Suboptimal feeding practices in infancy and childhood have led to the high prevalence of malnutrition, increased morbidity and mortality in children in the developing world. It has been found that non-exclusive breast-feeding (EBF) in the first 6 months of life results in 1·4 million deaths and 10 % of the disease burden in children younger than 5 years(Reference Black, Allen and Bhutta1). It is also estimated that the death of about 10–15 % of infants <5 years old in resource-poor countries could be prevented through the achievement of 90 % coverage with EBF alone(Reference Jones, Steketee and Black2), and about 22 % of neonatal deaths could be prevented if breast-feeding started within the first hour of birth(Reference Edmond, Zandoh and Quigley3).
In keeping with the Millennium Development Goals, countries in the developing world have committed to reduce the mortality rate in <5-year-olds by two-thirds between 1990 and 2015(4). Appropriate feeding of infants and young children is one of the feasible interventions in child survival programmes addressing this goal. The WHO infant feeding guidelines recommend that infants should be exclusively breast-fed for the first 6 months of life to achieve optimal growth, development and health(5). Thereafter, to meet their evolving nutritional requirements, infants should receive nutritionally adequate and safe complementary foods while breast-feeding continues for up to 2 years of age or beyond. Breast-feeding should be initiated within the first hour of birth, and no other pre-lacteals or bottle-feeds should be given to the infant.
Breast milk provides almost all the necessary nutrients, growth factors and immunological components for a healthy infant(Reference Leung and Sauve6). Appropriate breast-feeding has proven effective in reducing the incidence and severity of gastrointestinal and respiratory infections(Reference Arifeen, Black and Antelman7–Reference Senarath, Dibley and Agho11). Other advantages of breast-feeding include the enhancement of cognitive development(Reference Richards, Hardy and Wadsworth12, Reference Temboury, Otero and Polanco13), and prevention of allergies, obesity, hypertension and insulin-dependent diabetes mellitus. Health gains for breast-feeding mothers include lactational ameonorrhea, early involution of the uterus, enhanced bonding between the mother and the infant and reduction in the incidence of ovarian and breast cancer(Reference Leung and Sauve6). From an economic perspective, breast-feeding is less expensive than breast milk substitutes(Reference Leung and Sauve6).
Despite numerous recognized advantages over artificial feeding, breast-feeding rates in most countries are typically low, and have only slowly improved. According to estimates between 1995 and 2003, only 38 % of infants in the developing world were exclusively breast-fed for the first 6 months(14). Demographic and Health Surveys (DHS), Multiple Indicator Country Surveys (MICS) and national nutritional surveys (NNS) from East Asian countries provide information on infant and child feeding practices at a national level; however, there is limited information regarding cross-country comparisons of breast-feeding indicators in the region. A previous group has compiled an infant and young child feeding update using available key indicators from the DHS reports of countries around the world. However, this update includes only three countries – Cambodia, Indonesia and Philippines from the East Asian region(Reference Mukuria, Kothari and Abderrahim15). In East Asia and Southeast Asia it is important to estimate all possible feeding indicators as recommended by the WHO, with a view of recognizing the countries and practices that need further intervention. A cross-country comparison has the advantage of describing variations in different dimensions of breast-feeding across countries. Such an analysis would help individual countries to identify the aspects of breast-feeding that deserve priority in their breast-feeding promotion programmes. The aim of this secondary data analysis was to assess and compare infant and young child feeding practices across nine East and Southeast Asian countries using the key indicators recommended by the WHO(16).
Methods
Data sources
Our analysis was based mainly on available data sets of DHS and MICS collected between 2000 and 2005 in the East and Southeast Asian regions. DHS data were available for five countries – Indonesia 2002–2003(17), Philippines 2003(18), Timor-Leste 2003(19), Cambodia 2001 and 2005(20) and Vietnam 2002(21). Since these data, except Cambodia, were collected between 2002 and 2003, we assumed that the feeding practices remained relatively unchanged over the 2-year period. For Cambodia, only the 2005 data were used for the cross-country comparisons since our aim was to present the latest available data within the specified period. MICS data were available for Lao People’s Democratic Republic (Lao PDR)(22) and Myanmar(23) in 2000. There has been no DHS or MICS in the Democratic People’s Republic of Korea (DPR Korea). Data from the 2002 National Nutrition Survey with similar variables to those used in the DHS surveys were used(24). Similarly in Mongolia, the data from the 2002 National Nutrition Assessment were used, although it does not include all the variables available in other data sets(25). All these surveys were nationally representative households surveys in which married women of reproductive age were interviewed by trained investigators.
The MICS programme developed by UNICEF assists countries in filling data gaps for monitoring the situation of children and women through statistically sound, internationally comparable estimates of socio-economic and health indicators. MICS are typically carried out by government organizations, with the technical support and financial assistance of UNICEF and its partners. UNICEF provides technical support and training through a series of regional workshops covering questionnaire content, sampling and survey implementation, data processing, data quality and data analysis, and report writing, data archiving and dissemination.
The relevant public domain data sets were downloaded and inspected for quality of data, completeness of information and comparability of variables required for the analysis. The required variables from each data set were selected and files were constructed for each country. These were merged into a central database with the data from all countries. The analysis was confined to the last born child aged 0–23 months living with the respondent. The details of survey methodology, sampling procedure and questionnaires are available in the respective DHS, MICS or NNS reports.
Feeding indicators
Infant feeding indicators were estimated according to the key breast-feeding and selected complementary-feeding indicators described by the WHO in 1991(16). The estimated indicators were timely first-suckling rate, ever breast-fed rate, current breast-feeding rate, continued breast-feeding rate at 12–15 and 20–23 months, EBF rate, predominant breast-feeding rate, full breast-feeding rate, bottle-feeding rate, timely complementary-feeding rate and the median duration of breast-feeding. Timely first-suckling rate was based on mother’s response to the question how soon after the birth was the child given breast milk, and ever breast-fed rate whether the child was given breast milk at least once at any time since birth. All other indicators were based on 24 h recall by the mother. The timely complementary-feeding rate was calculated using a method proposed in earlier recommendations by the WHO(16).
Data analysis
Analyses were performed using the Stata statistical software package version 9·0 (Stata Corp., College Station, TX, USA) with ‘Svy’ commands to allow for adjustments for the cluster sampling design used in the surveys when estimating 95 % CI around prevalence estimates. A weighted total of 23 702 children were included from the nine countries.
Results
Basic characteristics of the samples
Basic characteristics of the DHS and non-DHS (MICS and NNS) samples included in the study are summarized in Tables 1 and 2, respectively. The sample sizes ranged from 826 to 5610 for the DHS data, and from 477 to 5860 for non-DHS data sets. In all the data sets, both male and female infants and 6-month age categories were almost equally represented. The Mongolian sample did not include infants less than 6 months of age.
Table 1 Individual, household and community level characteristics of children 0–23 months of age, for five DHS surveys

DHS, Demographic and Health Survey; TBA, traditional birth attendant.
Table 2 Individual, household and community level characteristics of children at 0–23 months of age, for MICS and other surveys

MICS, Multiple Indicator Country Survey; Lao PDR, Lao People’s Democratic Republic; DPR Korea, Democratic People’s Republic of Korea; TBA, traditional birth attendant.
Among the DHS samples (Table 1), the proportion of mothers who had secondary or a higher level of education was low in Cambodia (16 %) and Timor-Leste (27 %), intermediate in Indonesia (50 %) and high in Vietnam (67 %) and the Philippines (70 %). Vietnam had a very high working mother population (81 %) when compared with the other countries. More than 88 % of mothers had made at least one antenatal clinic visit during the pregnancy in Indonesia, Philippines and Vietnam. The trained assistance at delivery ranged from 16 % in Timor-Leste to 75 % in Vietnam. Almost 47 % of mothers in Cambodia did not have any postnatal checkup, whereas the corresponding rate for Vietnam was 6 %. The proportion of women who participated in decision making for all of the five household decisions enquired by the survey was 58 % in the Philippines, 64 % in Indonesia and 72 % in Timor-Leste. According to mothers’ perceptions, approximately 42–75 % of the children from these countries were of average size at birth. Timor-Leste, Vietnam and Cambodia had predominantly rural households, whereas Indonesia and Philippines were distributed equally between urban and rural populations.
Limited information was available in the non-DHS samples (Table 2). The proportion of mothers who had secondary or a higher level of education ranged from 17 % in Lao PDR to 76 % in DPR Korea. Information on birth attendance was available only for Lao PDR and DPR Korea. The trained attendance was poor for both (20 % and 13 %, respectively). Myanmar, Mongolia and Lao PDR had above 60 % rural households, whereas in the DPR Korea 59 % were from urban households. According to mothers’ perceptions, approximately 70–90 % of these children were of average size at birth.
Feeding indicators across the countries
Tables 3 and 4 illustrate the estimated breast-feeding indicators for the nine East Asian countries included in the present study. More than 90 % of the infants were ever breast-fed in all the countries under study, except in the Philippines, where the rate was 88 %. Almost all infants in Myanmar and Lao PDR were ever breast-fed. Information on timely initiation of breast-feeding was mainly limited to the five DHS and these rates varied from 32 % in Indonesia to 46 % in Timor-Leste.
Table 3 Timely first-suckling, ever breast-fed, current breast-feeding and continued breast-feeding rates in East and Southeast Asian countries (2000–2005)

Lao PDR, Lao People’s Democratic Republic; DPR Korea, Democratic People’s Republic of Korea.
*For Mongolia, data were available for children at 6–23 months of age.
Table 4 Exclusive breast-feeding, predominant breast-feeding, full breast-feeding, bottle-feeding and timely complementary-feeding rates in East and Southeast Asian countries (2000–2005)

Lao PDR, Lao People’s Democratic Republic; DPR Korea, Democratic People’s Republic of Korea.
*For Mongolia, data were available for children at 6–23 months.
When compared with other countries the current breast-feeding rate among children aged 0–23 months was found to be significantly lower in the Philippines (59 %). The current breast-feeding rates fell between 70 % and 80 % for Timor-Leste, Vietnam and DPR Korea, and between 80 % and 90 % for Indonesia, Cambodia, Lao PDR, Myanmar and Mongolia. The pattern of continued breast-feeding rate at 12–15 months in each country was very similar to the country’s current breast-feeding rate, but the continuation rate declined by about 30–40 % when the child reached 20–23 months. However, countries such as Myanmar (67 %), Indonesia (59 %), Cambodia (54 %) and Mongolia (66 %) sustained higher rates of continuation even at 20–23 months.
The EBF rate in infants of less than 6 months of age varied from 11 % in Myanmar to 60 % in Cambodia (Table 4). Lower EBF rates were reported in Vietnam (16 %) and Lao PDR (23 %). The rates in Indonesia, Philippines and Timor-Leste were between 30 % and 40 %. As shown in Fig. 1, the proportion of infants aged <6 months who were given breast milk together with non-milk liquids (predominantly breast-fed) was high except in Indonesia and Timor-Leste.
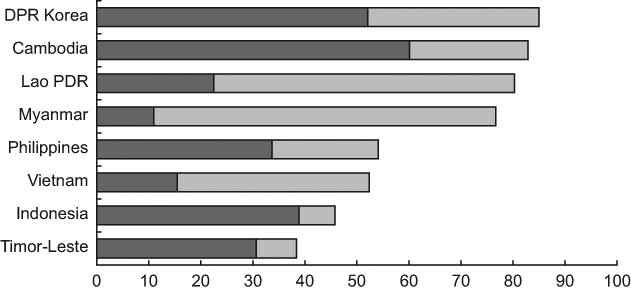
Fig. 1 Percentage of infants <6 months of age who were exclusively breast-fed (![]() ) or received breast milk with non-milk liquids, i.e. predominant breast-feeding (
) or received breast milk with non-milk liquids, i.e. predominant breast-feeding (![]() ), across East and Southeast Asian countries (2000–2005) (DPR Korea, Democratic People’s Republic of Korea; Lao PDR, Lao People’s Democratic Republic)
), across East and Southeast Asian countries (2000–2005) (DPR Korea, Democratic People’s Republic of Korea; Lao PDR, Lao People’s Democratic Republic)
Lower bottle-feeding rates were reported in DRP Korea (3 %), Lao PDR (6 %) and Myanmar (6 %). Higher bottle-feeding rates were reported in Philippines (49 %), Mongolia (31 %), Indonesia (23 %) and Vietnam (21 %). With respect to timely complementary feeding, the rate was more than 60 % in the majority of the countries. However, there was a wide variation between countries. For example, it was as low as 6 % in Myanmar and 10 % in Lao PDR, and as high as 99 % in Mongolia.
Discussion
Early initiation of breast-feeding has proven benefits(Reference Edmond, Zandoh and Quigley3), thus we recommend that all the countries should make greater efforts to improve the practice of initiation of breast-feeding within the first hour of birth. Very high ever breast-fed rates across the region indicate that breast-feeding is universal in the East and Southeast Asian region. The proportion of currently breast-fed was also high, especially during the first year of life. These observations are favourable indications as far as breast-feeding promotion is concerned, and warrant the need to focus on aspects such as timeliness, exclusiveness and continuity of breast-feeding. According to WHO recommendations, breast-feeding should be continued through the second year(5). The present analysis revealed that, in all nine countries studied, the majority of mothers continued breast-feeding beyond the first year. However, it is important to take measures to sustain this rate until the end of the second year.
The EBF rates in all the countries should be improved in order to gain the full benefits of EBF that ultimately lead to a reduction in deaths among infants <5 years old(Reference Jones, Steketee and Black2). This could be achieved through breast-feeding promotion programmes by highlighting the importance of giving breast milk alone, and nothing else including plain water. It is important to note that even though EBF is low, a very high proportion of infants in countries like Lao PDR and Myanmar were fed with non-milk liquids in addition to breast milk. Hence, breast-feeding (giving only breast milk or breast milk and water) was high in Cambodia, Lao PDR and Myanmar despite low EBF. In contrast, the practice of giving non-milk liquids in Indonesia and Timor-Leste was minimal. The countries that reported very low EBF such as Myanmar, Vietnam and Lao PDR could make a substantial improvement in the EBF rate by avoiding the practice of giving water or other non-milk liquids in addition to breast milk.
Bottle-fed infants are at a higher risk of having infections and lower cognitive capacity(Reference Dewey, Heinig and Nommsen-Rivers8, Reference Temboury, Otero and Polanco13). It is important to adopt policies and practices to avoid the use of feeding bottles in infants unless medically indicated. Countries with high bottle-feeding rates such as the Philippines, Mongolia, Indonesia and Vietnam should identify target groups, i.e. socio-economically better-off women, in order to change the practice of bottle-feeding. Bottle-feeding rates rise with the socio-economic development. Countries with lower bottle-feeding rates, such as Lao PDR, Myanmar and DPR Korea, should try to sustain these low rates.
Lao PDR and Myanmar will need to educate families about the introduction of solid or semi-solid feeds to infants from 6 to 9 months. Although the timelines are satisfactory in many countries, these findings should be carefully interpreted with consideration to the adequacy and quality of feeds given to infants. A timely complementary-feeding rate based on 24 h dietary recall does not actually reflect the timing of the introduction of complementary food, because it can include those who have started complementary feeding even before the sixth month. In addition, this indicator alone is insufficient to comment about the adequacy of feeding frequency, energy density and quality of the diet, including sufficient micronutrients.
The main strengths of the present study were the nationally representative samples, the comprehensive data on standard infant feeding indicators and the appropriate adjustments for sampling design made in the analysis. One limitation would be the subjectivity of information in recalling the time of first suckling especially among mothers of older infants. This study was restricted to a description of the breast-feeding indicators at a national level. However, it is important to observe the variation of each indicator across different individual, household and community characteristics in the respective country. It is also important to identify the significant predictors of poor practices in each country. Such information would help the respective countries to target women for breast-feeding promotion programmes.
The main limitation of this comparison is the different years the surveys were conducted between 2000 and 2005. The infant and young child feeding practices could have changed in some countries due to programmatic activities or for other reasons. For example, in Cambodia there were remarkable improvements in many of the feeding indicators between 2000 and 2005 related to new infant and young child feeding programmes conducted by the Ministry of Health with support from UNICEF(20, 26). Similarly, caution should be taken when comparing data from different types of surveys – DHS, MICS and other national nutrition surveys. However, the questions used in the DHS and MICS surveys for infant feeding indicators were almost identical and the greatest differences in the manner the data were collected were found with the national nutrition surveys, e.g. the data available from Mongolia were for children 6–23 months of age, which prevented calculation of a number of indicators including exclusive and predominant breast-feeding rates.
In conclusion, all the countries should make greater efforts to improve the practice of initiation of breast-feeding within the first hour of birth. The EBF rates in all the countries should be improved by emphasizing the importance of giving breast milk alone and nothing else, including plain water, during the first 6 months of life. Countries with higher bottle-feeding rates should identify those groups at risk of bottle-feeding in order to implement targeted interventions. Further analysis would be required to disaggregate each indicator by different individual, household and community characteristics and to identify the significant predictors of poor practices in each country.
Acknowledgements
The financial support for the study was provided by the UNICEF East Asia/Pacific under the agreement SSA/THLA/2006/00000422-0. The views expressed in this publication do not necessarily reflect those of UNICEF. The authors declare that there is no conflict of interests. M.J.D. generated the concept of study, designed the plan of analysis and edited the manuscript. U.S. compiled the tables and prepared the manuscript. K.E.A. downloaded the data and conducted the data analysis. The authors thank Dr Milana Votrubec of the University of Sydney for English language editing of the manuscript.







