Patient experience is a vital source of evidence that can drive the provision of high-quality health services.1, 2 Mental health in-patients report a range of experiences including fear of assault, concerns regarding coercion, limited recovery-focused support and lack of therapeutic activities.3–8 A triennial review of mental health services in England by the Care Quality Commission (2017)9 highlighted several serious concerns about in-patient care, including wards located in older buildings not designed to meet the needs of acute patients, unsafe staffing levels and overly restrictive care in wards far from patients' homes and families.
The National Health Service (NHS) is under pressure to deliver timely, effective and affordable care with increasingly constrained resources. The National Institute for Health and Care Excellence, the NHS National Quality Board and others have restated core principles of patient-centred care including dignity, compassion, choice and autonomy,3–5, 5–8 and called for a strengthening of the patient voice. Healthcare providers are now required to collect data to assess patients' experiences of care.9–Reference Bramesfeld, Klippel, Seidel, Schwartz and Dierks12 However, the impact of this data collection on services is unclearReference Coulter, Locock, Ziebland and Calabrese13 because of: the diverse and poor-quality feedback methods,14 a lack of consensus about which experiences are most salient (and hence should be asked about), and limited evidence about how patient experience data can guide service improvements.Reference Coulter, Locock, Ziebland and Calabrese13, Reference Boiko, Campbell, Elmore, Davey, Roland and Burt15 Such challenges highlight the need for robust evidence to inform best practice, with clarity about the experiences of most importance to patients. In response to this need, this systematic review aimed to identify the most salient experiences of people using in-patient mental healthcare to inform the provision of high-quality services.
Method
The review was divided into a scoping review to ascertain the nature and size of the evidence base, and the main systematic review.
Protocol and registration
The EURIPIDES (Evaluating the Use of Patient Experience Data to Improve the Quality of Inpatient Mental Health Care) systematic review was registered in 2016 on PROSPERO: CRD42016033556.
Scoping review
Before the systematic review, a scoping review was conducted to ascertain the extent, range and nature of studies to map emerging key themes without describing the findings in full or performing a quality checkReference Arksey and O'Malley16 and to inform the main review. Six key authors known to be experts in mental health patient experience were contacted for new or unpublished reports and studies.
Patient and Public Involvement Reference Group
The Patient and Public Involvement Reference Group (PPIRG) included 10 service users, recruited by the Mental Health Foundation, with experience of in-patient care or caring for someone who had been an in-patient. They were invited to two meetings: first, to obtain their views on the themes identified in the scoping review, with the potential to add further concepts they felt had not been identified; and second, to obtain their opinions on themes identified in the main systematic review and to contribute to the interpretation of our findings. A full description of the patient involvement in the study is reported using the GRIPP2 Short Form Checklist in Table 1.
Table 1 Reporting Patient and Public Involvement in the EURIPIDES study using GRIPP2

a. Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, Altman DG, Moher D, Barber R, Denegri S, Entwistle A, Littlejohns P, Morris C, Suleman R, Thomas V, Tysall C. GRIPP2 reporting checklist: tools to improve reporting of patient and public involvement in research. BMJ 2017; 358: j3453.
Identification of studies for the systematic review
Guided by the themes that emerged from the scoping review, search terms and a search strategy were developed and applied to the databases MEDLINE, CINAHL and PsycINFO. An example of search terms and results is reported in Fig. 1. Reference lists of included papers were scanned. The search deviated from the protocol in that only three of five databases were searched due to the large numbers of abstracts retrieved (Web of Science and Embase were not used).

Fig. 1 Example of search strategy from MEDLINE.
Inclusion and exclusion criteria
All study designs were considered if papers included experiences of current or former in-patients of mental health institutions. No restrictions were applied based on country. Articles were included if they reported primary research, were peer reviewed and published in English between January 2000 and January 2016. Papers were excluded if they were not primary studies, based on pre-2000 data, included children and adolescents (aged under 18 years) or were not in the English language. Where study participants included both in- and out-patients, only data regarding in-patient experiences were extracted. Reviews (Table A.1) were noted and reference lists scanned, but excluded from the review to avoid bias.
Study selection
Titles and abstracts were screened (C.M., G.C.), 20% of which were independently cross-checked for agreement before obtaining full-text articles (S.S. and C.M.). Full texts were obtained where the abstract was unclear. Any disagreements could be resolved by consensus (C.M., G.C. and S.S.) but no disagreements occurred.
Data extraction
The data extracted, using Microsoft Excel (version 2013), included citation details, sample recruitment and research methods, findings related to key concepts and any other emerging concepts (C.M.).
Quality and risk of bias in individual studies
The quality of the studies were evaluated by the Critical Appraisal Skills Programme (CASP) Qualitative Checklist,17 undertaken by C.M. Because of the heterogeneity of the included studies, many of which were descriptive in their approach, this checklist provided an appropriate basis for comparison between studies. The only question change in the CASP checklist was from ‘Is the qualitative methodology appropriate for this study?’ to ‘Is the methodology appropriate for this study?’
Data analysis
The scoping review informed the development of a thematic framework, which guided but did not restrict the review. A narrative synthesis of the themes was undertaken.Reference Sandelowski, Voils and Barroso18 As the researcher read each study, an initial preliminary synthesis of the study was undertaken and emerging sub-themes were identified. The researcher was then able to compare themes and sub-themes within and across studies and further develop them into the main themes. Themes were summarised in a descriptive form, allowing for the findings of all review studies, regardless of study design, to be aggregated and summarised. We used the concept of data saturation to help us decide when to complete data extraction. Saturation of data is judged to have happened at a point where no new themes are being identified in the studies when compared with what has already been extracted.Reference Staniszewska, Boardman, Gunn, Roberts, Clay, Seers, Brett, Avital, Bullock and O'Flynn7 It is a useful approach for large reviews where the addition of further papers is unlikely to change key findings.
Results
PPIRG
Key themes identified in the scoping review were discussed in detail by group members who critiqued their content and identified additional areas such as boredom. The PPIRG provided content and face validity for the identified themes and provided real-life examples of the themes from their own experiences. The PPIRG also provided an opportunity to check if the themes identified from international studies resonated in a UK context.
The systematic review
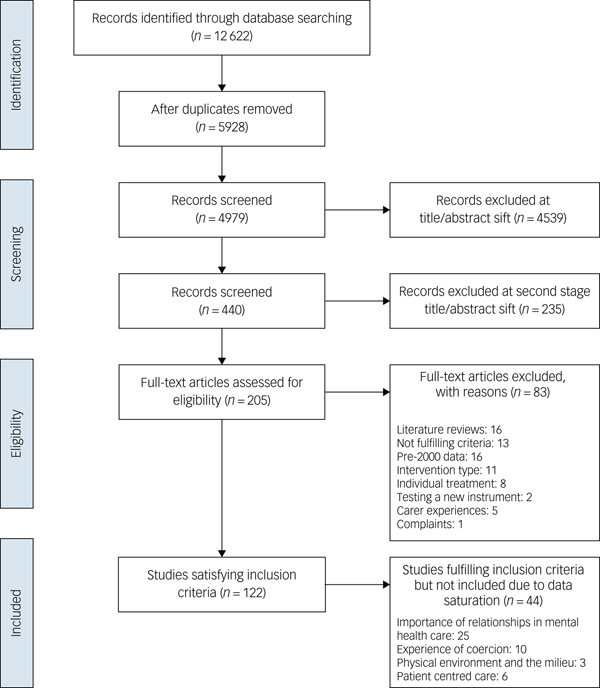
A total of 4979 abstracts were screened and 116 papers fulfilled the inclusion criteria (Fig. 2). Two consecutive sifts were conducted due to an error in the first search of the PsycINFO database omitting 2980 hits which was identified after the first sift was completed. The first sift of 1999 hits resulted in 72 relevant papers for the review; 11 papers were from same studies.Reference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19–Reference Wyder, Bland, Herriot and Crompton29 Following this, the second sift of 2980 abstracts resulted in an additional 44 studies fitting the criteria (total n = 116). Drawing on the principles of data saturation,Reference Dixon-Woods, Agarwal, Jones, Young and Sutton30 additional studies that repeated themes already identified were excluded from the main review. In total, eight studies added new themes and were included at this stage.

Fig. 2 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009 flow diagram.
A total of 16 systematic reviews (Table A.1) which investigated in-patient experience were identified. In total, 72 studies were included in the review, a third of which were from the UKReference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24–Reference Russo and Rose47 (n = 24)Reference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19–Reference Bennewith, Amos, Lewis, Katsakou, Wykes and Morriss21, Reference Whittington, Bowers, Nolan, Simpson and Neil25, Reference Stewart, Burrow, Duckworth, Dhillon, Fife and Kelly27, Reference Alexander31–Reference Kennedy and Fortune49 (Supplementary Table 1 available at https://doi.org/10.1192/bjp.2019.22). Although studies using qualitative methods were most common (Table A.1), studies using patient experience questionnaires and patient record data were also included. The CASP checklist identified many of the papers as being of medium to poor quality.
Timing of data collection in included studies
Little information was provided about the timing of data collection in over a third of papers (37%), other than describing participants as in-patients at the time.Reference Whittington, Bowers, Nolan, Simpson and Neil25–Reference Stewart, Burrow, Duckworth, Dhillon, Fife and Kelly27, Reference Alexander31, Reference Baker, Lovell, Easton and Harris32, Reference Chorlton, Smith and Jones35, Reference Cutting and Henderson36, Reference Labib and Brownell43, Reference Milner, Jankovic, Hoosen and Marrie44, Reference Stenhouse48–Reference Johansson and Eklund63 Data were mostly collected just before,Reference Wyder, Bland, Blythe, Matarasso and Crompton28, Reference Wyder, Bland, Herriot and Crompton29, Reference Nolan, Bradley and Brimblecombe45, Reference Brunero, Lamont and Fairbrother64–Reference Strauss, Zervakis, Stechuchak, Olsen, Swanson and Swartz73 immediately after dischargeReference Katsakou, Rose, Amos, Bowers, McCabe and Oliver20, Reference Nolan, Bradley and Brimblecombe45, Reference Roe and Ronen59, Reference Anders, Olson and Bader74, Reference Steinert, Birk, Flammer and Bergk75 or from former in-patients.Reference Kauppi, Hätönen, Adams and Välimäki22, Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Bowl34, Reference Duggins and Shaw37–Reference Gilburt, Rose and Slade39, Reference Hughes, Hayward and Finlay41, Reference Jones and Crossley42, Reference Ridley and Hunter46, Reference Russo and Rose47, Reference Johansson and Eklund63, Reference Bramesfeld, Wedegartner, Elgeti and Bisson76–Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 This suggests that patients were recovering when experiences were elicited. In three studies, data collection coincided with a ward event (e.g. refurbishment).Reference Kulkarni, Gavrilidis, Lee, Van Rheenen, Grigg and Hayes81–Reference Shattell, Melanie Andes and Thomas83 A number of studies (n = 12, 17%) collected data shortly after an event such as admission,Reference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19, Reference Bennewith, Amos, Lewis, Katsakou, Wykes and Morriss21, Reference Giacco, Fiorillo, Del Vecchio, Kallert, Onchev and Raboch84–Reference Thapinta, Anders, Wiwatkunupakan, Kitsumban and Vadtanapong86 seclusion, sedation or restraint.Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Bonner, Lowe, Rawcliffe and Wellman33, Reference Chien, Chan, Lam and Kam87–Reference O'Brien and Cole92
Identification of key themes
Patient experiences were categorised into four overarching themes or dimensions of experience: the importance of high-quality relationships; averting negative experiences of coercion; a healthy, safe and enabling physical environment and ward milieu; and authentic experiences of patient-centred care. These key themes accompanied by sub-themes are described in detail below.
The importance of high-quality relationships
The importance of high-quality relationships was the most consistently reported theme.
Important factors in developing such relationships with staff included being treated with respect, feelings of stability, recognising empathy and high-quality communicationReference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19, Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Stewart, Burrow, Duckworth, Dhillon, Fife and Kelly27, Reference Wyder, Bland, Blythe, Matarasso and Crompton28, Reference Chorlton, Smith and Jones35, Reference Cutting and Henderson36, Reference Fenton, Larkin, Boden, Thompson, Hickman and Newton38, Reference Gilburt, Rose and Slade39, Reference Borge and Fagermoen51, Reference Gunasekara, Pentland, Rodgers and Patterson55, Reference Sibitz, Scheutz, Lakeman, Schrank, Schaffer and Amering60, Reference Thibeault, Trudeau, d'Entremont and Brown61, Reference Johansson and Eklund63, Reference Looi, Engström and Sävenstedt78, Reference Chien, Chan, Lam and Kam87, Reference Iversen, Sallaup, Vaaler, Helvik, Morken and Linaker90 with staff who patients felt were trustworthy, reliableReference Chorlton, Smith and Jones35, Reference Johansson and Eklund63, Reference McGuinness, Dowling and Trimble69 or helpful.Reference Stewart, Burrow, Duckworth, Dhillon, Fife and Kelly27, Reference Borge and Fagermoen51, Reference Donald, Duff, Lee, Kroschel and Kulkarni54, Reference Thomas, Shattell and Martin62 Good staff–patient relationships facilitated the in-patient care pathway in mental health institutionsReference Wyder, Bland, Blythe, Matarasso and Crompton28, Reference Chorlton, Smith and Jones35, Reference Gilburt, Rose and Slade39, Reference Borge and Fagermoen51, Reference Greenwood, Hussain, Burns and Raphael68 and reduced the use of coercive measures.Reference Chorlton, Smith and Jones35, Reference Nolan, Bradley and Brimblecombe45, Reference Looi, Engström and Sävenstedt78 Ward rounds were an important setting for staff–patient interaction and patients reported these as helpful and informative.Reference Milner, Jankovic, Hoosen and Marrie44
Potential barriers to therapeutic relationships included: gender-specific problems – male nursing staff were not welcome if the patient had a history of abuse by male perpetratorsReference Cutting and Henderson36, Reference Looi, Engström and Sävenstedt78 or where gender-specific cultural barriers existed (e.g. a Muslim woman supervised by a male nurse);Reference Greenwood, Hussain, Burns and Raphael68 lack of meaningful communication – where communication was compromised due to differences in culture, language, religion,Reference Bowl34, Reference Gilburt, Rose and Slade39, Reference Ntsaba and Havenga57, Reference Greenwood, Hussain, Burns and Raphael68 through use of coercive measuresReference Bonner, Lowe, Rawcliffe and Wellman33, Reference Sibitz, Scheutz, Lakeman, Schrank, Schaffer and Amering60 or where technical language used by staff was not easily understood;Reference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19 absence of regular ward staff – patients were upset by the absence of regular ward staff due to office duties, shift working, reliance on temporary staffReference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Stewart, Burrow, Duckworth, Dhillon, Fife and Kelly27, Reference Wyder, Bland, Blythe, Matarasso and Crompton28, Reference Chorlton, Smith and Jones35–Reference Duggins and Shaw37, Reference Gilburt, Rose and Slade39, Reference Nolan, Bradley and Brimblecombe45, Reference Ridley and Hunter46, Reference Borge and Fagermoen51, Reference Donald, Duff, Lee, Kroschel and Kulkarni54, Reference Gunasekara, Pentland, Rodgers and Patterson55, Reference Johansson and Eklund63, Reference McGuinness, Dowling and Trimble69 and having extended waits to speak to staffReference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Cutting and Henderson36, Reference Ridley and Hunter46, Reference Donald, Duff, Lee, Kroschel and Kulkarni54, Reference Lilja and Hellzen77, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80, Reference Lindgren, Aminoff and Graneheim82 particularly at ward rounds;Reference Labib and Brownell43 poor staff attitude – where patients complained that staff ignored them,Reference Ntsaba and Havenga57, Reference Chien, Chan, Lam and Kam87, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88, Reference Meehan, Vermeer and Windsor91 displayed indifferenceReference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24 or insufficient understanding of patients;Reference Looi, Engström and Sävenstedt78 inconsistent staff behaviour – reports of staff interpreting ward rules inconsistently, causing confusion;Reference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19, Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Stewart, Burrow, Duckworth, Dhillon, Fife and Kelly27, Reference Alexander31, Reference Bonner, Lowe, Rawcliffe and Wellman33, Reference Cutting and Henderson36, Reference Ridley and Hunter46, Reference Kennedy and Fortune49, Reference Lindgren, Aminoff and Graneheim82, Reference Meehan, Vermeer and Windsor91 staff abuse – some patients reported abuse by staff, including provocation, bullying, shouting or belittling of patients.Reference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19, Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Stewart, Burrow, Duckworth, Dhillon, Fife and Kelly27, Reference Wyder, Bland, Blythe, Matarasso and Crompton28, Reference Bonner, Lowe, Rawcliffe and Wellman33, Reference Gilburt, Rose and Slade39, Reference Lucas and Stevenson56, Reference Thomas, Shattell and Martin62, Reference Looi, Engström and Sävenstedt78, Reference Mayers, Keet, Winkler and Flisher79, Reference Shattell, Melanie Andes and Thomas83, Reference Chien, Chan, Lam and Kam87, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88
Relationships with other patients and with relatives
Patients relied on other patients for information about ward activities and rules, to share experiences and when debriefing after group sessions.Reference Kauppi, Hätönen, Adams and Välimäki22, Reference Nolan, Bradley and Brimblecombe45, Reference Lilja and Hellzen77, Reference Lindgren, Aminoff and Graneheim82, Reference Shattell, Melanie Andes and Thomas83 However, arguments and violence between patientsReference Cutting and Henderson36, Reference Gilburt, Rose and Slade39, Reference Stenhouse48 generated fear and isolation for some, causing them to retreat to their rooms for safety or to abscond.Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Duggins and Shaw37, Reference Gilburt, Rose and Slade39, Reference Kennedy and Fortune49, Reference Cleary, Horsfall and Hunt65, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80
Isolation from family caused distress. Patients reported that having a friend or family member with them would have helped with orientationReference Mayers, Keet, Winkler and Flisher79 and they could have helped staff with assessments and treatment plans.Reference Kauppi, Hätönen, Adams and Välimäki22, Reference Fenton, Larkin, Boden, Thompson, Hickman and Newton38, Reference Cleary, Hunt, Escott and Walter53 However, family members felt left out of decision-making about care.Reference O'Brien and Cole92
Averting negative experiences of coercion
The second main theme was concerned with experiences of coercion. All patients expected to be treated as ‘normal human beings’Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Wyder, Bland, Herriot and Crompton29, Reference Lilja and Hellzen77 and addressed professionally, including during restraint.Reference Chien, Chan, Lam and Kam87 Patients wanted the reasons for coercive measures to be communicated so they could understand them as this helped some patients trust staff and feel safe.Reference Ridley and Hunter46, Reference Georgieva, Mulder and Wierdsma67, Reference Steinert, Birk, Flammer and Bergk75, Reference Mayers, Keet, Winkler and Flisher79, Reference Chien, Chan, Lam and Kam87 Patients valued persuasion over threats of forceReference Sibitz, Scheutz, Lakeman, Schrank, Schaffer and Amering60 and coercion,Reference Looi, Engström and Sävenstedt78 which could bring back memories of past history of violence and neglect.Reference Bonner, Lowe, Rawcliffe and Wellman33, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88, Reference Holmes, Kennedy and Perron89
Where coercive measures were discussed in the studies, these included experiences of sedation, seclusion and restraint. It has been reported that Black and minority ethnic patients are more likely to experience coercion than White patients.
Ethnicity
Two studies examined the commonly held perception that Black and minority ethnic patients experienced more coercion on admission than other patients.Reference Bennewith, Amos, Lewis, Katsakou, Wykes and Morriss21, Reference Anders, Olson and Bader74 The findings were not conclusive: although hospitals in the UK with higher proportions of Black and minority ethnic patients employed more coercive practices, this was independent of individual patient ethnicity.Reference Bennewith, Amos, Lewis, Katsakou, Wykes and Morriss21, Reference Anders, Olson and Bader74
Sedation
Some patients recognised that medication was important for the in-patient care pathway.Reference Katsakou, Rose, Amos, Bowers, McCabe and Oliver20, Reference Gilburt, Rose and Slade39, Reference Hughes, Hayward and Finlay41 Some trusted staff to decide on appropriate sedation,Reference Baker, Lovell, Easton and Harris32, Reference Cleary, Horsfall, Jackson, O'Hara-Aarons and Hunt52 whereas others felt empowered to decide on timing and dose of medication when administered on an ‘as needed’ basis.Reference Baker, Lovell, Easton and Harris32 However, patients also voiced concerns that included lack of communication about consent, information about medication and advanced wishes;Reference Gilburt, Rose and Slade39, Reference Cleary, Horsfall, Jackson, O'Hara-Aarons and Hunt52 lack of confidentiality regarding medication;Reference Baker, Lovell, Easton and Harris32, Reference Jones and Crossley42 perceived overmedicationReference Baker, Lovell, Easton and Harris32, Reference Gilburt, Rose and Slade39, Reference Hughes, Hayward and Finlay41, Reference Ridley and Hunter46, Reference Russo and Rose47, Reference Cleary, Horsfall, Jackson, O'Hara-Aarons and Hunt52, Reference McGuinness, Dowling and Trimble69 (including overlooked or ignored reports of side effects);Reference Wyder, Bland, Blythe, Matarasso and Crompton28, Reference Hughes, Hayward and Finlay41 and fear of harm during forced medication,Reference Katsakou, Rose, Amos, Bowers, McCabe and Oliver20, Reference Baker, Lovell, Easton and Harris32, Reference Gilburt, Rose and Slade39, Reference Donald, Duff, Lee, Kroschel and Kulkarni54, Reference Sibitz, Scheutz, Lakeman, Schrank, Schaffer and Amering60, Reference Looi, Engström and Sävenstedt78 for example patients in crisis reported a fear of being raped by staff or of dying.Reference Katsakou, Rose, Amos, Bowers, McCabe and Oliver20, Reference Hughes, Hayward and Finlay41, Reference Looi, Engström and Sävenstedt78, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88
Seclusion
Some patients reported seclusion as helpful or necessaryReference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Ntsaba and Havenga57, Reference Mayers, Keet, Winkler and Flisher79, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88 and that they felt safe as staff were nearby.Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Ntsaba and Havenga57, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88, Reference Iversen, Sallaup, Vaaler, Helvik, Morken and Linaker90 Patient concerns included having insufficient information about the reasons for seclusionReference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Ridley and Hunter46, Reference Ntsaba and Havenga57, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88 before or after the event.Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Ntsaba and Havenga57 Seclusion was perceived as a punishmentReference Mayers, Keet, Winkler and Flisher79 and associated with limited contact;Reference Ntsaba and Havenga57, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88 lack of concern by staff;Reference Holmes, Kennedy and Perron89 degradation and humiliation, e.g. lack of facilitiesReference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Ntsaba and Havenga57, Reference Holmes, Kennedy and Perron89 or being stripped of clothing in front of staff members;Reference Thibeault, Trudeau, d'Entremont and Brown61, Reference Mayers, Keet, Winkler and Flisher79, Reference Holmes, Kennedy and Perron89, Reference Meehan, Vermeer and Windsor91 and violation of rightsReference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88 and dignity.Reference Thibeault, Trudeau, d'Entremont and Brown61
Restraint
Restraint was described as forcible manual or mechanical restraint and typically involved several staff, mostly nursesReference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Sibitz, Scheutz, Lakeman, Schrank, Schaffer and Amering60, Reference Looi, Engström and Sävenstedt78, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88, Reference O'Brien and Cole92 but occasionally security staff.Reference Looi, Engström and Sävenstedt78, Reference O'Brien and Cole92 Restraint was described negativelyReference Whittington, Bowers, Nolan, Simpson and Neil25, Reference Bonner, Lowe, Rawcliffe and Wellman33, Reference Looi, Engström and Sävenstedt78 and fear of restraint prevented patients from seeking help earlier.Reference Bonner, Lowe, Rawcliffe and Wellman33 There was a risk of harm if mechanical restraints were used,Reference Chien, Chan, Lam and Kam87 although these were not used in all countries. Talking with staff following restraint or being allowed to examine records of the event was considered helpful.Reference Bonner, Lowe, Rawcliffe and Wellman33
In addition to the use of coercive measures, patients also described perceived punishment by staffReference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19, Reference Chorlton, Smith and Jones35, Reference Hughes, Hayward and Finlay41, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80, Reference Meehan, Vermeer and Windsor91 in the form of the removal of leave entitlements,Reference Chorlton, Smith and Jones35 removal of furniture and personal itemsReference Hughes, Hayward and Finlay41, Reference Meehan, Vermeer and Windsor91 and not being able to stay up in the evening.Reference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 Patients described this as a violation of their rights.Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Ntsaba and Havenga57, Reference Robins, Sauvageot, Cusack, Suffoletta-Maierle and Frueh58, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88
A healthy, safe and enabling physical environment and ward milieu
The third main theme focused on a healthy, safe and enabling environment. This contributed to how relatives felt when visiting,Reference O'Brien and Cole92 how patients felt about themselvesReference Gilburt, Rose and Slade39 and how they reacted to treatment.Reference Cutting and Henderson36, Reference Gilburt, Rose and Slade39, Reference Jones and Crossley42 Johansson et al (2003)Reference Johansson and Eklund63 argued that the physical environment was as important to patients as receiving satisfactory care. A number of studies reported that patients saw hospital as a ‘sanctuary’Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 or a ‘safe space’Reference Thomas, Shattell and Martin62 where they could have time to reflect away from day-to-day stressors,Reference Fenton, Larkin, Boden, Thompson, Hickman and Newton38, Reference Borge and Hummelvoll50 be kept safeReference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19, Reference Gilburt, Rose and Slade39, Reference Stenhouse48, Reference Donald, Duff, Lee, Kroschel and Kulkarni54 and experience a caring, therapeutic environment.Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80
Patients felt that their in-patient care pathway was aided by connection to the ‘real world’Reference Thibeault, Trudeau, d'Entremont and Brown61 and that being made to feel ‘normal’Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Wyder, Bland, Blythe, Matarasso and Crompton28, Reference Borge and Fagermoen51, Reference Lilja and Hellzen77 was important. This included being allowed to walk around hospital grounds.Reference Gilburt, Rose and Slade39, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 Older establishments often had extensive grounds and patients reported that access to these spaces resulted in less need for medication.Reference Baker, Lovell, Easton and Harris32 Access to a place of worship was comforting,Reference Borge and Fagermoen51, Reference Greenwood, Hussain, Burns and Raphael68 as was freedom to make small decisionsReference Alexander31, Reference Hughes, Hayward and Finlay41 such as making snacksReference Thomas, Shattell and Martin62 or hot drinks.Reference Cutting and Henderson36 Private bedrooms were important,Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 being near windows enabled ward-bound patients to enjoy the outside and fresh air,Reference Shattell, Melanie Andes and Thomas83 and appropriate use of colour was described as conducive to recovery.Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 An environment where staff and patients mixed together reduced feelings of stigmaReference Borge and Fagermoen51 and encouraged favourable interactions.Reference Johansson and Eklund63
Patients reported several environmental problems that were not conducive to recovery-focused care. Some of these were associated with arguments and violence between patients.Reference Cutting and Henderson36, Reference Gilburt, Rose and Slade39, Reference Stenhouse48 Other environmental problems included noise from doorbells, alarms and telephones.Reference Lindgren, Aminoff and Graneheim82 Poor positioning of the nurses' stations often created physical divisions between patients and staff, reducing interaction.Reference Thibeault, Trudeau, d'Entremont and Brown61, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80, Reference O'Brien and Cole92 Communal spaces sometimes lacked privacy for visiting relatives or opportunities for physical activity,Reference Kennedy and Fortune49 especially for those under close observation.Reference O'Brien and Cole92
There were also contradictory reports. In several studies, some patients described hospital as a place of confinement rather than therapy.Reference Katsakou, Marougka, Garabette, Rost, Yeeles and Priebe19, Reference Wyder, Bland, Herriot and Crompton29, Reference Cutting and Henderson36, Reference Duggins and Shaw37, Reference Gilburt, Rose and Slade39, Reference Jones and Crossley42, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 There were analogies with prisonReference Wyder, Bland, Herriot and Crompton29, Reference Cutting and Henderson36, Reference Gilburt, Rose and Slade39, Reference Jones and Crossley42, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 and punishment.Reference Duggins and Shaw37, Reference Gilburt, Rose and Slade39 This was particularly so in secure units with a lack of outside spaceReference Gilburt, Rose and Slade39 and where more patients were admitted compulsorily.Reference Wyder, Bland, Herriot and Crompton29
Ward milieu
Related to environment was the experience of ward milieu, which was shaped by the conduct of staff. Staff provided structure, order and safetyReference Lindgren, Aminoff and Graneheim82 and were responsible for creating a congenial atmosphere.Reference Donald, Duff, Lee, Kroschel and Kulkarni54 Feeling safe was a prime concern to patientsReference Stenhouse48, Reference Cleary, Horsfall and Hunt65 who perceived wards to be safe when they viewed staff as trustworthy,Reference Chorlton, Smith and Jones35 caring and supportive.Reference Chorlton, Smith and Jones35, Reference Fenton, Larkin, Boden, Thompson, Hickman and Newton38 Wards were sometimes criticised as being too busyReference Cutting and Henderson36, Reference Kennedy and Fortune49, Reference Donald, Duff, Lee, Kroschel and Kulkarni54 and reactive to events such as restraint,Reference Lucas and Stevenson56, Reference Mayers, Keet, Winkler and Flisher79, Reference O'Brien and Cole92 seclusionReference Meehan, Vermeer and Windsor91 or violence.Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Robins, Sauvageot, Cusack, Suffoletta-Maierle and Frueh58, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 Patients felt vulnerable to the latter,Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Duggins and Shaw37, Reference Gilburt, Rose and Slade39 fearful of other patientsReference Kennedy and Fortune49, Reference Looi, Engström and Sävenstedt78 and worried about security of belongings.Reference Cutting and Henderson36, Reference Cleary, Horsfall and Hunt65, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 Fear contributed to withdrawing within the wardReference Kennedy and Fortune49, Reference Kulkarni, Gavrilidis, Lee, Van Rheenen, Grigg and Hayes81 or leaving hospital.Reference Duggins and Shaw37, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80
Ward routines also shaped patients' experiences. The dayReference Borge and Fagermoen51 was often structured to include individual and group therapies as well as other activities, e.g. puzzles, conversation or listening to music.Reference O'Brien and Cole92 Evenings were typically less structured.Reference Borge and Fagermoen51 Some patients relished the leisure timeReference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Fenton, Larkin, Boden, Thompson, Hickman and Newton38, Reference Borge and Hummelvoll50, Reference Donald, Duff, Lee, Kroschel and Kulkarni54 and some took this as a time for personal reflection.Reference Fenton, Larkin, Boden, Thompson, Hickman and Newton38, Reference Borge and Fagermoen51, Reference Ntsaba and Havenga57 However, others were uneasyReference Fenton, Larkin, Boden, Thompson, Hickman and Newton38, Reference Borge and Fagermoen51 and reported insufficientReference Cutting and Henderson36, Reference Kennedy and Fortune49 activity. Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Gilburt, Rose and Slade39, Reference Kennedy and Fortune49, Reference Greenwood, Hussain, Burns and Raphael68 The location of the hospital – being close to family – was important to patientsReference Mayers, Keet, Winkler and Flisher79 and they appreciated the inclusion of, and support from, families.Reference Kauppi, Hätönen, Adams and Välimäki22, Reference Fenton, Larkin, Boden, Thompson, Hickman and Newton38, Reference Cleary, Hunt, Escott and Walter53
Boredom
‘Boredom’ or having little to do was mentioned in several studies.Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Stewart, Burrow, Duckworth, Dhillon, Fife and Kelly27, Reference Hughes, Hayward and Finlay41, Reference Borge and Fagermoen51, Reference Donald, Duff, Lee, Kroschel and Kulkarni54, Reference Roe and Ronen59, Reference Greenwood, Hussain, Burns and Raphael68, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80, Reference Lindgren, Aminoff and Graneheim82, Reference Shattell, Melanie Andes and Thomas83, Reference Meehan, Vermeer and Windsor91 Patients suggested that inactivity slowed the in-patient care pathway,Reference Roe and Ronen59 reduced self-efficacy,Reference Hughes, Hayward and Finlay41 exacerbated symptomsReference Muir-Cochrane, Oster, Grotto, Gerace and Jones80 and was related to aggression and violence on the ward.Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23 Some patients reported that inactivity encouraged poor health outcomes, e.g. saying that they would eat, sleep or smoke but not exercise.Reference Kontio, Joffe, Putkonen, Kuosmanen, Hane and Holi24, Reference Roe and Ronen59, Reference Muir-Cochrane, Oster, Grotto, Gerace and Jones80, Reference Shattell, Melanie Andes and Thomas83
Authentic experiences of patient-centred care
The final theme brought together a collection of sub-themes focused on authentic experiences of patient-centred care, which included shared decision-making, sensitivity to gender and culture and the provision of information.
Shared decision-making
Two studies reported that patients’ involvement in treatment decisions was associated with positive experiences of care.Reference Borge and Hummelvoll50, Reference Cleary, Horsfall and Hunt65
Gender and cultural differences
Patients wanted to be understood and seen as individuals, and this was framed in respect of their gender, ethnicity and religion.Reference Bonner, Lowe, Rawcliffe and Wellman33, Reference Bowl34, Reference Greenwood, Hussain, Burns and Raphael68, Reference Looi, Engström and Sävenstedt78 Some patients described cultural differences in perceptions of privacy, and reported concern that staff had not recognised or responded to their discomfort in accepting care from differently gendered staff,Reference Greenwood, Hussain, Burns and Raphael68 for example during restraint and sedation,Reference Bonner, Lowe, Rawcliffe and Wellman33 or for women with a history of sexual abuse by male perpetrators.Reference Looi, Engström and Sävenstedt78 More positively, female patients tended to prefer single-gender wards (where they felt saferReference Cutting and Henderson36). Where this was not available, female patients were satisfied on mixed wards if they had access to a quiet room, if their privacy was respected and if they had access to personal hygiene products.Reference Kulkarni, Gavrilidis, Lee, Van Rheenen, Grigg and Hayes81 Faith also mattered: prayer and rituals (e.g. hand washing) offered comfort to some patientsReference Greenwood, Hussain, Burns and Raphael68 but were not always understood or accommodated by staff.Reference Bowl34
Provision of information
There were several reports in which patients felt they had not received sufficient information about their diagnosis,Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Cleary, Horsfall and Hunt65, Reference McGuinness, Dowling and Trimble69, Reference Chien, Chan, Lam and Kam87 treatment,Reference Katsakou, Rose, Amos, Bowers, McCabe and Oliver20 treatment plan,Reference Kontio, Anttila, Lantta, Kauppi, Joffe and Valimaki23, Reference Baker, Lovell, Easton and Harris32, Reference Cleary, Horsfall, Jackson, O'Hara-Aarons and Hunt52, Reference Ntsaba and Havenga57, Reference Sibitz, Scheutz, Lakeman, Schrank, Schaffer and Amering60, Reference Cleary, Horsfall and Hunt65, Reference McGuinness, Dowling and Trimble69, Reference Chien, Chan, Lam and Kam87, Reference Ezeobele, Malecha, Mock, Mackey-Godine and Hughes88, Reference Iversen, Sallaup, Vaaler, Helvik, Morken and Linaker90, Reference Meehan, Vermeer and Windsor91 choices or rights.Reference Katsakou, Rose, Amos, Bowers, McCabe and Oliver20, Reference Ridley and Hunter46, Reference Cleary, Hunt, Escott and Walter53, Reference Brunero, Lamont and Fairbrother64, Reference Thapinta, Anders, Wiwatkunupakan, Kitsumban and Vadtanapong86 Timing was also important as patients found it difficult to understand or remember this information when unwell.Reference Nolan, Bradley and Brimblecombe45, Reference McGuinness, Dowling and Trimble69
Discussion
The aim of this review was to identify the most salient aspects of in-patient experience to support improvements in care in ways that are conducive to recovery-focused care. To the best of our knowledge this is the largest review of its type in the UK and internationally, with 72 included studies, of which a third were from the UK. A strength of the review was the involvement of the PPIRG who provided important face and content validity checks and were able to identify additional areas of experience, such as boredom, which could be built into the main review.
The review makes an important contribution to the field of mental health in-patient experiences through the identification of four key, interlinked themes: the importance of high quality relationships; averting negative experiences of coercion; a healthy, safe and enabling physical environment and ward milieu; and authentic experiences of patient-centred care. These themes and their associated sub-themes represent the active ingredients of a high-quality mental health in-patient experience (as well as the common causes of very poor experiences). The identified themes can be used to design and deliver high-quality services, provide content for the development of robust patient experience questionnaires or inform qualitative methods that aim to evaluate salient aspects of patient experience. They provide evidence for the development of practice guidance that supports the implementation of high-quality services.
A consistent thread across all four themes was the key role of staff in facilitating a high-quality patient experience. However, staff operate within the context of a wider system that needs to support the delivery of care. It was not always possible to understand this context from the studies reviewed as many did not provide such wider contextual information. This would have been useful, particularly in understanding why some studies reported very negative experiences and others reported more positive experiences. Future studies might consider reporting contextual information to aid interpretation.
It is important to note that the findings of studies relating to discharge appeared to be influenced by the research design, with questionnaires identifying high levels of satisfaction whereas experiences captured using qualitative methods were described differently. Future studies should pay careful attention to the way in which design might affect the reporting of experiences.
Limitations
A limitation of this review, common to all secondary research, is that it is reliant on the conduct and content of primary studies which may have included biases that we could not account for. Few studies mentioned the involvement of patients in data collectionReference Katsakou, Rose, Amos, Bowers, McCabe and Oliver20, Reference Gilburt, Rose and Slade39, Reference Ridley and Hunter46, Reference Mayers, Keet, Winkler and Flisher79 and research design,Reference Katsakou, Rose, Amos, Bowers, McCabe and Oliver20, Reference Stewart, Burrow, Duckworth, Dhillon, Fife and Kelly27, Reference Gilburt, Rose and Slade39, Reference Ridley and Hunter46, Reference Mayers, Keet, Winkler and Flisher79 and the study authors’ professional perspective is often unreported. It is therefore unclear to what extent a study finding reflects the patient voice or whether it predominantly reflects the researchers’ interpretation of their data. Ensuring greater clarity about whose voice is represented, as a means of minimising bias, represents an important methodological challenge for future research. In future reviews, the case could be made to focus on studies where there is evidence of a strong patient voice in the conduct and interpretation of the study.
Although we used the concept of data saturation to decide when to stop data extraction, it is always possible that other papers contained nuances in themes that were unintentionally omitted. The risk of bias in this review may have been partially mitigated by our scoping review which identified key authors and included a citation search of their papers and other literature reviews. In addition, the PPIRG provided important assurance of face and content validity.
Our study relies on secondary analysis of qualitative data. The findings we have presented are drawn from the reports from participants in primary studies. Many of these claims (e.g. the perceived role of good relationships in reducing a range of unwanted outcomes, the role of boredom in exacerbating those outcomes) are reported across multiple primary sources. However, an important limitation of secondary research involves the gaps that exist in studies. A key gap in this review was the lack of experiences from people of Black and minority ethnic groups, which appears to be under-researched. Future studies should ensure they build ethnicity into their design.
Funding
S.S. is part-funded by NIHR CLAHRC West Midlands. K.B. was (in part) supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) North Thames at Bart's Health NHS Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2019.22
Acknowledgements
We thank the Patient and Carer Reference Group members, who have been key to the development of this review. We thank them for all their inputs and insights. The results are stronger through their involvement.
Appendix
Table A.1 Other systematic reviews






eLetters
No eLetters have been published for this article.