Globally, childhood undernutrition is one of the most important public health challenges. When considering all causes of under-5s mortality worldwide, it is estimated that 35 % of these deaths are attributable to malnutrition(Reference Black, Allen and Bhutta1). The critical ‘window of opportunity’ for child growth is in the first 2 years of life; recent analyses have found that the effect of growth faltering during this period is more severe than previously thought(Reference Victora, de Onis and Hallal2). In this critical period for the growth of children under 2 years of age, it is essential to ensure proper nutrition. According to the UNICEF conceptual framework for child nutrition(Reference Pelletier3), both dietary intake and health care are critical determinants of child undernutrition.
Aspects of infant and young child feeding (IYCF) that are important in the first 2 years of life include: early initiation of breast-feeding; exclusive breast-feeding for the first 6 months of life; adequate, timely and appropriate complementary feeding from 6 to 24 months of age; continued breast-feeding after the introduction of complementary foods; adequate dietary diversity in complementary foods; and adequate frequency of meals. A large body of research was conducted over almost a decade, to hone in on the most critical IYCF practices and to derive globally accepted indicators for capturing the range and quality of these IYCF practices(Reference Dewey, Cohen and Rollins4–Reference Arimond, Daelmans and Dewey9). The WHO-recommended indicators of IYCF practices were an outcome of this process, and the currently recommended indicators include both core and optional indicators that can be used to measure these practices in population-based surveys(8).
Previous studies have investigated the relationship between IYCF practices and child growth. In a study using data from five countries in Latin America, a significant association was found between better child feeding practices (which included breast-feeding, appropriate use of complementary foods, feeding frequency and the diversity of the diet) and nutritional status among children 12–36 months of age(Reference Ruel and Menon10). That study established a young child feeding index that has subsequently been adapted to test the relationship between child feeding practices and child growth in multiple settings including rural Senegal(Reference Ntab, Simondon and Milet11), Burkina Faso(Reference Sawadogo, Martin-Prevel and Savy12), rural India(Reference Garg and Chadha13), urban Madagascar(Reference Moursi, Treche and Martin-Prevel14) and rural China(Reference Zhang, Shi and Wang15). One longitudinal study in Bangladesh constructed an infant feeding scale and found that children who scored higher on the infant feeding scale were more likely to have better growth later in infancy. Although that study was able to capture many of the core infant feeding practices outlined by the WHO in their scale, the relationship between food variety and child growth could not be evaluated due to lack of adequate data on foods fed to children(Reference Saha, Frongillo and Alam16).
While these studies have used composite infant feeding scales and indices that captured many of the WHO-recommended IYCF practices, many other studies have focused only on the relationship between specific aspects of IYCF and child growth. For example, the association between breast-feeding practices and child growth has been investigated in a number of settings: Bangladesh(Reference Giashuddin, Kabir and Rahman17, Reference Arifeen, Black and Caulfield18), Malawi(Reference Kalanda, Verhoeff and Brabin19), Brazil(Reference Victora, Morris and Barros20, Reference Spyrides, Struchiner and Barbosa21), Columbia(Reference Alvarado, Zunzunegui and Delisle22), Turkey(Reference Gokcay, Turan and Partalci23), rural Senegal(Reference Simondon, Simondon and Costes24) and Mexico(Reference Eckhardt, Rivera and Adair25, Reference Villalpando and Lopez-Alarcon26). Additionally, the appropriate introduction of complementary foods (both timing and type) and associations with child growth have been studied in Malawi(Reference Kalanda, Verhoeff and Brabin19, Reference Espo, Kulmala and Maleta27), Vietnam(Reference Hop, Gross and Giay28), Barbados(Reference Galler, Ramsey and Harrison29) and Senegal(Reference Simondon and Simondon30).
Another IYCF practice that has been well studied is dietary diversity, which is recognized as important in enabling children 6–24 months of age to achieve adequate nutrient density in their diet(Reference Kant31–Reference Hoddinott and Yisehac36). Previous studies have examined the association between dietary diversity and anthropometric measures of nutritional status in countries of Africa, South Asia, South-East Asia and Latin America/Caribbean. Using Demographic and Health Survey (DHS) data from these regions, chronic undernutrition was found to be significantly associated with dietary diversity(Reference Arimond and Ruel37). Significant and positive associations between dietary diversity and nutritional status among young children have also been found in smaller-scale studies in rural Bangladesh(Reference Rah, Akhter and Semba38), rural Burkina Faso(Reference Sawadogo, Martin-Prevel and Savy12), Kenya(Reference Onyango, Koski and Tucker39), Mexico(Reference Allen, Black and Backstrand40) and Mali(Reference Hatloy, Hallund and Diarra41), and in a review in Africa(Reference Onyango35).
The relationships between the newly established WHO-recommended IYCF indicators with nutritional outcomes have not been previously examined using national-level data from Bangladesh. The present research applied the newly established indicators to nationally representative data, to study and illustrate the associations between IYCF practices and growth in Bangladeshi children.
Materials and methods
Survey data from the 2007 DHS in Bangladesh were used. The DHS is a nationally representative household survey that is available for public use(42). Data from the children's re-coded data set, which contains one record for every child of eligible women who were born in the last 5 years (0–59 months of age), were adjusted for cluster sampling and sampling weights for the present analysis. Children who were not alive during the interview or had a missing age variable were dropped from the sample. Regression analysis included only the youngest child in each family as the DHS collected dietary diversity data only on this population. Data were analysed for children between the ages of 0 and 23 months who had corresponding data for the outcome variables of interest as well as the control variables. If data were missing for any of these variables, the child was not included. Additionally, children who had implausible corresponding maternal heights (less than 100 cm) were not included in the analytic sample.
Infant and young child feeding indicators
The following IYCF indicators were calculated as specified by the WHO Indicators for Assessing Infant and Young Child Feeding Practices(8), based on available data from the 2007 Bangladesh DHS: early initiation of breast-feeding; exclusive breast-feeding under 6 months of age; continued breast-feeding at 1 year of age; introduction of solid, semi-solid or soft foods; minimum dietary diversity; minimum meal frequency; minimum acceptable diet; and consumption of Fe-rich foods. The optional IYCF indicators of continued breast-feeding at 2 years of age, age-appropriate breast-feeding and predominant breast-feeding at less than 6 months of age were also calculated. All of these variables were calculated per the WHO guidelines except for minimum dietary diversity (described below), which had to be adapted because of a limitation with the data available for calculating the dietary diversity index.
Dietary diversity index
A dietary diversity index (DDI) was created, rating the diversity of a child's diet from 0 to 6 by giving one point for each of the following food groups that were consumed the previous day (during the daytime or at night): (i) grains, roots and tubers; (ii) legumes and nuts; (iii) dairy products; (iv) flesh foods and eggs; (v) vitamin-A rich fruits and vegetables; and (vi) other fruits and vegetables.
Although the currently recommended indicators for assessing IYCF practices(8) recommend the use of seven categories (flesh foods and eggs are two separate categories), the 2007 Bangladesh DHS(42) combines meat, fish and eggs into one question. Therefore, six categories were used for the present study.
Minimum dietary diversity
Minimum dietary diversity (MDD) was defined in the present study as the proportion of children aged 6–23 months who received foods from four or more food groups (out of six). The recommended core indicator is four out of seven groups(8); however, as discussed previously, only six groups were available for the present study.
Anthropometric measures of nutritional status
Anthropometric measures of nutritional status, namely height-for-age Z-score (HAZ), weight-for-age Z-score (WAZ) and weight-for-height Z-score (WHZ), were calculated based on the WHO growth standards and were used to determine nutritional status among the children(43). Stunting, underweight and wasting were defined as being less than 2 sd below the median value for HAZ, WAZ and WHZ, respectively.
Sociodemographic influences
Variables included in the regression analyses were decided a priori based on potential influences on nutrition in the Bangladeshi context. These variables were: child sex, child age, the square of child age, maternal height, maternal BMI, maternal education, prenatal care visits, wealth index, current breast-feeding status, number of children, age of mother at first birth, residence (urban v. rural) and location (division in Bangladesh). In these analyses, child sex was defined as either male or female; child age was calculated using the number of days from the reported date of birth and then converted to months; maternal educational attainment (reported as none, primary, secondary or higher) was defined in two variables, (i) primary education v. no education and (ii) secondary education v. no education; and maternal height was given to the nearest 0·1 cm. The DHS calculates a wealth index using the DHS standard method based on ownership of assets, types of water access and sanitation facilities. Using principal components analysis to compute the wealth index, households in the data set are then classified into the poorest, poorer, middle, richer or richest wealth quintile based on the range of scores for Bangladesh(44). The index value given to each household was used in the present analysis.
Analysis
A multiple linear regression model was developed to determine the association between IYCF indicators and the continuous measures of anthropometric status (HAZ, WAZ and WHZ). Binomial logistic regression analysis was used to determine the association between the IYCF indicators and the binary outcomes of stunting, underweight and wasting. All regression models adjusted for the following potential confounding factors: child age in months, the square of child age, sex of the child, height of the mother, maternal BMI, education of the mother, prenatal care visits, urban v. rural residence, wealth index, current breast-feeding status, number of children, the age of the mother at first birth and regional dummy variables (division in Bangladesh) to control for unobservable factors at the regional level. When running the regression models for the IYCF indicators that were relevant only for currently breast-feeding children, current breast-feeding status was not used as a control variable. Regression models were run using the ‘svy’ command in STATA to ensure that standard errors were adjusted for the complex survey design. Adjusted mean HAZ was estimated using the ‘margins’ command in STATA, generating predicted HAZ values based on the corresponding regression model. The STATA statistical software package version 11 (2010; StataCorp LP, College Station, TX, USA) was used for all analyses.
Results
Sample characteristics
Table 1 and Fig. 1 describe the characteristics of the sample. Overall, child age was distributed as 6–11 months (29·91 %), 12–17 months (40·45 %) and 18–23 months (29·64 %), and gender was evenly split (50·60 % male and 49·40 % female).
Table 1 Characteristics of the sample (n 1508), 2007 Bangladesh Demographic and Health Survey

HAZ, height-for-age Z-score; WAZ, weight-for-age Z-score; WHZ, weight-for-height Z-score.
†Values are presented as means with their standard errors.
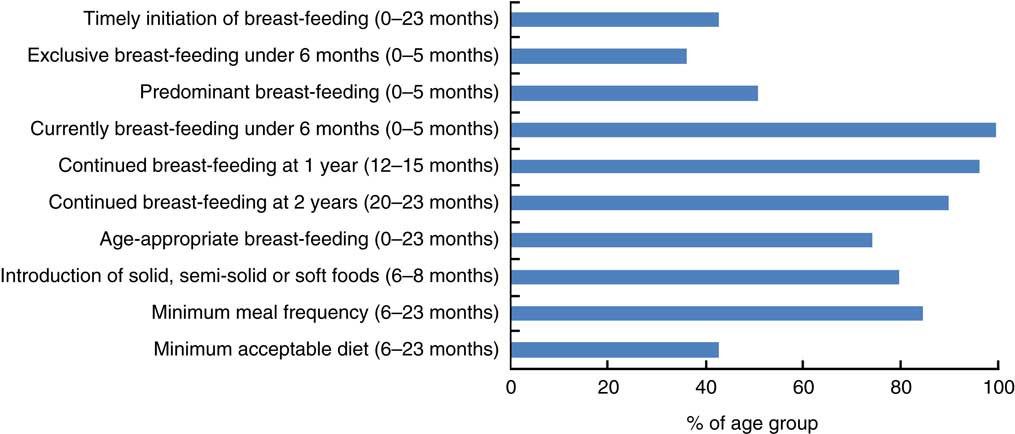
Fig. 1 (colour online) Infant and young child feeding practices among children aged 0–23·9 months, 2007 Bangladesh Demographic and Health Survey
In this sample 33·69 % of children were stunted, 21·42 % were wasted and 34·75 % were underweight. The mean HAZ, WAZ and WHZ were −1·45, −1·58 and −1·13, respectively (Table 1). The percentage of children in the sample meeting MDD was 45·16 % and the percentage of children who were exclusively breast-fed under 6 months was 36·05 % (Fig. 1).
Regression results
The results of the regression analyses that examined associations between the different IYCF indicators and anthropometric outcomes are summarized in Table 2. These models present the associations between adherence to the WHO-recommended IYCF practices and child anthropometry. The results in Table 2 demonstrate that exclusive breast-feeding under 6 months of age predicted WHZ higher by 0·29 (P = 0·049). For children with age-appropriate introduction of solid, semi-solid or soft foods, HAZ was higher by 0·63 (P = 0·005) and WAZ was higher by 0·30 (P = 0·038). Additionally, the log of the odds of stunting was lower by 1·34 (P = 0·005) for children with age-appropriate introduction of complementary foods. As DDI rose by 1 point, HAZ was higher by 0·08 (P = 0·006) and WAZ higher by 0·04 (P = 0·045). The log of the odds of stunting and underweight was lower by 0·12 (P = 0·020) and 0·12 (P = 0·013), respectively, as DDI increased by 1 point. For a child who was consuming at least four out of six food groups and thus achieving MDD, HAZ was higher by 0·20 (P = 0·024). The summary IYCF indicator of minimum acceptable diet predicted HAZ higher by 0·19 (P = 0·024) for those children who had a minimum acceptable diet. An illustrative example of a full regression model is provided in Table 3 which depicts the linear regression results for the association between DDI and HAZ.
Table 2 Summary of results from linear and logistic regression models on the association between IYCF practices and child anthropometric outcomes, 2007 Bangladesh Demographic and Health Survey

IYCF, infant and young child feeding; BF, breast-feeding; HAZ, height-for-age Z-score; WAZ, weight-for-age Z-score; WHZ, weight-for-height Z-score; EBF, exclusive breast-feeding.
(*)P < 0·10, *P < 0·05, **P < 0·01.
Table 3 Linear regression results for the association between DDI and HAZ in children aged 6–23 months, 2007 Bangladesh Demographic and Health Survey

DDI, dietary diversity index; HAZ, height for age Z-score.
(*)P < 0·10, *P < 0·05, **P < 0·01, ***P < 0·001.
The adjusted mean HAZ was significantly higher (P = 0·024) for children aged 6–23 months who achieved MDD compared with those who did not (Fig. 2). Adjusted mean WAZ was marginally higher (P = 0·11) among those who achieved MDD; mean WHZ (P = 0·97) was not significantly associated with MDD.

Fig. 2 (colour online) Adjusted mean height-for-age Z-score (HAZ), weight-for-age Z-score (WAZ) and weight-for-height Z-score (WHZ) by achievement of minimum dietary diversity (MDD; ![]() , did not achieve MDD;
, did not achieve MDD; ![]() , achieved MDD) among children aged 6–23 months, 2007 Bangladesh Demographic and Health Survey. Mean values were significantly different from those who did not achieve MDD: *P < 0·05
, achieved MDD) among children aged 6–23 months, 2007 Bangladesh Demographic and Health Survey. Mean values were significantly different from those who did not achieve MDD: *P < 0·05
Discussion
Using nationally representative data from Bangladesh, the analyses reported herein established a significant, positive linear association between a variety of IYCF practices and child HAZ. Specifically, exclusive breast-feeding among children under 6 months of age was significantly and positively associated with WHZ, but not with other anthropometric outcomes in this age group. We also found that age-appropriate introduction of solid, semi-solid and soft foods, a better DDI, achieving MDD and a minimum acceptable diet were associated with better HAZ. Additionally, a significant, positive linear association was found between age-appropriate introduction of solid, semi-solid and soft foods and better dietary diversity and WAZ.
The analyses indicated that exclusive breast-feeding was protective against wasting among children 0–6 months of age; this complements existing evidence that exclusive breast-feeding protects against infectious diseases, through both broad immune system benefits and the reduction in exposure to contaminated food(Reference Arifeen, Black and Antelman45, Reference Kramer and Kakuma46). Additionally, this finding is consistent with evidence that exclusive breast-feeding has a positive relationship with length and weight gain among infants in developing countries(47). Given the high levels of early wasting among infants in Bangladesh(42) and other South Asian countries(Reference Arnold, Parasuraman and Arokiasamy48), the finding that exclusive breast-feeding is protective against wasting is important from a public health and public policy perspective for the region. The lack of finding an association between exclusive breast-feeding and stunting or underweight was unsurprising in this context; both stunting and underweight are lower than wasting in the 0–6 month age group and increase later in infancy(Reference Victora, de Onis and Hallal2) – this pattern is seen in the Bangladesh DHS data as well. Thus, it is not anticipated that the data would reveal associations between exclusive breast-feeding and stunting or underweight in the 0–6 month age range. However, emerging research findings suggest that early wasting is predictive of later stunting(Reference Menon and Stoltzfus49) and thus the protective role for exclusive breast-feeding in relation to wasting takes on even greater public health significance, given the extremely high levels of stunting in Bangladesh and indeed South Asia.
It is well established that 6–23 months of age is a vulnerable period for child growth(Reference Victora, de Onis and Hallal2). It is also a vulnerable period for IYCF practices, as this is the age range within which a child must effectively be transitioned from breast milk only to a combination of breast milk and nutritionally adequate complementary foods or ‘family foods’. The analyses reported herein indicated that better IYCF practices during this vulnerable period were predictive of better growth outcomes among children. Our findings suggested adequate dietary diversity to be the indicator most strongly associated with better nutrition outcomes during this period. Other studies that have used a variety of indicators aimed at capturing food variety or dietary diversity have come to similar conclusions about the importance of the diversity of young children's diets(Reference Ruel and Menon10, Reference Sawadogo, Martin-Prevel and Savy12, Reference Onyango35, Reference Arimond and Ruel37, Reference Onyango, Koski and Tucker39–Reference Hatloy, Hallund and Diarra41). Building on these previous studies, and using nationally representative data, our analysis also showed a clear association between dietary diversity and linear growth above and beyond known socio-economic, sociodemographic and regional influences on child nutrition in the Bangladeshi context. The effect sizes for the associations seen between achieving MDD and child growth outcomes were substantial and biologically meaningful. Reviews of efficacy trials that aimed to improve complementary feeding among children aged 6–12 months found that improvements in growth rates due to these interventions ranged from 0·10 to 0·50 sd(Reference Caulfield, Huffman and Piwoz50). The associations seen in our analyses fell well within this range.
The lack of association between certain IYCF practices and child anthropometry does not imply that these practices are not important for child growth. For instance, the lack of association between early initiation of breast-feeding and child growth is not an argument against the importance of this practice. The evidence for the role of early and exclusive breast-feeding from a neonatal mortality perspective is strong and unequivocal(Reference Bhutta, Darmstadt and Hasan51). From the perspective of child growth, however, it is possible that this indicator acts mainly as a marker of better practices along a continuum of recommended optimal IYCF practices rather than as a direct marker of the nutrient quality of child diets. We note here that those variables that are indeed more direct markers of the nutrient quality of child diets, i.e. exclusive breast-feeding, diet diversity, minimum acceptable diet, appeared to demonstrate stronger associations with the child growth outcomes.
From a methodological perspective, the new IYCF indicators are designed to be used with population-level cross-sectional data based on the known biological significance of these practices either independently or in conjunction with other recommended IYCF practices on child growth. Acknowledging, however, that cross-sectional data do not allow robust causal inferences related to the links between these indicators and child growth, we highlight the need for longitudinal studies that document IYCF practices at the critical age points for each practice and together provide a stronger evidence base for the importance of these practices and their indicators in relation to child growth outcomes in different contexts.
The present study is not without limitations. First, as mentioned above, the cross-sectional nature of the data limits our analyses to exploring associations rather than determining causality. Longitudinal data would be better suited for this line of inquiry. However, we address the limitations of using cross-sectional data through inclusion of a variety of variables to control for confounding and regional unobservables. Second, the ability to generalize our results to other developing countries is not possible with this single country study although our results are likely applicable to similar regions in South Asia, including parts of India, given similarities in the growth patterns of infants in the region and the gaps in IYCF practices.
Conclusions
The results presented herein speak to three important points in relation to the Bangladeshi context: (i) exclusive breast-feeding under 6 months is protective of wasting; (ii) dietary diversity and the overall adequacy of child diets in the 6–23 months period is important for linear growth outcomes; and (iii) the new IYCF indicators exhibit important associations with child growth in Bangladesh and should continue to be monitored at a nationally representative scale.
Our findings have significant implications for public health practice, both in programme design and evaluation and for future research in Bangladesh and South Asia. We conclude that strategies to improve IYCF practices, and particularly to increase exclusive breast-feeding and improve the diversity of complementary foods fed to infants, should be a high priority in programmes that aim to address undernutrition among infants and young children in this region.
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. A.Z. conducted the analyses and write-up as part of her Masters degree in Public Health thesis at Emory University. K.W. and P.M. were supported by their institutions. There are no conflicts of interest. A.Z. conceptualized and implemented the data analysis, wrote first drafts of the manuscript and edited subsequent drafts. K.W. reviewed and edited the manuscript drafts, and supported the MPH thesis on same topic for A.Z. P.M. conceptualized and supported the data analysis, and reviewed and edited the manuscript versions.







