Although treatment-resistant depression is a heterogeneous condition, it is typically defined as a depressive disorder that fails to show satisfactory response (optimally remission) to at least one adequately given antidepressant medication. Reference Thase and Rush1,Reference Fekadu, Wooderson, Donaldson, Markopoulou, Masterson and Poon2 It is rightly regarded as a significant clinical and public health challenge Reference Greden3 owing to its common occurrence, Reference Souery, Papakostas and Trivedi4,Reference Trivedi, Rush, Wisniewski, Nierenberg, Warden and Ritz5 association with serious complications such as self-harm and suicide, and higher level of comorbidity and service utilisation. Reference Fava6–Reference Sackeim10
Treatment-resistant depression has attracted an increasing level of research interest in the past two decades. However, virtually no two studies have defined treatment-resistant depression or its outcomes consistently. Reference Fekadu, Wooderson, Markopoulo, Donaldson, Papadopoulos and Cleare11 Furthermore, other than in the context of acute treatment trials, there are no systematic reports on the predictors of medium- and longer-term outcomes. Reference Fekadu, Wooderson, Markopoulo, Donaldson, Papadopoulos and Cleare11 Understanding factors associated with outcome is important in order to better understand the aetiology of the disorder, and to identify potential targets for therapeutic intervention. In this report we describe the findings from a study of the longer-term outcome of treatment-resistant depression, together with the clinical and psychosocial factors that may be associated with outcome, in a well-characterised sample of patients with treatment-resistant depression. Specifically, we aimed to determine the factors associated with remission and recovery, and with illness persistence. The sample was drawn from a tertiary in-patient service in the UK. Because such patients may have a number of pathways to treatment-resistant depressive symptoms, and to maintain a naturalistic and generalisable sample, we included patients with a bipolar diathesis as well as patients in whom depression occurred in the context of another psychiatric disorder. This is particularly relevant given the recent findings that bipolar symptomatology is especially common in those with treatment-resistant depression. Reference Keller, Lavori, Friedman, Nielsen, Endicott and McDonald-Scott12
Method
Design
The study was a prospective follow-up of patients discharged from a tertiary unit. Follow-up data were collected using both longitudinal and cross-sectional assessments. The report presented here relies on longitudinal assessments using the Longitudinal Interval Follow-up Evaluation (LIFE) chart and Psychiatric Status Rating (PSR). Reference Ruhé, van Rooijen, Spijker, Peeters and Schene13
Participants
The cohort consisted of patients discharged from a tertiary unit for treatment-resistant mood disorders in the UK. Treatment-resistant depression was defined using the Maudsley Staging Method (MSM), Reference Fekadu, Wooderson, Donaldson, Markopoulou, Masterson and Poon2 a multidimensional tool that incorporates treatment failure (antidepressants, augmentations and electroconvulsive therapy (ECT)), duration and severity of depression to grade level of treatment resistance (Table 1). Reference Fekadu, Wooderson, Donaldson, Markopoulou, Masterson and Poon2,Reference Fekadu, Wooderson, Markopoulo and Cleare14 The mean severity of the level of resistance measured using the MSM was 10.1 (s.d. = 2.2), suggesting that most participants had moderately severe or severe treatment-resistant depression. The MSM was developed based on theoretical considerations, and the staging method has shown good predictive validity for both short-term and longer-term outcomes. Reference Fekadu, Wooderson, Donaldson, Markopoulou, Masterson and Poon2,Reference Li, Bai, Huang, Chen, Chen and Cheng15 As the MSM incorporates failure of antidepressants and of augmentation strategies and mood stabilisers, we have used it for staging bipolar treatment-resistant depression as well, particularly as there is as yet no widely accepted differential definition of treatment-resistant bipolar depression. We also note accumulating evidence that a bipolar diathesis may be more common in treatment-resistant depression, and that treatment non-response is more common in bipolar depression. Reference Keller, Lavori, Friedman, Nielsen, Endicott and McDonald-Scott12 In order to maximise diagnostic accuracy, all patients undertook a detailed diagnostic assessment process over at least 4 weeks as described previously. Reference Wooderson, Juruena, Fekadu, Commane, Donaldson and Cowan16 Follow-up assessment took place a minimum of 1 year after discharge from hospital except in individuals who for practical reasons were followed up 8–11 months post-discharge.
TABLE 1 Summary of scoring system and domain components of the Maudsley Staging Method

| Score range | |
|---|---|
| Domains | |
| Antidepressants | 1-5 |
| Failure of augmentations | 0-1 |
| Failure of electroconvulsive therapy | 0-1 |
| Chronicity | 1-3 |
| Severity | 1-5 |
| Total score | 3-15 |
| Severity categories | |
| Mild | 3-6 |
| Moderate | 7-10 |
| Severe | 11-15 |
Outcome definitions
The main outcomes of interest were remission, recovery, relapse and persistence of depressive episode (Table 2). These outcomes were drawn from the PSR scores and were consistent with the operational criteria suggested in previous outcome studies of depressive disorders. Reference Frank, Prien, Jarrett, Keller, Kupfer and Lavori17,Reference Keller18 Remission was defined as maintaining asymptomatic or nearly asymptomatic state for a minimum of 1 month and was considered from the point of discharge. Recovery from an episode was defined by maintaining remission for at least 6 consecutive months at any stage of follow-up. A more stringent criterion defines recovery as achieving continuous remission in the past 6 months of follow-up. Reference Coryell, Endicott and Keller19 For an episode, a patient fulfils diagnostic criteria for a depressive episode according to ICD-10. 20 For a persistent episode, the depressive episode continues throughout the follow-up period. Relapse assumes the participant has developed an episode lasting at least 1 month after attaining full or partial remission. Mortality during this period was also included as a separate adverse outcome.
TABLE 2 Definition of outcome terms with required Psychiatric Status Rating scores, the equivalent ICD-10 status and the minimum duration

| Outcome | Psychiatric Status Rating score |
ICD-10 status | Minimum duration,
months |
|---|---|---|---|
| Remission | 1-2 | Asymptomatic | 1 |
| Partial remission (response/subthreshold) | 3-4 | Symptomatic but below episode level | 1 |
| Episode | 5-7 | Episode criteria | 1 |
| Recovery | 1-2 | Asymptomatic | 6 |
| Relapse | 5-7 | Episode criteria | 1 |
Measurement of outcome
The LIFE chart was administered once at the end of the follow-up period to rate the monthly clinical status of participants using all available information, including data from clinical records and informants. The LIFE allows the weekly or monthly symptomatic state of a patient to be rated retrospectively at follow-up intervals of 6 months or longer (up to 96 months). Reference Ruhé, van Rooijen, Spijker, Peeters and Schene13 Symptoms are ordinarily rated on a six-point scale using the PSR. The PSR ratings are operationally linked to DSM-IV 21 and ICD-10. 20 In this study, we used a modified PSR rating as adapted for a UK study. Reference Kennedy, Abbott and Paykel22,Reference Kennedy and Paykel23 The modification expands the PSR ratings from 6 to 7 scores: a score of 1 or 2 corresponds to remission, a score of 3 or 4 corresponds to response/partial remission with subsyndromal symptomatology, and a score of 5, 6 or 7 corresponds to being in a depressive episode (mild = 5, moderate = 6, severe = 7). The PSR scores were obtained to characterise the monthly clinical status of patients for the interval between discharge from hospital and final follow-up date.
The LIFE chart was administered by two psychiatrists (A.F. and K.M.). The two raters had good interrater reliability (kappa of 0.9, P<0.001 and Spearman's rho of 0.9, P<0.001). The LIFE chart ratings also showed good convergence with concurrently administered cross-sectional clinical scales (the Beck Depression Inventory Reference Beck, Ward, Mendelson, Mock and Erbaugh24 and the 21-item Hamilton Rating Scale for Depression (HRSD) Reference Hamilton25 ) and divergence with functional scales (the Global Assessment of Functioning 21 and the 12-item Short-Form Health Survey Reference Ware, Kosinski and Keller26 ).
Predictors
Based on the outcome literature on depression, three main categories were assessed for predicting relapse and remission: (a) sociodemographic predictors; (b) clinical predictors (severity of prior treatment resistance measured with the MSM; age at onset of depression; symptom severity at discharge; and treatments received during admission); and (c) level of social support and life events. A short self-report questionnaire, the Oslo 3 Support Scale (OSS) Reference Dalgard, Dowrick, Lehtinen, Vazquez-Barquero, Casey and Wilkinson27 was used to assess general social support. The OSS contains 3-items assessing the number of close confidants, perceived level of concern from others and perceived ease of getting help from neighbours. Based on the raw scores, the scale allows a summary score (range 3–14) or categories of social support (strong v. poor) to be generated. To assess life events, we used the List of Threatening Experiences. Reference Brugha, Bebbington, Tennant and Hurry28
The effect on remission of individual psychotropic medications, either switching class of antidepressant or using a first- or second-line choice for treatment-resistant depression as listed in the Maudsley Prescribing Guidelines, Reference Taylor, Paton and Kapur29 was determined if the medication was given to at least ten patients at adequate doses. The analysis was essentially exploratory because of the relatively small number of patients receiving the individual medications. However, despite the limitation of the sample size and the fact that this was not a treatment trial, any supportive evidence regarding effective intervention in this difficult-to-treat diagnostic subgroup is useful.
Data management
Data were entered in to the Statistical Package for Social Sciences version 15 for Windows. Analysis used SPSS supplemented with STATA, version 11 for Windows (Statacorp). Although some studies in chronic depression and treatment-resistant depression report on pooled data, Reference Keller18,Reference Dunner, Rush, Russell, Burke, Wooodard and Wingard30 we stratified analysis according to discharge diagnosis (unipolar, bipolar and secondary treatment-resistant depression Reference Scott31 ) in addition to presenting results on pooled data. The term ‘secondary’ was used in the chronological and not necessarily in the aetiological sense; for example, when treatment-resistant depression developed in the context of an obsessive–compulsive disorder or personality disorder that had started first. For the main data analysis, we employed the Cox multivariate model to determine the independent effect of predictive factors on survival status in remission or in depressive episode.
All patients with potential to relapse into a full episode (40 patients discharged in remission and 36 patients in partial remission as well as 19 patients that achieved full or partial remission during follow-up) were included in the survival analysis. The focus of this study was on depression, and we have not included manic or hypomanic relapses in the analysis. Nevertheless, only two patients had hypomanic and two patients had manic relapses during the follow-up period.
All study procedures were approved by the local ethics committee and all participants provided written, informed consent (ethics approval numbers 285/03 and 322/03).
TABLE 3 Sociodemographic and clinical characteristics of study sample stratified by diagnostic subtype

| Treatment-resistant depression subtype | ||||||
|---|---|---|---|---|---|---|
| Total | Unipolar | Bipolar | Secondary | χ2/F | P | |
| Gender, n (%) | ||||||
| Male | 30 (25.4) | 17 (22.1) | 6 (22.2) | 7 (50) | 5.06 | 0.08 |
| Female | 88 (74.6) | 60 (77.9) | 21 (77.8) | 7 (50) | ||
| Marital status, n (%) | ||||||
| Married | 66 (55.9) | 48 (62.3) | 15 (55.6) | 3 (21.4) | 8.05 | 0.028 |
| Single/post-marital | 52 (44.1) | 29 (37.7) | 12 (44.4) | 11 (78.6) | ||
| Employment, n (%) | ||||||
| Unemployed | 80 (67.8) | 52 (67.5) | 16 (59.3) | 12 (85.7) | 2.9 | 0.22 |
| Employed | 38 (32.2) | 25 (32.5) | 11 (40.7) | 2 (14.3) | ||
| Ethnicity, n (%) | ||||||
| White British | 111 (94.1) | 73 (94.8) | 26 (96.3) | 12 (85.7) | 1.41 | 0.31 |
| Other | 7 (5.9) | 4 (5.2) | 1 (3.7) | 2 (14.3) | ||
| Any life event 12 months to assessment,Footnote a n (%) | 81 (75.7) | 50 (73.5) | 21 (84) | 10 (71.4) | 1.25 0.54Footnote b | |
| Age, years: mean (s.d.) | 47.8 (12.4) | 48.9 (12.7) | 49.1 (11.5) | 38.9 (9.0) | 4.31 | 0.02 |
| Age at onset of depression, years: mean (s.d.) | 29.1 (13.0) | 31.5 (13.1) | 26.4 (12.7) | 19.3 (5.5) | 5.59 | 0.01 |
| Years in education, mean (s.d.) | 13.1 (3.3) | 12.8 (3.3) | 13.6 (3.3) | 13.5 (3.8) | 0.676 | 0.511 |
| Duration (current episode), years: median (IQR) | 5.5 (6.6) | 4.0 (2.0-8.0) | 1.0 (0.0-1.0) | 10.5 (3.0-18.5) | 27.88Footnote b | <0.001 |
| Duration of illness, years: mean (s.d.) | 18.9 (14.1) | 17.5 (14.5) | 22.7 (13.4) | 24.9 (19.9) | 1.24 | 0.29 |
| Duration of admission, weeks: mean (s.d.) | 26.8 (20.1) | 27.3 (21.6) | 26.4 (15.9) | 24.9 (19.9) | 0.09 | 0.91 |
| Admission HRSD, mean (s.d.) | 20.5 (6.4) | 21.1 (6.1) | 20.2 (6.6) | 17.6 (7.2) | 1.84 | 0.16 |
| Discharge HRSD, mean (s.d.) | 13.6 (7.3) | 14.5 (7.2) | 9.2 (6.1) | 17.1 (6.3) | 6.77 | 0.002 |
| Number of prior antidepressant trials, mean (s.d.) | 5.9 (3.5) | 6.3 (3.7) | 4.1 (2.6) | 6.3 (3.6) | 3.50 | 0.03 |
| Total number of prior medication trials, mean (s.d.) | 12.0 (6.5) | 12.3 (6.8) | 11.1 (5.9) | 12.0 (5.9) | 0.27 | 0.76 |
| Duration of follow-up, months: mean (s.d.) | 39.1 (22.0) | 40.7 (21.6) | 31.0 (18.5) | 46.0 (27.3) | 2.80 | 0.07 |
HRSD, Hamilton Rating Scale for Depression; IQR, interquartile range.
a Total denominator, n = 107 (missing data for 11 individuals: 9 unipolar and 2 bipolar).
b Kruskal-Wallis test.
Results
Sociodemographic and clinical characteristics of cohort
Of the 150 patients discharged with treatment-resistant depression and approached, 118 (78.7%) were successfully followed-up. Reasons for non-participation in the study were: refused to take part (n = 7), not traced because of change of address (n = 8), deceased (n = 13) and incomplete data (n = 4). There was no significant difference in all baseline characteristics between participants and non-participants except for duration of admission, which was longer for participants (median 24.0 weeks, interquartile range (IQR) 25.0 weeks) than non-participants (median 9.5 weeks, IQR = 21.0) (P<0.01).
The baseline sociodemographic and clinical details of the 118 included participants are presented in Table 3. Participants had highly treatment-resistant illness, with 65.5% having had a history of treatment with ECT, and the mean number of prior antidepressant treatments for the admission episode being 5.9 (s.d. = 3.5). Additionally, 60% of the sample had history of a suicide attempt. The majority of the cohort was female, married or stably cohabiting, and unemployed. The mean duration of illness was nearly 20 years, and the median duration of index (admission) episode was 3 years (IQR = 7). At discharge, 33.9% (40/118) were in remission, while 30.5% (36/118) and 35.6% (42/118) were in partial remission and in depressive episode respectively.
Participants were followed up for a mean of 39.1 months (s.d. = 22.0), ranging from 8 to 84 months. The mean HRSD-21 for the whole group was 20.5 (s.d. = 6.4), higher for unipolar treatment-resistant depression (mean 21.1, s.d. = 6.1) and lower for secondary treatment-resistant depression (mean 17.6, s.d. = 7.2), although the differences were not statistically significant (Table 3).
Pharmacological treatments
The main antidepressant switches were to monoamine oxidase inhibitors (MAOIs) (n = 16), duloxetine (n = 22) tricyclic antidepressants (n = 28), mirtazapine (n = 10) and venlafaxine (n = 26), whereas augmentation strategies involved the use of lithium (n = 23), lamotrigine (n = 50), thyroid hormone (n = 16) and atypical antipsychotics (n = 25). All the major MAOI classes were used (moclobemide, phenelzine, tranylcypromine and isocarboxazid), although phenelzine was the most common. Amitriptyline and imipramine were the two tricyclic antidepressants commonly used. The main atypical antipsychotics used for augmentation were olanzapine, risperidone, quetiapine and aripiprazole. Minimum dose and duration to define an adequate trial was based on the Maudsley Prescribing Guidelines, Reference Taylor, Paton and Kapur29 supplemented by the Antidepressant History Form Reference Sackeim32 and the British National Formulary. 33
Main outcomes
Details are presented in Fig. 1 and Table 4. Overall, 48.3% (n = 57) of the cohort met recovery criteria, and 11.9% (n = 14) had met remission criteria without ever meeting recovery criteria. Of those who met only remission criteria, all except one participant had been in remission for 2 months or longer. Thus, if recovery was defined as achieving remission at least for 2 consecutive months as used in some outcome studies of chronic affective disorders, Reference Coryell, Endicott and Keller19 the proportion achieving recovery would rise to 59.3% (n = 70/118). On the other hand, if recovery was defined more stringently as achieving remission in the last 6 months of follow-up, Reference Coryell, Endicott and Keller19 the figure for recovery drops to 31.4% (n = 37). In terms of unfavourable outcome, 39.8% had persistent symptomatology throughout the follow-up period, either because of persistent subthreshold/subsyndromal symptoms (19.5%) or persistent depressive episode (20.3%). Nearly two-thirds of the follow-up time (60.7%) was spent in a symptomatic state: 36.1% in episode and 24.6% in subthreshold state (Table 4).

FIG. 1 Proportion of participants in various longitudinally defined outcome states stratified by treatment-resistant depression subtype.
Total number of participants: n = 118; unipolar treatment-resistant depression, n = 77; bipolar treatment-resistant depression, n = 28; secondary treatment-resistant depression, n = 14.
TABLE 4 Percentage time spent in various clinical states stratified by diagnosis and discharge status

| Percentage time spent in: | |||
|---|---|---|---|
| Episode | Subthreshold | Remission | |
| Diagnostic subtype of treatment-resistant depression | |||
| Unipolar | 39.9 | 35.5 | 24.4 |
| Bipolar | 23.6 | 49.2 | 25.3 |
| Secondary | 39.1 | 34.8 | 24.7 |
| Clinical status at discharge | |||
| Remission | 9.9 | 10.1 | 78.7 |
| Partial remission | 20.5 | 60.0 | 19.3 |
| Episode | 74.1 | 16.2 | 9.0 |
| Overall | 36.1 | 24.6 | 38.5 |
In a stratified comparison between the diagnostic groups, about three-quarters of participants with bipolar treatment-resistant depression (74.1%, n = 20) had achieved either remission or recovery, whereas the proportion for unipolar (55.8%, n = 43) and secondary treatment-resistant depression (57.1%, n = 8) was comparably lower (Fig. 1). However, the only statistically significant difference in outcome between these groups was the higher proportion of participants with persistent episode in the unipolar (P = 0.02) and secondary treatment-resistant depression groups (P = 0.01) compared with the bipolar treatment-resistant depression group.
Excluding those with persistent episode, 95 participants had the potential to experience relapse; of these, 54.7% (n = 52) experienced a depressive relapse during follow-up.
Mortality
Mortality is one of the indicators of unfavourable outcome in depression. Reference Shergill, Robertson, Stein, Bernadt and Katona34 Thirteen participants died during follow-up: eight from natural causes (primarily cardiovascular) and five from unnatural causes (suicide, n = 3; accidental deaths, n = 2). There was a significant trend for association between discharge status and mortality χ2 = 8.03; P = 0.01). Thus, only two individuals who were discharged in remission died.
Predictors of outcome
Three main factors were associated with achieving remission during follow-up: severity of treatment-resistant depression measured with the MSM, educational achievement and level of social support. Participants with higher levels of treatment resistance were less likely to achieve remission, i.e. had more persistent illness (hazard ratio (HR) = 0.77, 95% CI 0.68–0.99; P = 0.04). Participants with higher educational achievement (HR = 1.17, 95% CI 1.01–1.35; P = 0.03) and those with strong social support (HR = 1.76, 95% CI 1.07–2.89; P = 0.03) were more likely to achieve quicker remission (Table 5). The two factors independently associated with relapse were poor social support (HR = 3.55, 95% CI 1.01–12.54; P = 0.05) and receiving a diagnosis of bipolar depression (HR = 3.39, 95% CI 1.06–10.98). The survival plot is shown in Fig. 2.
TABLE 5 Prediction of remission among those discharged in symptomatic state modelled using the Cox regression methodFootnote a

| Variable | Crude hazard ratio |
95% CI | Adjusted hazard ratio |
95% CI | P |
|---|---|---|---|---|---|
| Gender | 0.95 | 0.40-2.24 | 0.62 | 0.25-1.57 | 0.32 |
| Life event | 1.17 | 0.60-5.08 | 1.02 | 0.33-3.11 | 1.00 |
| Age at onset | 1.60 | 0.99-1.00 | 1.01 | 0.97-1.05 | 0.70 |
| Years of education | 1.16 | 1.04-1.29 | 1.17 | 1.01-1.35 | 0.03 |
| Severity of treatment-resistant depressionFootnote b | 0.77 | 0.65-0.92 | 0.82 | 0.68-0.99 | 0.04 |
| Psychiatric Status Rating at discharge | 0.90 | 0.68-1.17 | 0.89 | 0.39-2.03 | 0.78 |
| Social support | 1.81 | 1.17-2.81 | 1.76 | 1.07-2.89 | 0.03 |
a All variables in the model mutually adjusted.
b Severity of treatment-resistant depression measured with the Maudsley Staging Method.
Use of MAOIs while an in-patient was independently associated with remission at point of discharge controlling for other treatments, particularly for unipolar treatment-resistant depression (odds ratio (OR) = 6.49, 95% CI 1.63–25.91). Similarly, in-patient use of MAOIs (OR = 4.78, 95% CI 1.15–19.85) or duloxetine (OR = 4.60, 95% CI 1.18–17.93) was associated with being in full remission at the time of final follow-up. When analysis was stratified by gender, the effect of duloxetine remained significant only among women (OR = 6.07, 95% CI 1.59–23.17; P = 0.01). Mean doses of MAOIs used were: phenelzine 70 mg; moclobemide 650 mg; tranylcypromine 32.5 mg; and isocarboxazid 40 mg. The mean dose of duloxetine was 98.2 mg. Number of medications received prior to admission was only marginally but negatively associated with achieving remission (OR = 0.92, 95% CI 0.85–1.00).
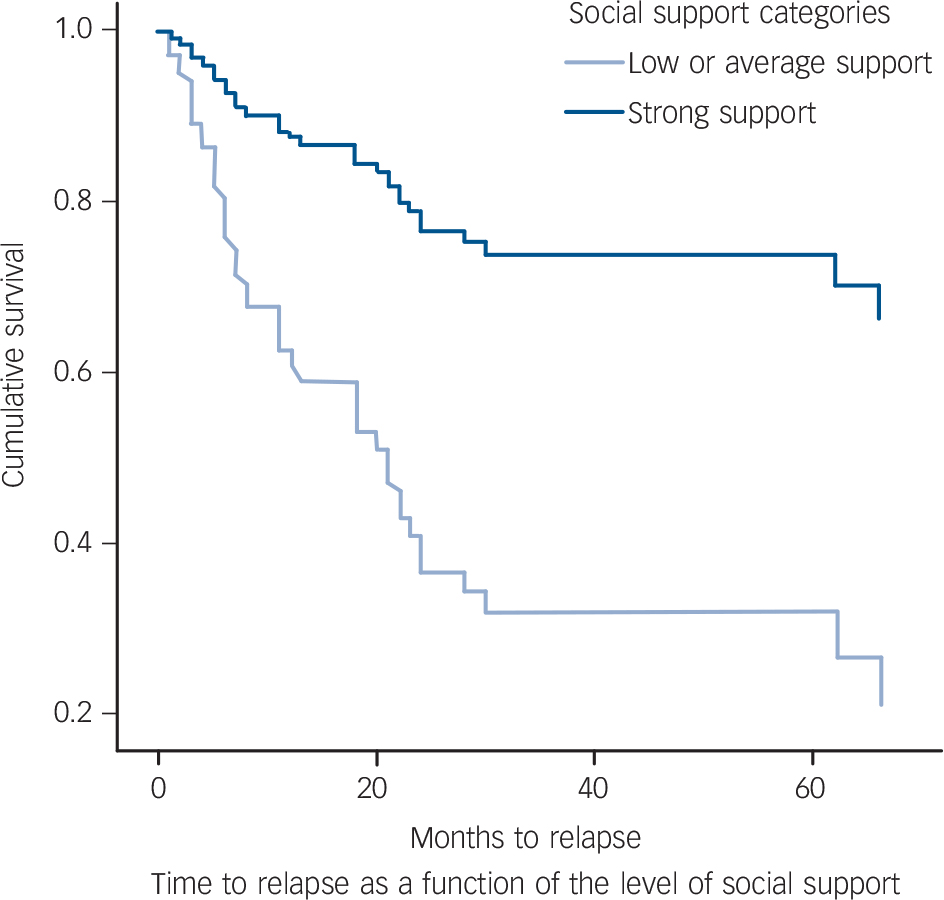
FIG. 2 Survival curves for time to relapse as a function of the level of social support.
Adjusted for years of education, gender, age at onset, discharge clinical status and diagnosis (hazard ratio 3.55, 95% CI 1.01–12.54; P = 0.05).
Discussion
Our study is novel in that it takes a longitudinal perspective on the outcome, and predictors of outcome, in well-defined treatment-resistant depression in a naturalistic setting. The main findings of this study relate: first, to a clearer understanding of the expected outcomes in moderate to severe TRD; and second, to indications of potentially modifiable risk factors that may be amenable to intervention or change in order to improve outcome.
Limitations
Before discussing these results in more detail, some limitations of the study should be highlighted. First, the cohort was identified from a specialist service and is likely to represent the more severe spectrum of illness. Therefore, the results may not fully translate to treatment-resistant depression seen in other settings. Second, the follow-up duration was variable. However, the Cox regression model is suitable for analysis of data with variable duration of follow-up. Third, we could only determine outcomes of 131/150 patients, leaving 19/150 (13%) unaccounted for. It is possible that these patients had worse outcome, particularly those who refused to take part (7/150). If this is the case, then the proportion with a poor outcome would be slightly higher. Finally, the sample size was modest for a detailed analysis on the various treatment-resistant depression subcategories. However, rather than solely looking at all treatment-resistant depression categories together, as has been done in other studies, we opted also to show the outcomes of the categories separately when applicable so that any differences between unipolar, bipolar and secondary treatment-resistant depression could be observed. Moreover, despite these limitations, to our knowledge, this is the first report on the longer-term outcome of explicitly defined treatment-resistant depression and its predictors using well-operationalised outcome criteria.
General outcome
The population has a very high level of treatment-resistant illness with 12 prior failed medication trials and a mean MSM score of 10 as well as history of failed trials with ECT in two-thirds of patients, although the admission HRSD severity level was generally in the mild to moderate range according to National Institute for Health and Clinical Excellence guidance. 35 Admission depression severity may have been influenced by a partial treatment response, which might be expected given the large number of prior treatment exposures. Overall, the proportion achieving remission and recovery (60.2%) over an average follow-up period of 3 years is substantial. However, a high proportion of participants also experienced persistent episode (20.3%) or showed a significant level of persistent and impairing symptomatology (19.5%). This is particularly so for both the unipolar and the secondary treatment-resistant depression group. Additionally, optimal outcome (remission for at least 6 contiguous months) was achieved in under 50% of cases. About 10% of participants died during this follow-up period, most of whom had poorer responses to in-patient treatment. If this latter group was considered also to have unfavourable outcome, the figure for those with the most favourable outcome drops to 43.5% (57/131). This figure would drop further to 38% if those who had refused follow-up assessments or were lost to follow-up were again considered to have had worse outcome. This confirms the serious and chronic nature of treatment-resistant depression and the need to improve on current treatments.
There are no directly comparable studies with which we can compare our findings. One of the few well-designed studies on treatment-resistant depression looked at the 1- to 2-year outcome of patients with moderately advanced unipolar and bipolar treatment-resistant depression in a multicentre study setting. Reference Dunner, Rush, Russell, Burke, Wooodard and Wingard30 The 1- and 2-year remission rates defined with a self-rated measure were very low (3.7% and 7.8% respectively). However, the study was part of a treatment trial and remission was determined for each visit on the basis of the severity of symptoms in the 7 days prior to the visit rather than longitudinally for the whole follow-up duration. Another follow-up study of 66 patients with well-defined treatment-resistant depression (both unipolar and bipolar) followed up patients for 1.1–59.3 months (mean 29.0). Reference Nierenberg, Price, Charney and Heninger36 Outcomes were classified as poor, fair and good, with 71% categorised as having a good or fair outcome. Despite differences in methodology and follow-up duration, these results may be considered roughly comparable to our findings.
A study conducted as part of the National Institute of Mental Health Collaborative Program on the Psychobiology of Depression-Clinical Studies may be compared with our study in methodology, and to some extent in patient sample. Reference Coryell, Endicott and Keller19 This report was based on a 5-year follow-up of 129 patients with chronic affective disorders (unipolar, bipolar and schizoaffective disorders), and employed the LIFE chart method. In this study, 77% of patients followed-up recovered (defined as achieving remission for at least 2 months). When recovery was defined more stringently (achieving remission for the last 6 months of follow-up), about 48% meet recovery criteria. Reference Coryell, Endicott and Keller19 When our outcome criteria were modified to fit the US study, the outcome in our sample is somewhat worse, in terms of both the proportion of patients meeting general recovery criteria (59% v. 77%) and more stringently defined recovery criteria (34.1% v. 48%). One explanation could be the shorter duration of follow-up in our sample, since there is a higher chance of recovery with longer follow-up. It could also be due to the inclusion of patients with more severely treatment-resistant illness in our study, because the US study was a follow-up of patients with chronic depression rather than explicitly defined treatment-resistant depression. The main advantage of our report compared with the US study is that our study deals with a poorly researched patient group (those with treatment-resistant depression) and the details are stratified by diagnostic group rather than based solely on analysis of pooled data.
Prediction of outcome
The main predictors of outcome, specifically predictors of remission and factors predicting early relapse, are consistent with what has been previously reported for depression in general. For example, several studies have reported that social support predicts recovery or treatment response, particularly in the short term. Reference Leskela, Rytsala, Komulainen, Melartin, Sokero and Lestela-Mielonen37–Reference Nasser and Overholser39 Severity of treatment resistance measured with the MSM was also an important predictor of failure to achieve remission or illness persistence. Reference Li, Bai, Huang, Chen, Chen and Cheng15
Our results also show cross-sectional association between certain medication groups (MAOIs and duloxetine) and better outcome. The use of MAOIs is one of the recommended strategies for managing treatment-resistant depression; studies from over two decades ago had indicated the usefulness of MAOIs in non-responsive depression Reference Pare40 or depression with specific symptom profiles. Reference Tyrer41 However, it occurs only as a third-line option (in combination with a tricyclic antidepressant) in the widely used Maudsley Prescribing Guidelines. Reference Taylor, Paton and Kapur29 We suggest that our findings act as a reminder that MAOIs have a place in the management of treatment-resistant depression, and require more systematic investigation.
Clinical implications
In a potentially chronic and relapsing condition such as treatment-resistant depression, studies looking at longitudinal outcome are particularly relevant. The present study represents one of the very few such studies, and confirms the often poor long-term outlook and the need for new treatment approaches to improve outcomes. This is underlined by the association between increasing symptom severity and mortality. Nevertheless, most patients do experience sustained periods of remission. Importantly, we have found that social support influences the long-term outcome of treatment-resistant depression, suggesting that this could be a suitable target for therapeutic intervention. Reference Akiskal, Sadock, Sadock and Ruiz42 There are also suggestions that patients with treatment-resistant depression and a bipolar diathesis may have different long-term trajectories, an area that requires further study using larger sample sizes. Finally, the study highlights the need to further investigate the role of certain medications, particularly MAOIs, in the management of treatment-resistant depression.
Funding
This research was supported by the NIHR Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and the Institute of Psychiatry (King's College London).










eLetters
No eLetters have been published for this article.