to make the recruitment more efficient. The snowball method was also used during the whole recruitment period. Mothers could therefore have been approached through multiple channels, about which they were notified in the information letter sent to their address.
A paper-based, semi-quantitative FFQ was used to collect the data through personal interviews with the participating mothers. Trained female fieldworkers who spoke Norwegian, Somali, Arabic, Kurdish or English scheduled an interview at a time and place chosen by the mother, as close as possible to the date the child reached 6 months of age. In cases in which the mother was unable to meet, a telephone interview was conducted. Each mother who completed the interview received a baby-shop voucher for approximately $US 25.
The study was approved by the Regional Committees for Medical and Health Research Ethics and informed consent was obtained from the participating mothers.
The semi-quantitative FFQ
The semi-quantitative FFQ was designed to estimate exclusive breast-feeding, breast-feeding and other complementary feeding practices at 6 months of age and retrospectively from birth up to the given age. The FFQ was based on the FFQ used in the second Norwegian national dietary survey among infants in 2006–2007( Reference Øverby, Kristiansen and Andersen 21 ). A pilot study was conducted on a total of six Somali-born and Iraqi-born mothers to test the FFQ and it was revised accordingly.
The final FFQ included fifty questions about seven topics: (i) breast milk; (ii) infant formula and other milk; (iii) solid foods; (iv) liquids; (v) food intolerance/allergies; (vi) supplements; and (vii) infant nutrition information. The first questions were related to whether or not the child received breast milk and at what frequency. Breast milk intake was not quantified. The mothers were also asked whether and when the child stopped receiving breast milk, whether and when she/he started receiving infant formula/other milk, and whether and when solid and semi-solid foods were introduced for the first time. Types of foods, liquids and supplements received and the frequency of consumption at 6 months of age were also recorded.
After completing the FFQ, a single 24 h recall was conducted in which the mothers were asked to recall all foods and drinks given to the child, including breast milk frequency, from the time the child woke up the day before until the time the child woke up on the day of interview. The 24 h recall was used only during the interview situation in order to ensure coherence with some of the answers given on the FFQ with regard to whether the mother was still breast-feeding and/or had introduced complementary foods. In case of any detected mismatches or misunderstandings, the mothers were asked to elaborate on the questions of concern.
Participating mothers were asked to bring their infants’ health cards to the interview in order to record data on length and weight at birth. In addition, twenty-nine questions were asked regarding background information on parental education levels, current maternal age, age when the mother immigrated to Norway, maternal work situation, maternal marital status, number of children/parity, infant gender and gestational age, among other information.
Definitions of immigrants
Some studies referred to in the present article use the term ‘ethnic minorities’, whereas others use ‘immigrants’. Statistics Norway uses the following definitions: (i) ‘immigrants’ are persons who are born abroad to two foreign-born parents and who have moved to Norway; and (ii) ‘Norwegian-born to immigrant parents’ are those born in Norway to two immigrant parents( 13 ). In the present paper, ‘Norwegian-Somali infants’ and ‘Norwegian-Iraqi infants’ refer to Norwegian-born infants of mothers born in Somalia and Iraq, respectively.
Definitions of breast-feeding
Based on the WHO’s classification of breast-feeding( 22 ), the following definitions are used throughout the present paper. ‘Exclusive breast-feeding’ refers to infants who received only breast milk, with no additional foods and/or drinks, not even water. They may, however, have received vitamin and/or mineral supplements. ‘Breast-feeding’ refers to all infants who received breast milk, regardless of whether it was exclusive or given with other complementary foods and/or drinks.
Data entry and statistical analysis
Data from the FFQ and background information were manually entered in CSPro version 5·0 (US Census Bureau, Macro International and Serpro, S.A.) and further processed and analysed in the statistical software package IBM SPSS Statistics version 22·0. Background characteristics did not adhere to normal distribution and continuous variables are therefore presented as median and the 25th and 75th percentiles. Continuous variables were compared by the Mann–Whitney test. The χ 2 test was used to compare categorical variables. Multiple logistic regression analysis was applied to study exclusive breast-feeding at 3·5 months of age and breast-feeding at 6 months of age, in relation to selected maternal and infant characteristics. These ages were chosen to study adherence to the recommendations on infant feeding and previous national data on infants from Norway. Due to the small number of exclusively breast-fed infants at 4 months of age (n 15), infants exclusively breast-fed at 3·5 months (up to 4 months of age) were used in the multivariate model (n 40). Maternal age and number of years lived in Norway were reported as continuous variables. In the analysis, maternal age was combined into three categories: ≤24, 25–34 and ≥35 years. Number of years lived in Norway were categorized into two groups: ≤10 and >10 years. Parental education levels were reported in ten categories, capturing the highest education completed by the mother and father in both Norway and any other country. These were reduced to two categories for analysis: no/basic education (≤11 years) and high school/higher education (≥12 years), independent of it being completed in Norway or any other country. Work before pregnancy was also reported in ten categories and combined into two categories in the analysis: not working or working (full-time/part-time). Four categories of number of children were coded into two: ≤2 and >2 children. Six categories for language spoken at home were categorized into two: Norwegian and other languages. Univariate statistical analyses (with a criterion of P<0·10) and evidence from the literature were used to decide which variables to examine in the multivariate analyses. In the final models, country of origin, maternal age and maternal education were included regardless of the level of statistical significance in the univariate models. All other variables significant in the univariate models (P<0·05) were also included. All analyses were performed by both including and excluding mothers interviewed by telephone (n 10) and these indicated no differences in the results. Thus, mothers interviewed by telephone are included in the analyses presented in the current paper. Results from the regression analyses are presented with both unadjusted and adjusted odds ratios and confidence intervals. In all the final analyses, statistical significance was indicated by two-sided P<0·05.
Results
According to lists from the National Population Register, 481 Norwegian-Somali infants and 287 Norwegian-Iraqi infants living in Oslo, Akershus or Buskerud turned 6 months old during the recruitment period (Fig. 1). A total of 107 mothers/infants of Somali origin (22·2 %) and eighty mothers/infants of Iraqi origin (27·9 %) participated in the study. Mothers were recruited mainly by telephone or by us approaching their home address. Among the Somali-born mothers participating, 69 % lived in Oslo, 17 % in Akershus and 14 % in Buskerud. Sixty-nine per cent of the interviews were performed in Somali, 30 % in Norwegian and 1 % in English. Seven per cent of the interviews were conducted by telephone. Among the Iraqi-born mothers participating, 51 % lived in Oslo, 30 % in Akershus and 19 % in Buskerud. Half of the interviews were performed in Kurdish, 25 % in Arabic and 25 % in Norwegian. Four per cent were telephone interviews.
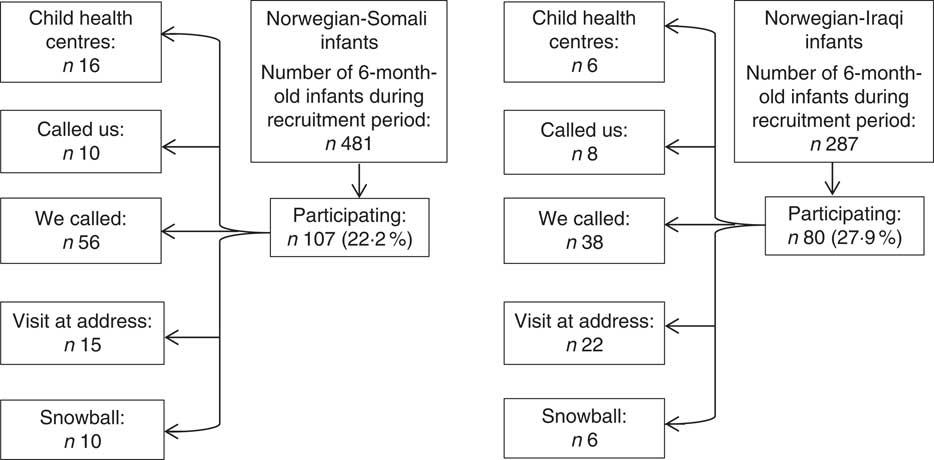
Fig. 1 Recruitment of participants in the survey
Selected characteristics of the infants and their parents are presented in Table 1. Median ages were 30 and 32 years among participating Somali-born and Iraqi-born mothers, respectively. Somali-born mothers had immigrated to Norway at earlier ages than Iraqi-born mothers and had lived in Norway for longer periods of time. Educational levels and the percentage of mothers having worked before pregnancy were significantly higher among the Iraqi-born mothers compared with the Somali-born mothers (Table 1).
Table 1 Characteristics of the infants and parents sampled (n 187); InnBaKost survey, March 2013–February 2014

P25, 25th percentile; P75, 75th percentile.
* Data are presented as median and P25–P75 for continuous variables, or as percentages for categorical variables.
† P values for the comparison of infants and parents of Somali and Iraqi origin.
‡ The birth weights of four Norwegian-Somali infants and two Norwegian-Iraqi infants, and the birth lengths of nine Norwegian-Somali and nine Norwegian-Iraqi infants, are missing. The gestational age of one Iraqi-born mother, the age when immigrated to Norway and the number of years lived in Norway of three Iraqi-born mothers, and the number of children of one Somali-born mother, are missing. The education levels of two Somali fathers are missing. These are not included in the calculations.
Breast-feeding practices
Breast-feeding was almost universally initiated after birth in both groups (a total of 93 % within 24 h). Two per cent of the Norwegian-Somali infants and 1 % of the Norwegian-Iraqi infants had never been breast-fed. Colostrum was fed to the majority of infants, but 8 % of Somali-born mothers and 6 % of Iraqi-born mothers reported not having fed their children colostrum.
Among Norwegian-Somali infants, the proportion of exclusively breast-fed infants was 37 % at 1 month of age and 21 % at 3 months of age, decreasing to 7 % at 4 months of age, and none were exclusively breast-fed at 5 months of age (Fig. 2). Thirty-five per cent of the Norwegian-Iraqi infants were exclusively breast-fed at 1 month of age and 26 % at 3 months of age; the proportion decreased to 10 % at 4 months of age and further decreased to 1 % at 5·5 months of age. None were exclusively breast-fed at 6 months of age (Fig. 2). There were no significant differences in the proportions of exclusive breast-feeding between the two groups.
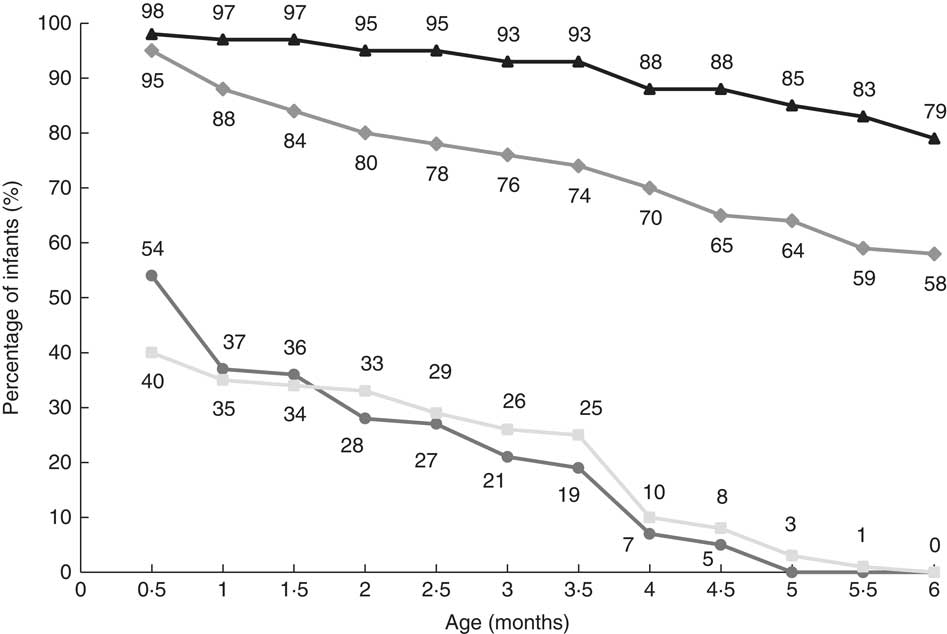
Fig. 2 Exclusive breast-feeding among Norwegian-Somali (![]() ) and Norwegian-Iraqi (
) and Norwegian-Iraqi (![]() ) infants and breast-feeding among Norwegian-Somali (
) infants and breast-feeding among Norwegian-Somali (![]() ) and Norwegian-Iraqi (
) and Norwegian-Iraqi (![]() ) infants during the first 6 months of life (Somali n 107; Iraqi n 80); InnBaKost survey, March 2013–February 2014
) infants during the first 6 months of life (Somali n 107; Iraqi n 80); InnBaKost survey, March 2013–February 2014
Breast-feeding decreased from 97 % at 1 month of age to 79 % at 6 months of age among Norwegian-Somali infants (Fig. 2). At 6 months of age, the mean breast-feeding frequency among those still breast-feeding was 6·5 times/d. Among Norwegian-Iraqi infants, breast-feeding decreased from 88 % to 58 % from 1 to 6 months of age (Fig. 2). Mean breast-feeding frequency was 8·5 times/d at 6 months of age among those still breast-feeding. At 4 and 6 months, breast-feeding was more common among Norwegian-Somali infants compared with Norwegian-Iraqi infants (P<0·001 and P=0·001, respectively).
Twenty-two Somali-born mothers and thirty-four Iraqi-born mothers ceased breast-feeding before 6 months of age. The most important reasons for this given by the Somali-born mothers were insufficient milk (59 %) and the infant no longer wanting breast milk (32 %). Among the Iraqi-born mothers, the most important reasons given were insufficient milk (56 %), the mother being sick or on medication (15 %) and the infant no longer wanting breast milk (12 %).
Infant formula and other breast milk substitutes
Figures 3 and 4 show the proportions of Norwegian-Somali and Norwegian-Iraqi infants who had been introduced to foods and drinks at the given age. Forty-four per cent of the Norwegian-Somali infants received infant formula the first month, 67 % at 4 months and 79 % at 6 months. Among Norwegian-Iraqi infants, the proportions that had received infant formula were 34 %, 55 % and 61 % at 1, 4 and 6 months, respectively. Fifty-eight per cent of the Norwegian-Somali infants were receiving both breast milk and infant formula at 6 months of age, while this was the case for 19 % of the Norwegian-Iraqi infants (data not shown). The rest were either breast-fed or formula-fed at 6 months of age. Water was commonly given to both groups. Among the Norwegian-Somali infants, 30 % had received water the first month, 69 % at 4 months and 93 % at 6 months. Among the Norwegian-Iraqi infants, 26 % had received water at 1 month, 76 % at 4 months and 100 % at 6 months. Sweetened drinks/fruit juices were given to 16 % of the Norwegian-Somali and 36 % of the Norwegian-Iraqi infants at 6 months of age. None of the mothers reported having introduced cow’s milk.
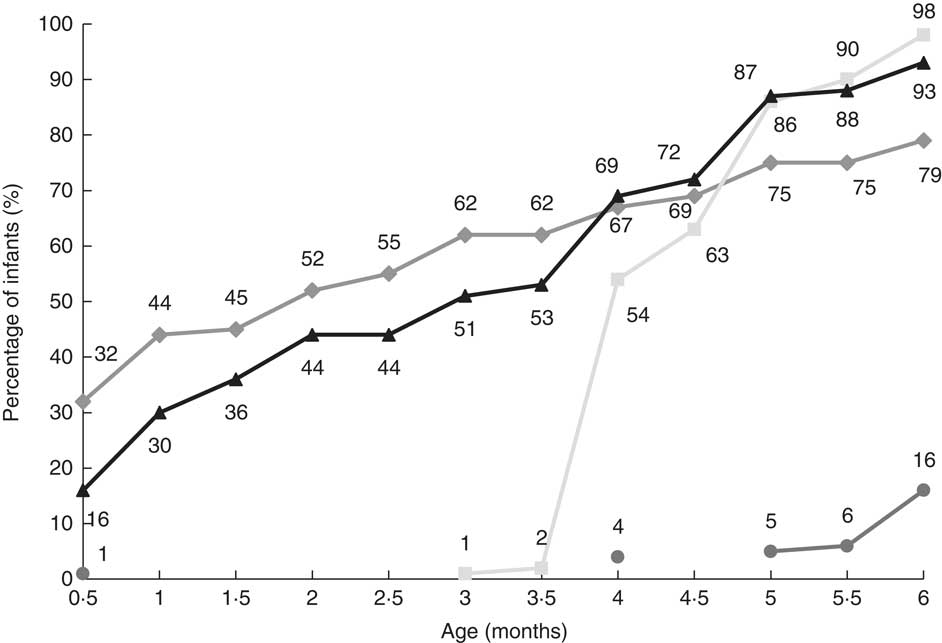
Fig. 3 Introduction of infant formula (![]() ), water (
), water (![]() ), sweetened drinks/fruit juices (
), sweetened drinks/fruit juices (![]() ) and solid and/or semi-solid foods (
) and solid and/or semi-solid foods (![]() ) to Norwegian-Somali infants during the first 6 months of life (n 107); InnBaKost survey, March 2013–February 2014
) to Norwegian-Somali infants during the first 6 months of life (n 107); InnBaKost survey, March 2013–February 2014
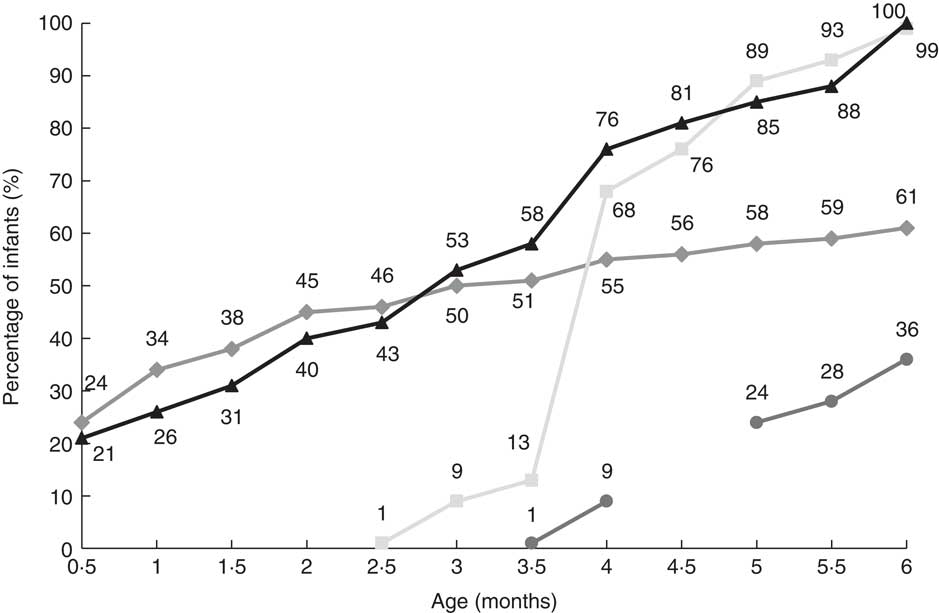
Fig. 4 Introduction of infant formula (![]() ), water (
), water (![]() ), sweetened drinks/fruit juices (
), sweetened drinks/fruit juices (![]() ) and solid and/or semi-solid foods (
) and solid and/or semi-solid foods (![]() ) to Norwegian-Iraqi infants during the first 6 months of life (n 80); InnBaKost survey, March 2013–February 2014
) to Norwegian-Iraqi infants during the first 6 months of life (n 80); InnBaKost survey, March 2013–February 2014
Solid and semi-solid foods
Two per cent of the Norwegian-Somali infants and 13 % of the Norwegian-Iraqi infants had been introduced to solid and/or semi-solid foods earlier than 4 months of age (Figs 3 and 4). At 4 months of age, 54 % of the Norwegian-Somali and 68 % of the Norwegian-Iraqi infants had been introduced to solid and/or semi-solid foods. Baby cereal was the most common solid or semi-solid food introduced. Thirty-five per cent of the Norwegian-Somali and 44 % of the Norwegian-Iraqi infants had been introduced to fruit purée/berries at this age. One-quarter of the infants had also been introduced to potatoes and vegetables in both groups. Among Norwegian-Somali infants, 7 % had been introduced to meat, 17 % to fish, 6 % to bread and 12 % to yoghurt at 5 months of age or earlier. Among the Norwegian-Iraqi infants, the proportions were 18 % for fish and 20 % each for meat, bread and yoghurt.
Data on selected foods and drinks given to the infants at 6 months of age are presented in Table 2. Baby cereal was the most commonly used food among Norwegian-Somali infants, and a higher proportion of Norwegian-Somali infants than Norwegian-Iraqi infants had received it (P<0·01). Industrially produced baby cereal was used most often and only a few reported making homemade porridge or other baby cereals in both groups. A number of foods and drinks were given to a higher proportion of Norwegian-Iraqi infants as compared with the Norwegian-Somali infants, including fruit purée/berries, squash/juice, bread, yoghurt, ice cream and cookies/cakes. Homemade dinners were given more frequently than industrially produced dinners in both groups. All Norwegian-Iraqi infants received water an average of 2·8 times daily, while 93 % of the Norwegian-Somali infants received water an average of 2·4 times daily.
Table 2 Proportion of infants receiving selected foods, drinks and supplements at 6 months of age, and frequency of consumption among users; InnBaKost survey, March 2013–February 2014
* Proportion of infants receiving ‘Baby cereal’ is not necessarily equal to the sum of the two types of baby cereals presented, because the infants could have received more than one type. This is also the case for ‘Dinner’, ‘Fruit purée/berries’, ‘Other food’, ‘Liquid’ and ‘Supplements’.
† ‘Sweetened drinks’ include squash for children 0–3 years, squash with sugar, squash artificially sweetened, soda with sugar and soda artificially sweetened. ‘Fruit juices’ include juice and nectar.
Vitamin D supplements
All Norwegian-Somali infants and 94 % of Norwegian-Iraqi infants received some kind of vitamin D supplement at 6 months of age (Table 2). Cod-liver oil was more frequently used among Norwegian-Somali infants than among Norwegian-Iraqi infants (P<0·001), while vitamin D drops were more common among Norwegian-Iraqi infants (P<0·05). Twenty per cent of the Norwegian-Somali infants started receiving vitamin D supplements before 4 weeks of age, 50 % at 4 weeks and 30 % between 5 weeks and 4 months of age. Among Norwegian-Iraqi infants receiving vitamin D supplements, 15 % started receiving supplements before 4 weeks of age, 30 % at 4 weeks and 55 % between 5 weeks and 6 months of age.
Factors associated with exclusive breast-feeding at 3·5 months of age
In the unadjusted logistic regression analyses, exclusive breast-feeding at 3·5 months of age was significantly associated with education and work before pregnancy (Table 3). Mothers with higher education were found to be more likely to exclusively breast-feed when the infant was 3·5 months of age than mothers with no or basic education. Mothers working before pregnancy were more likely to exclusively breast-feed than mothers not working before pregnancy. However, none of the factors remained significantly associated with exclusive breast-feeding at 3·5 months of age in the multivariate analysis (Table 3).
Table 3 Unadjusted and adjusted odds ratios of exclusive breast-feeding at 3·5 months of age in Norwegian-Somali and Norwegian-Iraqi infants; InnBaKost survey, March 2013–February 2014
* Number of exclusively breast-fed infants within current independent variable. Total number of infants at 3·5 months of age (n 187).
† OR and 95 % CI are adjusted for country of birth, maternal age, overall education and work before pregnancy.
‡ P values for the adjusted logistic regression model.
Factors associated with breast-feeding at 6 months of age
Country of birth, number of years lived in Norway and number of children were significantly associated with breast-feeding when the infant was 6 months of age in the unadjusted logistic regression analyses (Table 4). Country of origin and number of children remained significantly associated with breast-feeding at 6 months of age in the multivariate analysis adjusting for all other variables (Table 4). Mothers of Somali origin were more likely to breast-feed at 6 months of age than mothers of Iraqi origin. Furthermore, mothers with more than two children were more likely to breast-feed at 6 months of age than mothers with fewer children.
Table 4 Unadjusted and adjusted odds ratios of breast-feeding at 6 months of age in Norwegian-Somali and Norwegian-Iraqi infants; InnBaKost survey, March 2013–February 2014
* Number of breast-fed infants within current independent variable. Total number of infants at 6 months of age (n 187).
† OR and 95 % CI are adjusted for country of birth, maternal age, overall education, number of years lived in Norway and number of children.
‡ P values for the adjusted logistic regression model.
Discussion
The InnBaKost survey is the first survey in Norway to adapt the FFQ used in the national infant dietary survey from 2006–2007 to describe breast-feeding and other infant feeding practices among 6-month-old infants with immigrant parents. The results indicate a high prevalence of breast-feeding initiation among both Norwegian-Somali and Norwegian-Iraqi infants, but decreasing rates of exclusive breast-feeding during the first half of infancy in both groups. Continued breast-feeding up to 6 months of infant age was more common among Norwegian-Somali mothers than Norwegian-Iraqi mothers in the sample.
Breast-feeding initiation
The majority of the mothers in both study groups initiated breast-feeding. High breast-feeding initiation was also found in the Norwegian national dietary survey( Reference Kristiansen, Lande and Overby 11 ). Studies from several other countries generally report a higher initiation rate of breast-feeding among immigrant groups as opposed to non-immigrants( Reference Castro, Layte and Kearney 14 , Reference Santorelli, Petherick and Waiblinger 16 , Reference van Rossem, Vogel and Steegers 17 , Reference Rio, Castello-Pastor and Del Val Sandin-Vazquez 23 ), although not necessarily for all subgroups( Reference Rio, Castello-Pastor and Del Val Sandin-Vazquez 23 ). However, in these countries, breast-feeding initiation rates are much lower among the non-immigrant populations than among Norwegian-born mothers( Reference Kristiansen, Lande and Overby 11 ).
Breast-feeding initiation seems to vary between Somalia and Iraq, the countries of origin for the mothers in our study. There is a paucity of recent quantitative studies on breast-feeding practices in Somalia. One qualitative knowledge, attitude and practices (KAP) study described that only a small proportion of mothers initiated breast-feeding within the first hour and that initial breast-feeding usually took place 2–3 d after birth( 24 ). In Iraq, a nationwide household survey reported that 73 % of mothers initiated breast-feeding early after delivery( Reference Abdul Ameer, Al-Hadi and Abdulla 25 ).
Colostrum was reportedly fed to the majority of infants in the present study. Information on colostrum was not captured in the Norwegian national dietary survey. According to the KAP study from Somalia, colostrum was usually fed to less than 30 % of the children living in the different areas, as it was often considered heavy, thick and harmful to the child’s health( 24 ). A qualitative study from the USA also reported mixed attitudes among Somali mothers. Some, but not all, held on to the Somali belief that feeding colostrum makes the baby sick and they therefore postponed breast-feeding until several days after birth( Reference Steinman, Doescher and Keppel 26 ). In the nationwide study from Iraq, however, almost 93 % of the participating women considered colostrum to be good for their children( Reference Abdul Ameer, Al-Hadi and Abdulla 25 ).
Exclusive breast-feeding and breast-feeding practices
Duration of exclusive breast-feeding was shorter both among Somali-born and Iraqi-born mothers than the 6 months that is currently recommended in Norway( 7 , 8 ). Less than half of the Norwegian-Somali and Norwegian-Iraqi infants were exclusively breast-fed at 1 month and only 7 % and 10 %, respectively, were exclusively breast-fed at 4 months of age. Only one Iraqi infant was exclusively breast-fed up to 6 months of age (i.e. at 5·5 months of age) and none were exclusively breast-fed at 6 months of age in either study group.
In comparison, data on infants from the Norwegian national survey from 2006–2007 showed a high level of exclusive breast-feeding during the first 3 months of life, with 84 % of the infants being exclusively breast-fed at 1 month of age and 48 % at 4 months, declining to 10 % at 6 months( Reference Kristiansen, Lande and Overby 11 ). These findings were consistent with earlier national data from Norway( Reference Lande, Andersen and Baerug 10 ) and the more recent national survey from 2013( Reference Lande and Helleve 12 ). Thus, the rates of exclusive breast-feeding are appreciably lower among these two immigrant groups compared with the non-immigrant population in Norway.
Findings from Denmark have also suggested higher rates of exclusive breast-feeding among women of Nordic origin compared with immigrants and descendants of immigrants( Reference Busck-Rasmussen, Villadsen and Norsker 27 ). According to those findings, 50 % of mothers who had migrated from Iraq were fully breast-feeding for 4 months. The higher rates of full breast-feeding compared with our findings are probably due to the definition of full breast-feeding in the Danish study, which was infants receiving breast milk exclusively, supplemented by water or a maximum of one meal of formula per week. In England, on the other hand, rates of exclusive breast-feeding in women of immigrant background (except Pakistani) were double those of white British women( Reference Santorelli, Petherick and Waiblinger 16 ). These findings are, however, probably not quite transferable to our setting, since the prevalence of exclusive breast-feeding and breast-feeding overall is much lower in the UK and most other European countries than in Scandinavian countries( Reference Ibanez, Martin and Denantes 9 ).
The prevalence of exclusive breast-feeding also appears to be low in the country of origin of the two study groups. In the nationwide household survey from Iraq, 38 % of the sample reported that they knew what exclusive breast-feeding was, but only about half of these women defined it correctly and reported that exclusive breast-feeding should continue for 6 months postpartum( Reference Abdul Ameer, Al-Hadi and Abdulla 25 ). The KAP study from Somalia found that exclusive breast-feeding did not exist in many areas of the country, as breast milk alone was considered to be inadequate for the child( 24 ). Similar findings have been reported among immigrant mothers in other qualitative studies conducted in the USA and the UK( Reference Steinman, Doescher and Keppel 26 , Reference Ingram, Cann and Peacock 28 ).
Breast-feeding cessation was more likely to occur at an earlier age among Iraqi-born than Somali-born mothers. Only 58 % of the Iraqi-born mothers were still breast-feeding at 6 months of age, whereas this was the case for 79 % of the Somali-born mothers. The latter figure is similar to the 82 % of mothers still breast-feeding at 6 months, as reported in the Norwegian national survey( Reference Kristiansen, Lande and Overby 11 ). Other studies have reported various breast-feeding patterns among immigrant groups in different countries( Reference Santorelli, Petherick and Waiblinger 16 – Reference Dennis, Gagnon and Van Hulst 18 ). Studies from Somalia and Iraq have furthermore described that breast-feeding is seen as acceptable for mothers, their networks and professionals, but lack of knowledge, inappropriate beliefs and very close birth-spacing (a new sibling before the child reached 2 years of age) were the major obstacles for optimal breast-feeding practices( 24 , Reference Abdul Ameer, Al-Hadi and Abdulla 25 , Reference Al-Zwaini, Al-Haili and Al-Alousi 29 , Reference Al-Nassaj, Al-Ward and Al-Awqati 30 ).
Complementary feeding practices
Both infant formula and water had been introduced to more than half of the Norwegian-Somali and Norwegian-Iraqi infants during the first 3 months of life. On the positive side, none of the infants had been introduced to cow’s milk. The proportions of infants receiving formula and water were much higher compared with the Norwegian national survey, which showed that 28 % had been introduced to formula and 22 % to water in the same age group( Reference Øverby, Kristiansen and Andersen 21 ).
The KAP study from Somalia identified that water with sugar and milk were considered fundamental constituents of infants’ complementary diets, and children were mainly fed cow’s or goat’s milk in addition to breast-feeding from birth to 3 months of age( 24 ). Furthermore, concerns about adequate infant weight gain, advice from family members/community and lack of knowledge have been reported by Steinman et al. to be the main reasons for early supplementation with formula among Somali mothers in the USA( Reference Steinman, Doescher and Keppel 26 ). Early introduction of formula may compromise breast-feeding, as breast-feeding is a supply-and-demand system and introduction of formula could lead to decreased infant demand for breast milk, thereby decreasing the supply( Reference Holmes, Auinger and Howard 31 ). In order to increase exclusive breast-feeding and breast-feeding rates during the first months of life among these two groups, these aspects may be important to emphasize and communicate, as insufficient milk and the infant no longer wanting breast milk were two of the frequently reported reasons for breast-feeding cessation. Although Norway is known for its extensive and positive breast-feeding tradition and support system, more culture-specific information and support, and teaching of correct attachment and positioning of the baby during breast-feeding, may contribute to solve these problems.
Very few (2 %) of the Norwegian-Somali infants received solid or semi-solid foods before 4 months of age, whereas 13 % of the Norwegian-Iraqi infants did so, similar to the 11 % reported in the Norwegian national survey( Reference Øverby, Kristiansen and Andersen 21 ). The differences were greater at 4 months, when 54 % of the Somali infants and 68 % of the Iraqi infants were introduced to solid or semi-solid food, compared with approximately 40 % in the Norwegian national survey( Reference Øverby, Kristiansen and Andersen 21 ). Similar to findings in the present study, porridge (87 %) and fruit and berries (80 %) were the main foods given at 6 months of age in the Norwegian national survey( Reference Øverby, Kristiansen and Andersen 21 ). Dinners were given to 59 % of the infants and industrial dinners were more frequently used than homemade in the Norwegian national survey( Reference Øverby, Kristiansen and Andersen 21 ), which is the opposite of the findings in the present study. This may be due to concerns about lack of freshness of commercially prepared baby foods and the practice of feeding the child the same foods as adults among our sample, which have been reported in other studies( Reference Steinman, Doescher and Keppel 26 ). The use of bread, yoghurt, sweets, sweetened drinks and juices was much more frequent among Norwegian-Iraqi infants than among Norwegian-Somali infants in the present study, whereas the reported use of these foods was limited in the Norwegian national survey (0–10 %)( Reference Øverby, Kristiansen and Andersen 21 ). The earlier introduction and more frequent use of foods in general may be explained by the lower breast-feeding prevalence, which has also been described by Griffiths et al.( Reference Griffiths, Tate and Dezateux 32 ), and concerns about adequate infant weight gain, as discussed earlier. The consumption of yoghurt or other dairy products, however, is not recommended before 10 months of age( 8 ), as these contain no Fe and may therefore replace Fe-rich foods and increase the risk of Fe deficiency. Furthermore, sugar-sweetened beverages and energy-dense foods have been identified as dietary risk factors for childhood obesity( Reference Barlow 33 ) and may cause caries( Reference Alm, Wendt and Koch 34 ). The consumption of these foods and beverages should thus be limited.
Vitamin D supplements
Most infants in the present study received vitamin D supplementation at 6 months of age. Vitamin D supplementation was also widely used among infants in the Norwegian national survey( Reference Øverby, Kristiansen and Andersen 21 ). This is a positive finding, as the prevalence of vitamin D deficiency often is higher among immigrant populations in Europe compared with the indigenous populations of the countries to which they have migrated( Reference van der Meer, Middelkoop and Boeke 35 ). All infants in Norway are recommended to receive vitamin D supplementation from 4 weeks of age( 8 ).
Factors associated with exclusive breast-feeding
Although higher education and work before pregnancy among mothers were positively associated with exclusive breast-feeding at 3·5 months of age in the unadjusted logistic regression analyses, none of the factors were found to be significantly associated with exclusive breast-feeding in the multivariate analysis. In comparison, the Norwegian national survey found that exclusive breast-feeding at 4 months increased with maternal educational level and number of children( Reference Kristiansen, Lande and Overby 11 ). The study found a negative association between exclusive breast-feeding and maternal smoking and no association with maternal age, paternal education and geographical region( Reference Kristiansen, Lande and Overby 11 ). Similarly, in Denmark, the likelihood of being fully breast-fed among Nordic infants increased with maternal age and parity and was higher among women with a high socio-economic position, while the pattern was less clear for infants of all other immigrant groups( Reference Busck-Rasmussen, Villadsen and Norsker 27 ). There was, however, a tendency of less fully breast-feeding the longer the migrant had lived in Denmark before the delivery and the younger the mother had been when she immigrated to Denmark, suggesting that acculturation did not favour breast-feeding( Reference Busck-Rasmussen, Villadsen and Norsker 27 ). This was not observed in our study.
Factors associated with breast-feeding
Differences in breast-feeding patterns among immigrant groups have been described by many( Reference Santorelli, Petherick and Waiblinger 16 , Reference van Rossem, Vogel and Steegers 17 , Reference Thulier and Mercer 36 ), and this was also found in the present study where Somali-born mothers were more likely to breast-feed when the infant was 6 months of age than Iraqi-born mothers. Our findings showed increased odds of breast-feeding among mothers with more than two children, while the Norwegian national survey found no consistent pattern between breast-feeding at 6 months and parity( Reference Kristiansen, Lande and Overby 11 ). The literature is inconsistent on the association between breast-feeding and parity( Reference Dennis, Gagnon and Van Hulst 18 , Reference Thulier and Mercer 36 ); a study by Dennis et al. reported an increased odds of continuing to breast-feed with number of children (≥3) among Canadian-born women, whereas being primiparous was associated with increased breast-feeding duration among immigrant mothers( Reference Dennis, Gagnon and Van Hulst 18 ).
Strengths and weaknesses of the study
Although the response rate was less than 30 % in both groups, the present study provides unique data on breast-feeding and complementary feeding practices among two very specific subgroups of the population based in three Norwegian counties. Challenges in recruitment of immigrant populations for dietary surveys have been reported by many( Reference Garduno-Diaz, Husain and Ashkanani 37 , Reference Ngo, Gurinovic and Frost-Andersen 38 ) and extra time and effort in recruiting and sampling are often needed due to limited numbers of people in the target sample frame. Convenience sampling method is often used as the standard approach in ‘hard-to-sample’ population subgroups.
The proportions of participants from each county were almost the same as those estimated in the National Population Register, which reported that 75 % of the Somali-born mothers listed lived in Oslo, 12 % in Akershus and 13 % in Buskerud. Among the Iraqi-born mothers, 53 % lived in Oslo, 33 % in Akershus and 14 % in Buskerud. The use of bilingual information letters and fieldworkers during recruitment and in the interview situations made it possible for non-Norwegian-speaking mothers to participate. However, mothers who were approached through several channels (e.g. reached at a registered telephone number and/or visited at their home address) were more likely to be included than those who only received the information letter.
There is a potential for recall bias, as data on breast-feeding and infant feeding were collected retrospectively. These data were collected no more than 6 months after breast-feeding cessation and according to a review by Li et al., mothers in many populations studied seem to provide accurate estimates of the initiation and duration of breast-feeding when reported within a 3-year period( Reference Li, Scanlon and Serdula 39 ). However, the validity and reliability of maternal recall for the age of introduction of foods and liquids other than breast milk seem to be less accurate( Reference Li, Scanlon and Serdula 39 ).
The multivariate analyses presented in the current paper explore only a few selected factors that might potentially be associated with exclusive breast-feeding and breast-feeding practices. It is likely that social or other factors not measured in the study also may influence breast-feeding practices. A small sample size limits extensive multivariate analyses in the study. More research is therefore needed to better understand inequalities in breast-feeding practices.
Additionally, as breast-feeding patterns can be influenced by several factors, including country of residence and acculturation, the study cannot be generalized to other immigrant groups in Norway or to immigrant populations residing in other countries.
Conclusion
Breast-feeding initiation was common among both Somali-born and Iraqi-born mothers, but exclusive breast-feeding duration was shorter than recommended in both groups. Although both exclusive breast-feeding and breast-feeding overall are considered to be common in Norway, findings from the present study reveal some disparities in breast-feeding and complementary feeding practices for immigrant subgroups in the population. The study further suggests that there may be value in developing targeted approaches to ensure support for exclusive breast-feeding and breast-feeding by foreign-born mothers in order to achieve equity in breast-feeding and complementary feeding practices among Norwegian-born and Norwegian-immigrant mothers.
Acknowledgements
Acknowledgements: The authors would like to thank the fieldworkers who assisted with the data collection, as well as the mothers who participated in the study. Financial support: This study has been supported and financed by the Norwegian Research Council (grant number 213460/H10) and further by the Canada Research Chair and Canadian Foundation for Infrastructure Programs, the University of Oslo and Oslo and Akershus University College. The funders had no role in the design, analysis or writing of this article. Conflict of interest: The authors declare no conflict of interest. Authorship: N.K.G. participated in designing the study and data collection, carried out the data analysis and wrote the manuscript. L.F.A., A.M. and L.E.T. participated in the study design and provided advice during all stages of the work, including the drafting and editing of the manuscript. D.S. assisted in and contributed to the analytic plan and interpretation of the results and the editing of the manuscript. All authors read and approved the final manuscript. Ethics of human subject participation: The study was approved by the Regional Committees for Medical and Health Research Ethics and informed consent was obtained from the participating mothers.











