Behavioural theories suggest that social relationships influence health behaviours. For example, Social Cognitive Theory posits that behaviours are shaped by reciprocal interaction between personal and environmental factors, with social relationships being an important component of the environment( Reference Bandura 1 ). The Social Ecological Theory attempts to explain behaviours by providing context on the individual’s environment, including the social relationships (family, peers, schoolmates, etc.) that surround the individual( Reference Bronfenbrenner 2 ). Studies also provide evidence of links between social relationships and obesity. One such study provides preliminary evidence that obesity may spread within social networks in such a way that individuals with close relationships to an obese individual may be more likely to also become obese( Reference Christakis and Fowler 3 ). Some social relationship factors that influence dietary intake and physical activity have been identified. Examples of these factors include: social modelling (behaviours learned from observing others)( Reference Cruwys, Bevelander and Hermans 4 – Reference Horne, Hardman and Lowe 6 ); norms (behavioural rules generally accepted by a group)( Reference Higgs 7 – Reference Priebe and Spink 9 ); facilitation (enhancement or suppression of behaviours due to the presence of others)( Reference Rittenhouse, Salvy and Barkley 10 ); and impression management (attempts at controlling others’ opinions by modifying behaviour)( Reference Vartanian 11 , Reference Ommundsen, Gundersen and Mjaavatn 12 ). However, a comprehensive understanding of the mechanisms through which social relationships facilitate the spread of obesity remains unknown and under-researched( Reference Herman and Higgs 13 ), making it difficult for researchers to design and implement appropriate interventions targeting the social environment( Reference Salvy, de la Haye and Bowker 14 ).
Late childhood and early adolescence are important time periods to intervene as obese youths are more likely to become obese adults( Reference Serdula, Ivery and Coates 15 ). Social influences may play a particularly important role in the development of obesity during late childhood and early adolescence (ages 10–14 years) due to youths’ desire to conform to social norms( Reference Viner, Ozer and Denny 16 , Reference Stang and Story 17 ). Social dynamics also shift in late childhood and early adolescence. Youths begin spending more time with their peers( Reference Viner, Ozer and Denny 16 , Reference Rubin, Bukowski and Parker 18 ) and gain autonomy in their food-related decision making often due to increased access to money to independently purchase foods( Reference Dennisuk, Coutinho and Suratkar 19 ). Studies show that urban youths frequently purchase and consume high-energy and nutrient-poor foods, such as chips, candy, soda and fast food, when they are away from home( Reference Dennisuk, Coutinho and Suratkar 19 , Reference Borradaile, Sherman and Vander Veur 20 ). These purchasing behaviours, along with other factors, may contribute to high energy intakes and poor diet quality seen among urban African American youths( Reference Wang, Jahns and Tussing-Humphreys 21 ). High obesity rates and poor diet quality disproportionately impact low-income, African American youths( Reference Ogden, Carroll and Kit 22 – Reference Wang and Beydoun 24 ), and when combined with the known links between the social environment and weight status, underscore the importance of investigating the current social environment. This may aid in the development of strategies to prevent obesity in urban, minority youths.
Cross-sectional quantitative studies demonstrate that relationships exist between social relationships and weight-related behaviours( Reference Cruwys, Bevelander and Hermans 4 , Reference Vartanian 11 , Reference Herman 25 , Reference Lally, Bartle and Wardle 26 ); however, they are unable to provide in-depth information explaining the mechanisms through which these relationships seemingly spread obesity among social networks( Reference Salvy, de la Haye and Bowker 14 ). Additional qualitative research is needed to provide in-depth information and aid in the interpretation of these findings. The few qualitative studies that have examined social influences in youths are limited in scope, focusing narrowly on parents( Reference Savage, Fisher and Birch 27 ) or friends( Reference St George and Wilson 28 ), and fail to provide a holistic view of the diversity of social relationships of youths. In addition, only a small proportion of the qualitative studies focus on urban minority youths( Reference St George and Wilson 28 – Reference Dodson, Hsiao and Kasat-Shors 30 ). Mixed-methods studies have not yet been used to assess the interactions between urban, minority youths and their social relationships around eating and weight-related behaviours, and offer a unique opportunity to further explore this area.
The objectives of the present study were to: (i) provide in-depth information on the social roles that youths’ parents and friends play related to eating and physical activity behaviours; and (ii) explore the impact of other social relationships on youths’ eating and physical activity behaviours. Importantly, these data will help researchers and programme staff to identify potential ‘change agents’( Reference Gadhoke, Christiansen and Swartz 31 ) (i.e. influential individuals who could be engaged in obesity prevention interventions), as well as generate strategies to effectively incorporate social relationships in nutrition interventions.
Methods
Study design and setting
The present research uses a parallel convergent mixed-methods design and is a sub-study of B’More Healthy Communities for Kids (BHCK), a multilevel obesity prevention intervention conducted in low-income, racial and ethnic minority, food desert neighbourhoods in Baltimore, MD, USA( Reference Gittelsohn, Anderson Steeves and Mui 32 , Reference Franco, Diez Roux and Glass 33 ). All participants were recruited from communities participating in the BHCK parent study; however, different groups of participants were recruited for the quantitative and qualitative data collection components. In parallel convergent mixed-methods designs quantitative and qualitative data are collected and analysed in parallel, then merged for the interpretation and discussion of the results to enhance findings from both strategies (Fig. 1)( Reference Creswell and Plano Clark 34 , Reference Stenger, Ritter-Gooder and Perry 35 ).

Fig. 1 Convergent parallel mixed-methods design for examining social relationships and eating and physical activity (adapted from Creswell and Plano Clark( Reference Creswell and Plano Clark 34 ) and Stenger et al.( Reference Stenger, Ritter-Gooder and Perry 35 ))
Qualitative data collection and analysis
Instrument development
The instruments were developed by considering the goals of the research and by expanding upon previous work with this population( Reference Christiansen, Qureshi and Schaible 29 , Reference Gittelsohn, Dennisuk and Christiansen 36 ). Separate qualitative instruments were developed for in-depth interviews with youths and parents. Interview guides used open-ended questions to elicit themes related to the current eating- and physical activity-related behaviours of the youths, and the environmental, social and household influences on the youths’ health behaviours (Table 1). During the data collection process, the interview guides were refined through an iterative process. The research team met regularly to discuss the information being collected and to add questions to expand upon emerging themes.
Table 1 In-depth interview questions related to social influences on youths’ eating and physical activity behaviours for youth and parent interviews

Participant recruitment and selection
Eligibility criteria for the in-depth interviews required youths to be between the ages of 9 and 15 years, living in one of the predominantly African American, low-income neighbourhoods participating in the BHCK intervention, or regularly attending a recreation centre participating in the BHCK intervention. Participants were recruited at community locations (recreation centres, corner stores, etc.) with the support of community collaborators (recreation centre directors, store owners). Contact information was collected from interested participants and eligibility was confirmed with the parent/legal guardian. Purposive maximum variation sampling was used to obtain youths with a mix of genders, ages and neighbourhood locations (East v. West Baltimore). A total of thirty-eight youth interviews were conducted.
A sub-sample of youth participants’ parents were also recruited and interviewed in efforts to gain parental insight and enhance source triangulation. For nine of the ten youth–parent dyads, both the parent and youth were interviewed; one youth participant in this sub-sample declined to participate after her parent was interviewed. Parental consent and youth assent were collected prior to the data collection.
Qualitative data collection
Study team members trained in qualitative research methods (E.T.A.S., K.A.J., S.L.P.) conducted in-depth interviews with a total of forty-eight respondents. Refusal rates for in-depth interviews were not recorded; however, refusal rates for participating in interviews were very low among individuals referred to the programme by community collaborators and slightly higher when youths and adults were approached directly by study staff. Data collection continued until data saturation was reached and additional interviews did not yield novel themes( Reference Gibbs, Kealy and Willis 37 ).
Youth interviews (n 38) lasted 25–55 min and parent interviews (n 10) lasted 20–75 min. Youth and parent interviews were conducted separately. Twelve of the thirty-eight youth respondents were interviewed in pairs with other youths to facilitate the comfort and openness of younger respondents. Participants received a $US 20 gift card upon completion of the interview as an incentive to encourage participation.
All interviews were audio-recorded and transcribed verbatim immediately after the interview to preserve the emic terminology used by participants. In most cases the interviewer transcribed the interviews. Transcripts were uploaded to the Atlas.ti software version 7 (Atlas.ti Scientific Software, Berlin, Germany) for data management and analysis.
Qualitative data analysis
Guided by the principles of directed content analysis( Reference Hsieh and Shannon 38 ), interviewers (E.T.A.S., K.A.J., S.L.P.) reviewed the transcripts and generated an initial list of emerging themes. These themes, as well as several a priori codes of constructs from Social Cognitive Theory( Reference Bandura 1 ), Social Ecological Theory( Reference Bronfenbrenner 2 ) and specific research questions, were used to develop a codebook that was iteratively modified and used throughout the coding process. A total of thirty-two codes were developed and grouped into categories such as family relationships, peer relationships and physical activity. Two initial transcripts were double-coded by coders (E.T.A.S., K.A.J.), discrepancies in code usage between coders were resolved and the codebook was clarified. After the initial double-coding, transcripts were coded individually. Researchers met routinely to ensure codes were applied consistently and to discuss emerging themes. After all transcripts were coded, one researcher (E.T.A.S.) reviewed all transcripts to assure consistency and add new themes that emerged throughout the coding process.
Quantitative data collection and analysis
Instrument development
The quantitative measures collected demographic information and used a validated seven-item Change Agent questionnaire( Reference Gadhoke 39 ). This seven-item questionnaire was adapted for use in the BHCK study, with the purpose of assessing the social roles and interactions that support youths’ efforts to change their eating and physical activity behaviours( Reference Gadhoke 39 ). The original Change Agent questionnaire was designed for use in Native American/American Indian populations and was modified for the present study to include response options that reflect culturally appropriate relationships for low-income, urban African American youths. After the modifications were made, the adapted questionnaire was successfully pilot-tested in a sample of ten African American youths, which confirmed that the modified relationships were appropriate for this population( Reference Gittelsohn, Anderson Steeves and Mui 32 ). On the questionnaire, youths were asked to identify all of the people in their life who play selected supportive roles (questionnaire items listed in Table 2). Response categories included: parents, grandparents, siblings, other family members, friends, mentors, teachers, doctors and other. The response categories ‘mentor’ and ‘other’ experienced very low response rates (less than 5·7 % and 2·3 % for any question, respectively) and were removed from analyses.
Table 2 Types of support provided by different social relationships for modifying eating and physical activity behaviours among urban, minority youths (total n 297), Baltimore City, MD, USA
The values in this table represent the number and percentage of total youths (n 297) who reported receiving the support from the corresponding relationship. Respondents could choose multiple responses per prompt if multiple relationships were perceived to be providing that type of support. Different superscripts represent statistically significant differences in the proportion of youths who reported receiving support from the relationships at the α≤0·05 level. Having the same superscript indicates that the reported percentages are not significantly different. For example, in the first row (talks to you about making improvements in your food and physical activity habits?), parents (superscript a) were reported by a statistically significant higher percentage of youths than any other response. Grandparents, teachers and doctors/nurses (superscript b) were reported by a significantly different percentage of youths than parents (superscript a) and other family and friends (superscript c), but not a significantly different percentage from each other.
Participant recruitment and selection
Youths between the ages of 9 and 15 years living in neighbourhoods participating in the BHCK intervention were eligible for the quantitative surveys and were sampled using randomized sampling frames created from recruitment lists for each neighbourhood( Reference Gittelsohn, Anderson Steeves and Mui 32 ).
Quantitative data collection and analysis
Demographic data and the Change Agent questionnaire were collected, along with other data that are outside the scope of the current manuscript( Reference Gittelsohn, Anderson Steeves and Mui 32 ), during in-person interviews by trained and certified public health graduate students or study staff. Data were collected from a total of 297 youths who were provided a $US 30 gift card for completing the interview, which lasted approximately 60 min. Descriptive statistics, including the proportion of youths who reported receiving support for changing health behaviours (e.g. having someone in their life who would be their partner in making changes together), for each type of relationship (parent, grandparent, sibling, etc.), were calculated using the ‘proportion’ command in the statistical software package Stata version 13.1. Wald post-estimation tests, used to test the null hypothesis that the proportions are equal( Reference StataCorp 40 ), were then used to determine if statistically significant differences existed in the proportions of youths reporting that they receive support from each relationship for each of the seven Change Agent questions.
Mixed-methods data interpretation
In convergent parallel mixed-methods studies, the qualitative and quantitative strands of data are merged at the interpretation phase (Fig. 1). For the present study, the stated research objectives guided interpretation of the results, first by each strand of data collection, then by synthesizing a combined interpretation by layering the data collected from the different strands. The final stage of interpretation included assessing information provided by convergence and dissonance of both strands( Reference Creswell and Plano Clark 34 ). For example, when analysing the data on friend relationships (as part of objective 1), we first examined the quantitative results and the qualitative results separately. The quantitative results identified a unique pattern. The qualitative results, when layered with the quantitative results, were able to expand and add context to this pattern. Through exploring the differences in how the results were reported by respondents via the two methods allowed a deeper and more nuanced understanding of the influence of friend relationships on eating and physical activity behaviours in the sample.
The credibility of the findings presented in the current study was enhanced through the use of multiple forms of triangulation. Methodological triangulation was incorporated through the mixed-method study design which allowed for comparison and integration of the quantitative and qualitative data sets( Reference Lincoln and Guba 41 , Reference Shenton 42 ). Participant triangulation was incorporated by collecting and comparing the qualitative data from both youths and parents. Investigator triangulation was built into the study design and facilitated through weekly meetings between the data collectors and the larger study team. These meetings began during the research design phase and continued throughout the study, serving as the primary means of providing feedback and deciding on important emerging concepts during the design, data collection, analysis and interpretation phases.
Results
Sample characteristics
The quantitative survey was completed by 297 youths (53 % female, 91 % African American, mean age 12·3 (sd 1·5) years) from low-income households (68 % from households with income <$US 30000/year). In-depth interviews were conducted with thirty-eight youths (42 % female, 97 % African American, mean age 11·4 (sd 1·5) years) and ten parents (80 % female, 50 % single heads of house, 100 % African American). Qualitative participants were recruited from seven different Baltimore neighbourhoods, primarily in East or West Baltimore, and may have overlapping social relationships (i.e. similar friends) within those neighbourhoods.
Social relationships and interactions that influence youths’ eating and physical activity
A high proportion (74–89 %) of youths reported that they had someone in their life that provided support for changing eating and physical activity behaviours (Table 2). Parents, grandparents, friends, siblings, other family members, teachers and doctors/health-care providers were the main social relationships that influenced youths’ eating and physical activity. Parents and grandparents were identified most frequently and consistently in both the quantitative questionnaires and qualitative interviews as being sources of support and influence. Youths and parents elaborated on the influence of these social relationships by providing descriptive narratives of these interactions. Figure 2 integrates and synthesizes the results into a conceptual framework to aid in understanding the roles and interactions between youths and their social relationships.
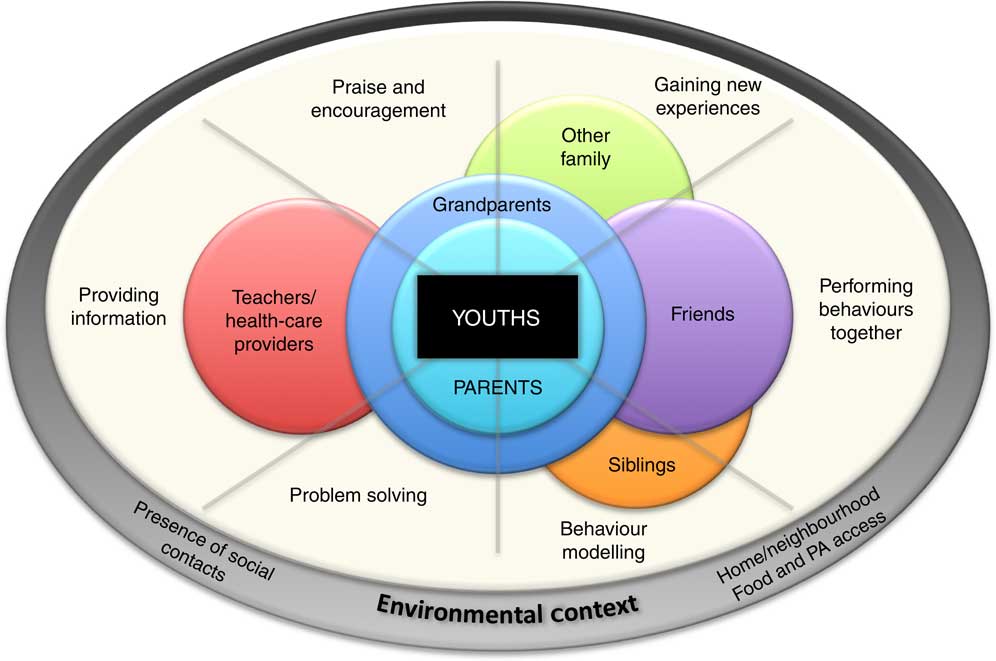
Fig. 2 (colour online) Conceptual framework depicting the influence of social relationships on youths’ eating and physical activity (PA) behaviours
Parents’ roles and interactions
Parents provided the most support for healthier behaviours. This is represented in Fig. 2 by the sphere representing ‘Parents’ being located centrally and in closest proximity to ‘Youths’. The location of this sphere encompassing all of the support strategies (‘Problem solving’, ‘Behaviour modelling’, etc.) indicates that parents were identified as playing all of these roles. In fact, parents were reported as being supportive of health behaviour change significantly more than any other relationship for the majority (six of seven) of the questions in the Change Agent questionnaire (P values<0·01). For example, 64 % of youths reported that their parents talk to them about making changes in their food and physical activity behaviours, compared with 26 % or less of youths reporting other relationships performing this role. Overall, for each question on the Change Agent questionnaire, parents were reported as performing that role by 30–64 % of youths. The majority of youths discussed parents as providing broad support for healthier eating and physical activity. A 12-year-old male said, ‘Man, my father he always talkin’; talkin’ to my mother and then talkin’ to us about like keeping your body healthy and stuff.’ A few youths described their parents’ unhealthy habits as motivation for them to take up healthy habits. For example, a 13-year-old female reported, ‘Sometimes I don’t want to eat a lot of junk food like my mother, so I just go ahead and eat healthy’, indicating both a lack of parental role modelling and parental apathy towards promoting healthier behaviours. Themes emerged about how parents provide support, which included: creating health-promoting rules; managing the home food environment; and serving as a role model for physical activity.
Creating health-promoting rules. Parents described promoting healthy eating and physical activity among youths by creating ‘rules’ such as reducing juice consumption by drinking water between glasses of juice, having a vegetable with every dinner meal and limiting screen time. An 11-year-old male reported, ‘I actually don’t watch TV or play video games during the week, my mom doesn’t allow me.’ The father of a 10-year-old female reported a household rule that his daughters had to finish their vegetables at meals, but also eluded to the fact that the rule may be loosely enforced, ‘Her mother tries to make her eat [greens], but then I’ll try to come to the rescue when she’s picking at ’em.’
Managing the home food environment. Parents also discussed how they modified their food purchasing behaviours to influence youths’ eating habits. The mother of an 11-year-old male described one method to reduce her son’s consumption of sugary snacks, ‘I just don’t buy it, and if I don’t buy it, how they gonna get it?’ However, parents’ desire for creating a healthy home food environment was tempered by the cost of grocery items and lack of information regarding the healthfulness of certain items. The mother of an 11-year-old-male described her household food purchasing behaviours by saying ‘I don’t buy candy too much … just for the holidays’ but then went on to say ‘I buy them Hawaiian Punch because it’s always two for $5 for the gallon. I’m not sure if it’s good or bad for ’em, but the price, you get a lot of juice for $5.’
Serving as a role model for physical activity. Youths occasionally described participating in physical activity with their parents; but young males also described their parents’ athletic legacy as influential on their desire to engage in physical activity. A 12-year-old male described his father’s sports career as an inspiration for his own dedication to athletics by saying, ‘He started playing when he was my age, at 12, it took him a year to get better at the sport, he’d wake up early in the morning and go to the basketball court and start practising, so he had a work ethic.’ This sentiment was echoed by other youths, demonstrating that parents’ past athletic experiences encouraged their pursuit of physical activity potentially more than parents’ current modelling of physical activity behaviours.
Grandparents’ roles and interactions
Grandparents – particularly grandmothers – were described as the second most supportive individual related to improving youths’ eating behaviours, which is why, in Fig. 2, ‘Grandparents’ are represented by a sphere encompassing both youths and parents, and spanning all of the identified supportive behaviours. After parents, grandparents provided significantly more support for health behaviour change compared with any other relationship on five out of the seven Change Agent questions (P values≤0·03). Thirteen to 26 % of youths reported grandparents performing the roles identified in the Change Agent questionnaire.
Intergenerational information exchange from grandparents. The main theme that both youths and parents reported was receiving advice from grandmothers about eating, particularly related to the type of foods that were appropriate for youths to consume, creating an expectation for nutrition and health information to be passed down through generations. A 10-year-old female explained this intergenerational involvement by saying ‘I think it is important to eat healthy because once I grow up, I’ll give advice to my kids and they’ll tell their kids and it goes on and on.’
Grandmothers were also identified by youths and parents as having a role in passing down cooking skills and teaching them to prepare both healthier (broccoli, greens) and less healthy foods (fried chicken and fish, red velvet cake). The mother of an 11-year-old-boy explained a family tradition, saying ‘My grandmother kept [my mother] and her sisters in the kitchen, and I was the only girl with my mom. My grandmother would cook every Sunday. I used to sit there; once I got older they used to have me startin’ with opening up cans and stuff like that.’
Friends’ roles and interactions
Friends had smaller and more specific roles related to eating and physical activity behaviours compared with parents and grandparents. Specifically, friends were identified as individuals who engaged in physical activity with youths, purchased and shared food with youths and potentially influenced the foods youths selected in social settings. In Fig. 2, the sphere representing ‘Friends’ is positioned in the ‘Performing behaviours together’ area to reflect these roles.
A significantly higher proportion of youths (42 %) reported that their friends would be their ‘partner’ in making positive food and physical activity changes together, compared with any other relationship (the next highest response was 30 % of youths reporting parents would play this role, P=0·01). Other than playing the role of ‘partner’, few youths (<11 %) reported that their friends performed other supportive roles identified on the Change Agent questionnaire. The qualitative themes provided more depth to this information by showing that youths’ friends often served as health-promoting partners for physical activity, but as negative influences on selecting healthier foods.
Performing physical activity with friends. Youths reported regularly participating on youth sports teams or in active clubs at school or recreation centres, and playing outside with their neighbourhood friends. An 11-year-old boy described spending time with neighbourhood friends by saying, ‘We’ll play dodge ball, we play hop scotch, we’ll play basketball, football. We just play a lot of games. It be fun.’ Parents also shared the perception that physical activity was something youths did with their friends. The mother of a 10-year-old girl explained her daughter’s sedentary behaviour by saying, ‘She’s not active because she don’t really have no friends.’
Acquiring and sharing food with friends. Youths also described getting and sharing less healthy items such as chips, cookies, candy, soda and sweetened fruit drinks with their friends. For example, a 14-year-old girl reported that she and her friends made a daily trip to the 7–11 store to get food before school. Parents also acknowledged that the eating and sharing of food between friends is commonplace, and that sharing food is part of the culture in some neighbourhoods. The mother of a 10-year-old boy said, ‘There’s things we do in our neighbourhood … sometimes the parents come out, like I do, and give the kids popsicles and stuff like that, or if [the kids’] friends have candy in the house they share with them.’
Friends’ influence on food choices. When youths described the influence of their peers on their eating choices, boys and younger girls (less than 12 years old) described feeling like their friends influenced their eating habits very little; for example, an 11-year-old male said, ‘Basically if you ask me, everybody eats the way they like to eat.’ Older girls described friends as having some influence on their choices; for example, a 12-year-old girl stated, ‘[if others are eating something] and they’re like popular, I want to eat it because I don’t want to be, like … the person who stands out.’ Parents also acknowledged the influence that youths’ friends have on food choices. The father of a 10-year-old girl shared ‘They see their friends eating like chicken fingers or something like that and it makes them wanna eat it.’ This influence may be limited to occasions when youths are in the presence of their peers, as stated by a 15-year-old boy, ‘If I’m with my friends or something, I eat out, but if I’m home I eat in the house.’
Siblings’ roles and interactions
Youths identified siblings as primarily being ‘partners’ in food- and physical activity-related behaviours. A higher percentage of youths (17 %) reported that siblings were willing to be a ‘partner’ in eating and physical activity behaviour changes than to provide other forms of support as assessed by the Change Agent questionnaire. However, a significantly higher proportion of youths reported other relationships such as friends and parents also played this role (P values<0·01). Parents described behavioural mimicry occurring among siblings. In Fig. 2, this is represented by the ‘Sibling’ sphere located in both the ‘Behaviour modelling’ and ‘Performing behaviours together’ sections.
Siblings’ home food preparation. One way youths described ‘partnering’ with their siblings was in food preparation, particularly preparing snacks together when their main caregiver was not available. A 14-year-old girl reported, ‘Usually it just be me and my sister ’cause we’ll cook, we’ll bake like hot wings in the oven.’
Behavioural mimicry among siblings. Parents identified that younger siblings mimic older siblings’ choices. The mother of an 11-year-old boy reported that, ‘[the participant’s son’s] little brother will follow behind him, so whatever he eat, his little brother wanna eat.’
Other family members’ roles and interactions
Other family members, particularly aunts and cousins, provided some support for health behaviour change. Aunts encouraged youths to try novel foods, while cousins served as companions in both active and sedentary activities. However, their roles were lesser than for other familial relationships, with a small percentage of youths (8–13 %) reporting that other family members played a supportive role in health behaviour change. These percentages were significantly lower than for primary familial relationships such as parents (P values<0·01) for all questions and grandparents for most questions (six of seven questions; P values<0·01).
Providing novel food experiences. Both parents and youths described how youths eating with other family members on a regular basis could create opportunities to experience new foods. The mother of a 10-year-old girl said, ‘My daughter came home [from a relative’s house] eating hot sauce. She came home eating pig’s feet. I don’t eat pig’s feet. Some other stuff … chitterlings. I don’t eat chitterlings; I know she done picked that up from somewhere else.’ An 11-year-old boy shared his negative experience of trying new foods, saying, ‘I was over at my aunt’s house and, you know, sometimes she has food I’ve never ate before. So she said: “Try this, you might like it. It’s very good” … so I taste it. I tell her it’s good. And as soon as she walk away I just had to spit it out.’ Figure 2 represents these relationships by depicting the ‘Other family’ sphere in the ‘Gaining new experiences’ section.
Cousins as companions. Youths often described visiting cousins on the weekend or during the summer and participating in sedentary (television, video games) and physically active behaviours together. An 11-year-old male described, ‘Me and my cousin play Wii Fit, Wii Sports. We play Mario. Mario, yeah, is fun. Them days is fun.’
Professionals’ roles and interactions
Professionals (i.e. teachers and health-care providers) were identified by youths as primarily providing information about healthy eating and physical activity, but doing little else in terms of influencing youths’ eating and physical activity behaviours. For example, 20 % and 21 % of youths reported teachers and doctors talking to them about making improvements, but only 5 % and 4 % of youths reported that their teachers and doctors, respectively, would be partners in making changes. In Fig. 2, the ‘Teachers/health-care providers’ sphere is located in the ‘Providing information’ section to reflect these relationships.
Health information from health-care providers. Youths and parents both described situations where doctors and health-care providers provided nutrition or physical activity information for the youth, mostly related to weight status. A 10-year-old girl stated that the doctor, ‘… said I was a little overweight for my age, and he gave me forms about what I should eat and what I shouldn’t.’ In addition to direct conversations with their doctors, youths often reported second-hand health information from doctors being passed down through other family members. A 10-year-old male said he knew drinking water was important because ‘My grandmother used to have kidney problems and her doctor told her “drink more water, it’s gonna cleanse your system”. My grandmother told my mother and my mother told me.’
Health information from school programmes. Youth expressed that health information and physical activity opportunities were shared through school-related programming (such as school-based sports teams, field trips to farms, school gardens, etc.), more so than directly from teachers.
Discussion
The present study used a convergent parallel mixed-methods design to explore the interactions and roles that different social relationships had on eating- and physical activity-related health behaviours in low-income, predominantly African American youth in Baltimore City. There is a growing interest in intervening in the social environment; however, it is recognized that modifying the social environment by outside parties may be difficult( Reference Salvy, de la Haye and Bowker 14 ). These results may provide important insight that would aid in intervention design and should be considered when designing future programmes for this population.
In the present study youths reported that parents, grandparents, friends, siblings, other family members, teachers and health-care providers interact with them related to eating and physical activity behaviours through semi-distinct roles, which is consistent with Koehly and Loscalzo’s conceptualization of youths’ social network( Reference Koehly and Loscalzo 43 ). Similar to previous studies( Reference Draxten, Fulkerson and Friend 5 , Reference Pedersen, Grønhøj and Thøgersen 8 , Reference St George and Wilson 28 – Reference Dodson, Hsiao and Kasat-Shors 30 , Reference Biggs, Lebow and Smith 44 , Reference Oliveria, Ellison and Moore 45 ), the present study identified parents as playing the most significant role in promoting healthy eating and physical activity habits among youths. Grandmothers were also identified as playing an important, multidimensional role. Friends were perceived as individuals that youths partner with to actually engage in health-related behaviours (i.e. participate in active leisure-time activities, purchase and share food), which is consistent with the literature( Reference St George and Wilson 28 , Reference Christiansen, Qureshi and Schaible 29 , Reference Biggs, Lebow and Smith 44 , Reference Bruening, Eisenberg and MacLehose 46 , Reference Barkley, Salvy and Sanders 47 ). Our results indicated that while friends promoted healthy physical activity behaviours by being willing to be active with youths, the food-related behaviours that friends influenced tended to involve purchasing, sharing and consumption of less healthy foods choices, indicating that friends serve as ‘partners’ to support engaging in physical activity and serve as ‘partners in crime’ in relation to eating-related behaviours. This potentially indicates that the 42 % of youths who reported their friends would serve as partners in making health behaviour changes were more focused on physical activity behaviours, rather than eating behaviours.
To our knowledge, the present study is one of the first to explore the roles of social relationships beyond immediate family and friends on youths’ eating and physical activity behaviours. Overall friends, other family members, teachers and health-care providers had specific, but limited roles and interactions around youths’ eating and physical activity behaviours.
Given the known relationships between social relationships and obesity( Reference Koehly and Loscalzo 43 ), researchers should consider these factors when designing interventions to prevent and treat obesity in urban, racial and ethnic minority youths. Specifically, future research is needed to test the effectiveness of intervention strategies that enhance or expand the supportive roles played by social relationships. Examples of intervention strategies that could enhance current roles could include things such as:
-
∙ Working with parents to create a healthy home food environment or on adopting appropriate parenting styles (including rule making and enforcement) that promote healthy behaviours.
-
∙ Working with grandparents to prepare healthier versions of traditional family recipes that can be passed down through the generations.
-
∙ Embracing the opportunity for novel food consumption that aunts provide by encouraging aunts to introduce novel, healthful choices.
-
∙ Involving friends and potentially siblings and/or cousins in interventions that encourage paired physical activity behaviours and design strategies that promote sharing of healthier food options rather than less healthy options with friends.
-
∙ Working with teachers and health-care providers to expand their roles beyond simply providing weight-related health information to other components of support. For example, teachers could lead short in-class bouts of physical activity.
Obesity is a multifaceted problem and researchers have begun to address it through systems-oriented interventions with multicomponent intervention strategies( Reference Gortmaker, Swinburn and Levy 48 ). Large intervention trials such as Shape Up Somerville( Reference Economos, Hyatt and Must 49 ) and BHCK( Reference Gittelsohn, Anderson Steeves and Mui 32 ) use multicomponent interventions to address the physical environment; however, the present results and others suggest that there may be value in investigating multicomponent social environment intervention strategies as well.
Study limitations must be acknowledged. In the present study we were not able to assess whom the youths identified as their primary caregivers (parents v. others), which may have influenced youths’ perceptions of the roles that different relationships play. The purposive sampling strategy used in the qualitative strand has the potential to create sampling bias, as parents and youths who agreed to participate may be more interested in nutrition, physical activity and overall health than those who declined interviews. In addition, the measures collected in the study were self-reported; while data collectors encouraged participants to answer as truthfully as possible, some participants may have skewed responses due to social desirability bias. Despite these limitations, the findings provide novel and valuable information related to the roles and interactions that influence the eating and physical activity behaviours of low-income, urban, predominantly African American youths.
Conclusion
These data suggest that there are multiple social relationships that influence youths’ eating and physical activity behaviours. When designing interventions aimed to create impact in the social environment, researchers and practitioners should consider the unique roles and interactions that different relationships have in supporting weight-related health behaviour change for youths. Future research should consider testing the strategies suggested herein that address multiple levels of the social environment, as well as other factors such as the built environment, to fully conceptualize the systems in which obesity-related behaviours operate.
Acknowledgements
Financial support: The project described was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD; grant number U54HD070725). The project is co-funded by the NICHD and the Office of Behavioral and Social Sciences Research (OBSSR). The funders had no role in the design, writing or analysis of this article. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NICHD or OBSSR. Conflict of interest: None. Authorship: E.T.A.S. was responsible for the study design, data collection oversight, analysis and manuscript preparation. K.A.J. and S.L.P. aided in data collection and analysis of the qualitative results. J.J.-S. aided in the analysis of the quantitative data collection. K.P. and S.L.J. aided in the interpretation of qualitative data. L.H. is the project coordinator and contributed to the quantitative data collection. J.G. is the Principal Investigator for the parent study and provided significant oversight throughout data collection, analysis and manuscript preparation. All authors provided significant feedback throughout the manuscript writing process. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board. Written informed consent/assent was obtained from all subjects/patients. In addition, parental consent was obtained for all youth participants.







