There is a recent but rapidly growing literature on the developmental psychopathology of mother–infant relations. One focus of research is the nature of the relationships between troubled mothers and their infants and the potential effects of discordant interactions on the infants’ development. Our aim was to investigate a group of mothers who have not been studied previously in this context – those with borderline personality disorder – in order to determine whether there were patterns of mother–infant interaction that characterised this group and whether there was evidence that any dysfunction might have an impact on infants as young as 2 months old.
METHOD
Background to the study
Early studies of mother–infant interactions revealed the qualities of mutual responsiveness that characterise the communication between ‘typical’ mothers and their infants. With growth of interest in the field of developmental psychopathology over the past two decades, research into the origins and cross-generational implications of psychopathological conditions has prompted investigators to consider infant development from this perspective.
There is already evidence that maternal psychopathology may be associated with patterns of mother–infant interaction that affect infant development. For example, there are now several studies that have reported marked disturbances in mother–infant interactions when mothers have been experiencing an episode of depression, especially when there is social and personal adversity. Depressed mothers have tended to be rated as hostile and intrusive, insensitive, withdrawn or showing negative affect, and infant distress and avoidance have been common (e.g. Reference Cohn, Campbell and MatiasCohn et al, 1990; Reference Murray, Fiori-Cowley and HooperMurray et al, 1996). The impact of maternal psychopathology on infant development has also been studied in relation to mothers with conditions such as eating disorder (Reference Stein, Woolley and CooperStein et al, 1994) and anxiety disorder (Reference Manassis, Bradley and GoldbergManassis et al, 1994).
A second line of evidence concerning the potential significance of maternal psychopathology for infant development begins not with psychiatric diagnosis but with individual differences in mothers’ responses to the Adult Attachment Interview of George et al (Reference George, Kaplan and Main1985). A number of studies have reported that the style with which mothers recall their early childhood is related to aspects of the interpersonal functioning of their infants (Reference van IJzendoornvan IJzendoorn, 1995). Especially impressive in this regard is the evidence that prenatal assessments of mothers’ mental representations of childhood social experiences can predict the separation–reunion reactions of mother–infant pairs over 1 year later (Reference Fonagy, Steele and SteeleFonagy et al, 1991). A plausible explanation for this finding is that the Adult Attachment Interview assesses aspects of the mother's psychological functioning that shape the mother's interactions with her infant, and that such interactions are a major factor in determining the infant's pattern of attachment to the mother later in infancy. As Crandell et al (Reference Crandell, Fitzgerald and Whipple1997) have suggested, to the extent that mothers have a defensive or entangled state of mind regarding attachment, they may either intrude upon or dismiss affective experiences that arise in the context of mother–infant interactions and thereby affect the infants’ ability to integrate and manage their feelings. More specifically with regard to psychopathology, Main & Hesse (Reference Main and Hesse1992) have suggested that mothers who are classified as ‘unresolved’ with respect to trauma and loss are prone to exhibit episodes of frightened/frightening behaviour towards their infants, predisposing to ‘disorganised’ strategies of infant reaction to separation–reunion experiences that are linked with subsequent interpersonal difficulties and conflicts when the infant grows into a young child (e.g. Reference Main and CassidyMain & Cassidy, 1988; Reference Lyons-Ruth, Alpern and RepacholiLyons-Ruth et al, 1993). Here is an instance in which atypical and perhaps dysfunctional qualities of mother–infant interaction may have a significant impact on infant development.
Mothers with borderline personality disorder have not been investigated previously in this context and we chose to study them for three reasons. First, the diagnosis of borderline personality disorder is based on a constellation of clinical features, of which the most important is a chronic instability and impulsivity in the individual's interpersonal relations. By adopting DSM–III–R diagnostic criteria (American Psychiatric Association, 1987), our aim was to constitute a relatively homogeneous group of mothers who have characteristic and severe relationship difficulties that might also find expression in relation to their infants.
Second, psychoanalytical experience and a previous study of our own (Reference Hobson, Patrick and ValentineHobson et al, 1998) suggest that women with borderline personality disorder tend to manifest a characteristic form of disturbed relatedness in their moment-by-moment interpersonal transactions with a psychotherapist. We anticipated that there would be corresponding patterns of relatedness between affected mothers and their infants.
Third, from an attachment perspective, there is evidence that ‘enmeshed’ and ‘unresolved’ patterns of response to the Adult Attachment Interview have a high prevalence in women with borderline personality disorder (Reference Patrick, Hobson and CastlePatrick et al, 1994; Reference Fonagy, Leigh and SteeleFonagy et al, 1996). Attachment research indicates that these categories of mental representation of early social experience predispose to difficulties in mother–infant relations.
In our approach to testing mothers in interaction with their 2-month-old infants, we adopted the methods and measures devised by Murray et al (Reference Murray, Fiori-Cowley and Hooper1996). In contrast to Murray's technique with depressed mothers, however, we decided to focus on infants’ reactions during and after a brief period in which we asked mothers to adopt a ‘still face’. This still-face procedure, which in fact involves a lack of vocalisation as well as a suspension of facial and other gestures while the mother maintains eye contact with her baby, was originally designed to illustrate infant sensitivity to perturbations in expected reciprocal interaction (Reference Tronick, Als and AdamsonTronick et al, 1978). Infants typically respond by making bids to re-engage the mother, and when this fails they show less smiling, become neutral to negative in affect and often turn their gaze away from the mother's face (Reference Carter, Mayes and PajerCarter et al, 1990; Reference Toda and FogelToda & Fogel, 1993; Reference Kogan and CarterKogan & Carter, 1996).
Our intention in adopting this approach was to assess how mother–infant dyads manage a situation of emotional difficulty and conflict. Previous evidence has suggested that the manner in which an infant responds to the still-face challenge is related to a mother's sensitivity, style of control and affect in the mother–infant interaction that precedes it (Reference Carter, Mayes and PajerCarter et al, 1990). In the case of maternal depression, Cohn et al (Reference Cohn, Matias and Tronick1986) reported that infants of depressed intrusive mothers became avoidant during the still-face procedure and infants of depressed withdrawn mothers became distressed and displayed more negative affect and protest. The procedure thus appears to have the potential to highlight the significance of maternal psychopathology for mother–infant relations.
It is also common for there to be carry-over effects from the still-face episode, in that often the infant remains more negative in the face-to-face play that follows (Reference Carter, Mayes and PajerCarter et al, 1990; Reference Toda and FogelToda & Fogel, 1993; Reference Weinberg and TronickWeinberg & Tronick, 1996). Once again there appear to be individual differences among infants that are related to maternal sensitivity. Kogan & Carter (Reference Kogan and Carter1996) reported that infants of mothers who were sensitive, positive and emotionally available during the pre-still-face play displayed more regulated and interpersonally oriented responsiveness (e.g. looking and smiling at mother) during the play that followed the still-face period, whereas infants of mothers who were intrusive and insensitive became either more avoidant or resistant in the post-still-face play. In a recent study, Rosenblum et al (Reference Rosenblum, McDonough and Muzik2002) reported that infants whose mothers described them with ‘balanced’ (rather than ‘disengaged’ or ‘distorted’) narratives were more able to re-establish positive affect after a still-face episode. Accordingly we decided to focus on the post-still-face period as providing a potentially sensitive index of the effects of maternal psychopathology.
In designing the study, we anticipated that there would be difficulty in identifying and recruiting mothers with borderline personality disorder and that we would be restricted to testing modest numbers of participants. With this in mind, we adopted the methodological strategy of making a limited number of predictions in accordance with our hypotheses about the nature of the psychodynamics and interpersonal pathology of the women we were studying; we applied one-tailed non-parametric statistics (Mann–Whitney) to test the directional predictions. We view this as a quasi-experimental design in so far as it depends on a priori stipulation of the factors that are expected to differentiate the groups and allows for relatively limited exploration of multiple interacting variables. Ideally, the method would involve matching the groups on as many other potentially important variables as possible, but we had to accept a degree of compromise in this respect.
Hypotheses and predictions
In framing our small number of predictions, we decided to concentrate on the still-face and post-still-face phases of the procedure. Our rationale in the case of the infants has been outlined already; in the case of the maternal assessments, we anticipated that experience of the still-face period and its possible sequelae might so affect troubled mothers that during the subsequent period of mother–infant interaction they would show disturbed behaviour that otherwise might not be apparent.
On the basis of our hypothesis about the nature of the psychodynamic mechanisms operative in individuals with borderline personality disorder, we predicted that mothers with this disorder would differ from control mothers in relating to their babies in a style that was insensitive in an intrusive (rather than withdrawn) manner.
With regard to the infants of the study, our prediction was that the infants of mothers with borderline personality disorder would become more distressed or disorganised by maternal non-responsiveness, whereas infants in the control group would manifest more robust and persistent attempts to engage in mutual interchange both during and after the still-face period. Our specific predictions for the still-face phase were that, compared with infants in the control group, infants of mothers with borderline personality disorder would show less availability for positive engagement, more negative affect, more looks away (in that these might include avoidant looks) and more dazed looks, reflecting their states of defensive withdrawal and disorganisation.
Our predictions for the post-still-face phase, when mothers were attempting to re-engage their infants, were that the infants would show less positive engagement, more negative affect, more dazed looks, and interactions with their mothers that were poorer in quality.
Procedure
Participants
Eight mothers with borderline personality disorder participated in the study, together with a control group of twelve mothers who had no history of disorder. The participants were recruited through screening at antenatal clinics and through advertisements placed in local publications. Participants were blind to the aims of the study and were told only that the project would be investigating relationships between mothers and infants. In addition, a member of the study team was available to discuss what participation in the study would involve.
Screening of potential participants involved questionnaires for ascertaining demographic information and for providing initial evidence regarding diagnosis. This was the first of two stages in making the diagnosis of borderline personality disorder in accordance with DSM–III–R criteria. In the first stage of screening, mothers were asked to complete the questionnaire version of the Structured Clinical Interview for DSM–III–R (SCID–NP; Reference Spitzer, Williams and GibbonsSpitzer et al, 1990a ) and a questionnaire version of the SCID overview with module A focusing on mood syndromes and module B/C on the ‘psychotic screen’. In this way mothers with a potential diagnosis of borderline personality disorder were identified (i.e. meeting the criteria for borderline personality disorder and no other disorders on the questionnaire). To confirm the diagnosis, these individuals were invited for interview and were given the SCID–II interview (Reference SpitzerSpitzer et al, 1990b ) focusing on personality disorders and the interview version of the SCID overview and modules A and B/C. Only those women meeting the diagnostic criteria for borderline personality disorder and no other diagnostic categories were recruited to the borderline group. Mothers were accepted into the control group provided that on screening and interview they showed no features of borderline personality disorder and did not meet the diagnostic criteria for any other DSM disorder, either current or past.
Infant characteristics are given in Table 1 and maternal characteristics and demographic details are presented in conjunction with measures of maternal relatedness in Table 2. Infants’ ages needed to be corrected for prematurity in the case of two infants in the borderline group and one in the control group. In the borderline group, five infants experienced the mother as the primary caregiver, one infant's care was shared with the father, one also had a nanny and for one the data were missing; in the control group, the mother was the primary caregiver in all cases. The family constellations were as follows: in the borderline group, three of the infants were only children, two infants were the second child and in one case each the infant came third, fifth and sixth in the family; in the control group, seven infants were only children, three were second children and in the remaining cases the infant was the third and fourth child. Three mothers in the borderline and five in the control group reported difficult births, but only one infant of a mother with borderline personality disorder was admitted to a special baby care unit.
Table 1 Infant characteristics

| Dyad | Gender (female:male) | Age (days) | Pregnancy (weeks) | Birthweight (oz) | |||
|---|---|---|---|---|---|---|---|
| Mean (s.d.) | Range | Mean | Range | Mean (s.d.) | Range | ||
| Borderline personality disorder (n=8) | 2:6 | 65 (10) | 54-82 | 39 | 36-42 | 110 (15) | 81-124 |
| Control (n=12) | 5:7 | 66 (7) | 54-75 | 39 | 35-41 | 124 (17) | 93-144 |
Table 2 Maternal non-intrusive sensitivity (post-still-face) and corresponding participant characteristics
| Dyad | Non-intrusive sensitivity (max. score 35) | Social class | Marital status | Ethnicity | Education |
|---|---|---|---|---|---|
| Borderline | 33 | II | Cohabiting | White | University |
| personality | 32 | II | Cohabiting | African—Caribbean | University |
| disorder (n=8) | 30 | II | Cohabiting | White | University |
| 26 | Unemployed | Single | African—Caribbean | University | |
| 26 | md | md | White | md | |
| 22 | I | Cohabiting | White | University | |
| 21 | II | Cohabiting | White | O level1 | |
| 20 | II | Single | African—Caribbean | O level1 | |
| Control (n=12) | 35 | II | Cohabiting | White | University |
| 34 | II | Cohabiting | White | University | |
| 34 | I | Cohabiting | White | A level1 | |
| 33 | I | Cohabiting | Asian | University | |
| 33 | II | Cohabiting | White | University | |
| 33 | I | Cohabiting | White | University | |
| 32 | I | Cohabiting | White | University | |
| 32 | II | Cohabiting | White | A level1 | |
| 31 | II | Cohabiting | White | O level1 | |
| 26 | III | Cohabiting | African—Caribbean | GCSE level1 | |
| 26 | II | Cohabiting | White | University | |
| 26 | II | Cohabiting | White | University |
Testing of the mothers and infants
When the infants were approximately 8 to 10 weeks old, mother and baby came to the research unit for their assessment. The infant was secured in an infant seat at eye level with his/her mother. Behind the seat was a large mirror positioned so that the mother's face and upper torso were reflected towards a remote-control camera situated across the room. In this way the camera, which was operated from the next-door room, captured both the infant and the mother in full-face position as they interacted with each other.
The testing session for mother–infant interaction was divided into three phases, each of which had been explained to the mothers before the session began.
-
(a) Face-to-face play (2 min). During this initial phase mothers engaged in ‘normal’ face-to-face play with their infants. Our instructions were that they should face their infant and, without the aid of toys or other props, play as they normally would. At the end of the 2 min the mothers heard a tap on the wall from the next room, at which point the next phase began.
-
(b) Still-face procedure (90 s). The mothers’ task was to maintain eye contact with their infant, but remain silent and keep a still face, and withhold any other reaction to the infant's behaviour. After a further 90 s another tap on the wall from the adjoining room indicated that they should resume face-to-face play.
-
(c) Face-to-face play (2 min). Again, the mother engaged in face-to-face play for a further 2 min.
Measures
The mother–infant play interactions of the pre- and post-still-face phases of the procedure were rated according to the global ratings for mother–infant interactions devised by Murray et al (Reference Murray, Fiori-Cowley and Hooper1996). This scheme entails 25 ratings on five-point bipolar scales that include the following.
-
(a) Maternal behaviour. We made the a priori decision to focus upon a single composite variable of non-intrusive sensitivity. This combined indices of (non-)intrusiveness (ratings of adult intrusive speech and behaviour) and sensitivity/insensitivity (ratings on warm-positive/hostile, accepting/rejecting, responsive/unresponsive, non-demanding/demanding and sensitive/insensitive).
-
(b) Infant behaviour and affect. We decided a priori to focus on two composite measures derived from the Murray scheme: positive engagement, summing ‘attentive to mother/avoidant’, ‘active communication/no active communication’ and ‘positive vocalisations/silent’; and affect, summing ‘happy/distressed’ and ‘non-fretful/fretful’. In advance we had decided to exclude the ratings for ‘engaged with the environment/self-absorbed’ and ‘lively/inert’ for the reason that these appeared to be addressing somewhat different (and possibly constitutional) infant characteristics.
-
(c) Quality of the interactions. Here we followed the Murray scheme by combining the five interaction scales to form a composite variable of the overall quality of adult–infant interaction. The five scales concern the following aspects of the interaction: smooth and easy/difficult, fun/serious, mutually satisfying/unsatisfying, much engagement/no engagement and excited engagement/quiet engagement.
For the still-face procedure we focused upon infant affect, gaze and availability for positive engagement. Infant affect and gaze are the two kinds of behaviour most commonly rated when evaluating reactions to the still-face procedure (Reference Cohn and TronickCohn & Tronick, 1989; Reference Kogan and CarterKogan & Carter, 1996).
-
(a) In assessing infant affect, we summed the ratings of happy/distressed and non-fretful/fretful from the Murray scheme, as above.
-
(b) In rating gaze, we studied the 90 s of the still-face phase and determined the onset and offset (in ms) of each instance of a look to or away from the mother's face, whether to the room or towards the infant's self. In addition, we noted the onset and offset of any dazed look, which was defined as a glazed expression on the infant's face that could occur as a feature of any look.
-
(c) In evaluating the infant's availability for positive engagement (for which the Murray scheme was not appropriate, given that the mother was immobile), we employed a newly devised scheme in which there was a single judgement made at the conclusion of the episode. We advised raters that availability for positive engagement might be indicated by a combination of the following: open mouth and tonguing movements; positive vocalisations; sustained eye contact; receptivity to mother's bids for engagement; and a quality of charm or irresistibility that draws the mother into interaction. Ratings were made on a five-point scale, thus: 1, virtually no signs of expecting or anticipating positive engagement; 2, very few and/or ambiguous signs of such availability; 3, either repeated, weak signs of positive engagement throughout or initial signs that became less frequent and energetic; 4, clear and persistent signs that the infant was available to engage, which were either moderate or strong but intermittent; and 5, clear and persistent signs that the infant was available to engage in a reciprocal social contact throughout the phase.
Reliability of ratings
Videotape ratings were conducted by a research assistant blind to the hypotheses of the study and the diagnostic groups of the mothers. She had attended a training course for the Murray scheme of rating and had passed reliability tests of her rating skills. A proportion of the videotapes were dual-rated by an independent rater for establishing reliability of all the above maternal and infant ratings (including frequency of looks and length of look) on this sample. The proportion evaluated in this way varied according to the subtlety of the ratings: for most measures there were ten dual-rated videotapes; the exceptions were for the frequency of dazed looks, when all the videotapes were dual-rated to ensure accuracy on this subtle judgement and to achieve consensus for the final ratings, and still-face ratings of infant affect and mean lengths of look to mother, where 30% of the videotapes sufficed. Interrater agreement was estimated with the intraclass correlation coefficient (Reference Shrout and FleissShrout & Fleiss, 1979), which, apart from a value of 0.56 for availability for infant positive engagement during the still face, ranged between 0.68 (for maternal sensitivity/non-intrusiveness) and 0.93 (for infant affect during the still face). For the frequency of dazed looks the coefficient was 0.82.
RESULTS
Baseline period of natural mother—infant interaction
Mothers in the pre-still-face phase
As already described, we did not make specific predictions about this baseline phase of mother–infant interaction and therefore examination of the data is exploratory. It turned out that there was a significant group difference on the measure of maternal non-intrusive sensitivity (mean rank: borderline group, 7.3; control group, 12.6; U=22.5; P<0.05, two-tailed). Inspection of the results revealed that there were only two out of the eight mothers with borderline personality disorder who scored over 25 (out of a possible maximum of 35) on this measure of sensitivity, whereas ten out of twelve control mothers did so. In fact, all but four of the control mothers scored at least 30 out of 35 for sensitivity/non-intrusiveness in this initial phase of mother–infant play.
Infants in the pre-still-face phase
There was not a significant group difference between the infants on the composite measure of positive engagement (attentive to mother v. avoidant; active communication v. no active communication; positive vocalisations v. silent): all but one of the infants of mothers with borderline personality disorder scored at least 10 out of 15 (mean rank 11.9), whereas eight out of twelve infants of control mothers did so (mean rank 9.5; U=36.5; NS). It was notable that the infants of mothers with borderline personality disorder showed non-significantly more (not less) positive engagement than control infants. Ratings of infant affect revealed a similar pattern of results: only one infant of the borderline group scored less than 9 out of 10, and three control infants did so.
Inspection of the looking patterns of the infants revealed that dazed looks were infrequent in both groups. Only one infant of a mother with borderline personality disorder had more than two dazed looks, and two other infants in this group and one infant in the control group had a single dazed look. Finally, ratings of the quality of mother–infant interaction revealed that the two groups were closely similar: all but one of the mother–infant pairs in the borderline group scored 20 or above (out of 25) and six out of twelve of those in the control group did so (mean ranks 10.6 and 10.5, respectively; U=47.5, NS). Therefore, in this respect too and despite the higher scores for insensitive intrusiveness of mothers with borderline personality disorder, there was little to distinguish the groups in quality of interaction.
The still-face phase
Mothers
We checked for indication that the mothers had indeed maintained a relatively still face (and otherwise inexpressive demeanour) during this phase. In general, the mothers sustained a non-responsive stance effectively. The minor exceptions were of three mothers (two in the borderline group, one in the control), each of whom gave a brief look away from their infant, and five mothers (one borderline and four control) who gave one brief smile, in two cases while the infant was looking away.
Infants
Two results were not in keeping with our predictions. First, the two groups of infants were similar in their availability for positive engagement (mean rank of infants: borderline group, 10.1; control group, 10.7; U=45.0; NS); by way of illustration, the mean scores were exactly 2.75 (out of 5) in each group. Second, the infants of mothers with borderline personality disorder were not significantly different in scores for affect, although there was a trend in this respect (mean ranks for affect, with higher scores reflecting more positive and less negative affect overall, were 8.4 for the borderline group and 11.9 for the control group; U=31.5; NS). These two measures suggested that, contrary to our expectation, there were not clear contrasts in the reactions of the two groups of infants to the stress of the still-face challenge.
Yet when it came to examining the infants’ patterns of gaze, there were two results in keeping with our prediction that signs of emotional stress would be more evident in the infants of mothers with borderline personality disorder. First, these infants showed more looks away from the mother (mean rank: borderline group, 14.9; control group, 7.5; U=11.5; P<0.005, one-tailed). Thus, for example, six out of eight of the infants in the borderline group but only one out of twelve of the infants in the control group had more than four looks away. Inspection of the mean lengths of looks to mother in this phase suggested that these tended to be shorter in the case of the infants of mothers with borderline personality disorder, and the two groups were not significantly different in the total time spent looking at the mother (borderline group: mean=41 s, s.d.=20 s; control group: mean=51 s, s.d.=34 s).
Second, infants in the borderline group showed more dazed looks (mean rank: borderline group, 12.9; control group, 8.9; U=28.5; P<0.05, one-tailed), with four out of eight infants in the borderline group but only two out of twelve in the control group showing more than one such look.
The post-still-face phase
Mothers
As predicted, the mothers with borderline personality disorder achieved lower scores for non-intrusive sensitivity than control mothers (mean rank: borderline-group mothers, 6.8; control-group mothers, 13.0; U=18.5; P<0.025, one-tailed). The distribution of raw scores appears in Table 2. Here it can be seen that whereas nine out of the twelve control mothers received scores above 30, indicating their high sensitivity and low intrusiveness, only two of the eight mothers with borderline personality disorder scored so highly, and there were three of these mothers whose scores were strikingly low.
Although logically and empirically it is not possible for a mother to be both intrusive and sensitive, it is possible for a mother to be insensitive but in a non-intrusive (e.g. withdrawn) manner. We had combined the ratings of intrusiveness and insensitivity because our hypotheses and predictions concerned the particular style of insensitivity characteristic of mothers with borderline personality disorder. Having said this, it was possible to compare the groups separately on those items most concerned with sensitivity and those concerned with intrusiveness. The results confirmed that in the post-still-face phase, the mothers with borderline personality disorder were both significantly less sensitive than control mothers (mean rank: borderline group, 7.2; control group, 12.7; U=21.5; P<0.025, one-tailed) and significantly more intrusive (for non-intrusiveness, mean ranks were 7.9 for borderline group and 12.2 for control group; U=27.0; P<0.05, one-tailed).
Infants
Contrary to our first prediction for the post-still-face phase, the infants of mothers with borderline personality disorder did not show less positive engagement in interaction with their mothers (mean rank: borderline group 10.1; control group, 10.8; U=44.5; NS); by way of illustration, mean scores were 10.6 (out of 15) for the borderline group and 11.3 (out of 15) for the control group. On the other hand, when we focused on infant affect, there was a significant group difference in the expected direction, with the infants of mothers with borderline personality disorder showing less positive affect (mean rank: borderline group, 7.7; control group, 12.3; U=26.0; P<0.05, one-tailed). Our third prediction was that, as an index of emotional conflict/disorganisation, the infants of the mothers with borderline personality disorder would show a greater number of dazed looks. The results were in accord with this prediction (mean rank: borderline group, 12.9; control group, 8.9; U=28.5; P<0.05, one-tailed). Thus, for example, five out of eight of the infants in the borderline group showed more than one dazed look, whereas only three out of twelve of the infants in the control group did so.
Mother —infant dyads
Our prediction was that, compared with control mother–infant pairs, the dyads involving mothers with borderline personality disorder would manifest interactions of a less satisfying/engaged quality of interaction (smooth/easy v. avoidant; fun v. serious; mutually satisfying v. unsatisfying; much engagement v. no engagement; excited engagement v. quiet engagement). The distribution of raw scores appears in Fig. 1, where it can be seen that the majority of the control mother–infant pairs are bunched at the high end of the range of scores, whereas this is not the case for the dyads involving a mother with borderline personality disorder (mean rank of mother–infant dyads: borderline group, 7.8; control group, 12.3; U=26.5; P<0.05, one-tailed).
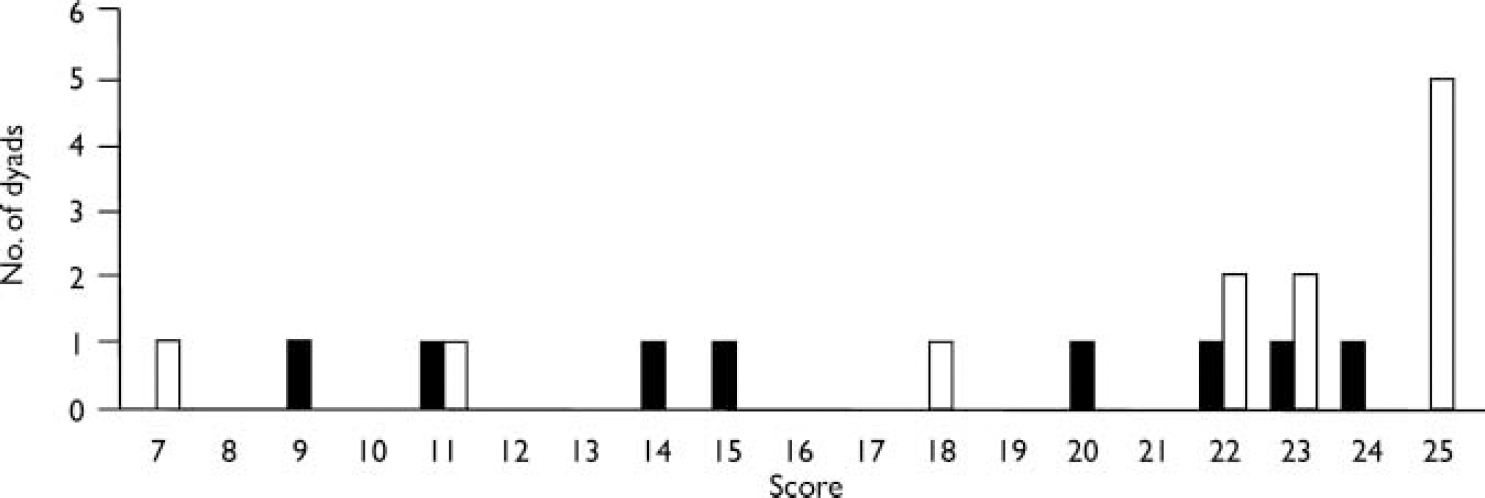
Fig. 1 Post-still-face scores for satisfying/engaged quality of interaction (max. 25): ▪, borderline personality disorder, n=8; □, control, n=12.
Changes in mother—infant status across the procedures
The analyses reported above appear to suggest that one important contrast between the groups might be in the changes in communication across the phases of our procedure. In order to conduct a post hoc exploratory analysis of this, we compared the differences between pre- and post-still-face ratings for each individual mother, infant and/or mother–infant dyad, and considered ratings of affect from this perspective. This approach meant that each dyad provided pre-still-face baseline measures against which the effects of dealing with the stress of the still-face challenge could be evaluated.
There was no indication that the overall degree of maternal sensitivity/intrusiveness changed between the pre- and post-still-face phases of the procedure. For example, the mean scores (out of 35) for non-intrusive sensitivity for the pre- and post-still-face phases were 26.4 and 26.3 for the mothers with borderline personality disorder and 30.2 and 31.3 for the control mothers. This is important because it seems to suggest that any changes in infant state observed in the post-still-face period are unlikely to be due to changes in maternal responsiveness.
When the two groups were compared for the difference between individual infants’ scores for infant positive engagement and affect in the pre- v. post-still-face phases of the procedure (by computing a post-phase minus pre-phase score for each infant), the group difference was shy of significance on a two-tailed test for positive engagement (mean rank: borderline group, 7.9; control group, 12.2; U=27) and significant for affect (mean rank: borderline group, 6.4; control group, 13.2; U=15; P<0.01, two-tailed). The source of the latter result was that the two groups had similar ratings for affect in the pre-still-face phase but the infants of mothers with borderline personality disorder were distinctive in showing a decrement in scores across the still-face and post-still-face periods. Six of the eight infants in the borderline group showed a decline in affect scores from the pre- to the post-still-face phases, but only two out of twelve infants in the control group did so (Fisher's exact test: P=0.02, two-tailed).
Although there was suggestive evidence that the quality of mother–infant interaction also showed a more marked worsening for the dyads with a mother having borderline personality disorder (post-still-face minus pre-still-face difference scores for mean rank: borderline group, 8.4; control group, 11.9; U=31.5; NS), this result did not reach significance.
Additional observations
Finally, we sought for evidence that factors other than that of maternal diagnosis might have been important in determining the pattern of results, even though the groups were not significantly different in these respects (not surprisingly, given the small group sizes). Although there was a slightly higher preponderance of female infants in the control group, inspection of the results revealed that within each group the different genders were fairly evenly distributed across the range of scores on the different measures. The same was true of other factors, such as maternal social class and education (see Table 2).
DISCUSSION
Mothers with borderline personality disorder
The study has yielded evidence that mothers with borderline personality disorder are prone to relate to their infants in a style that may be characterised as intrusively insensitive. In the post-still-face period, when both mother and infant were recovering from the stress of the mother maintaining an unresponsive stance, the majority (nine out of twelve) of the control mothers scored above 30 (out of 35) for non-intrusive sensitivity, but only a small minority of mothers with borderline personality disorder (two out of eight) did so. As it turned out, a similar style of maternal relatedness was also apparent in the initial period of free play, before the still-face phase began.
Infants’ relatedness
There were also group differences in the behaviour of infants in response to the still-face procedure. The infants of the mothers with borderline personality disorder had been indistinguishable from the control infants in the baseline period, and during the still-face episode itself (contrary to our predictions) they were neither markedly distressed nor low in availability for positive engagement – yet their greater number of looks away from the mother and their significantly greater number of dazed looks appeared to indicate a different strategy of dealing with interpersonal stress than occurred with the control infants. Each of these patterns of gaze had been predicted on the basis of previous studies, suggesting that gaze aversion and dazed looks are potential indicators of emotional conflict or disturbance in mother–infant interactions; for example, dazed looks were rated because of prima facie similarities with the states of infant ‘freezing’ observed in disorganised infant attachment patterns. It was also notable that the group difference was in the pattern rather than the duration of looks away, with the infants of mothers with borderline personality disorder tending to give brief looks to their mothers and then looking away. One interpretation of these findings is that whereas infants who have experienced a contingent and sensitive interactive partner are able to manage the forced disruption by waiting for the expected available person to return, such self-regulation is more problematic for infants who have been exposed to intrusive or otherwise insensitive interactions.
These indicators of group differences among the infants were reinforced when it came to the results from the final phase of the procedure, when mothers resumed play interaction after the still-face period was over. Although the infants in the borderline group continued to have a degree of positive engagement, they were depressed in affect and continued to show more dazed looks. Also as predicted, the quality of the interaction between the mothers with borderline personality disorder and their babies was less satisfying than in the case of control mother–infant dyads. Across the phases of the procedure, the infants in the borderline group showed a more marked decrement in scores for overall affect.
Methodological limitations
Given the thoroughness of the diagnostic screening procedures, the principal methodological limitation of the study arises from the small sample sizes – although, to our knowledge, this group of mothers with borderline personality disorder is the largest studied so far with their infants. One reason, of course, is the problem of identifying and recruiting mothers with borderline personality disorder who have very young infants. As in a previous study of small groups of patients with borderline personality disorder or dysthymia (Reference Hobson, Patrick and ValentineHobson et al, 1998), our limited number of coherent and theoretically grounded a priori predictions proved to be testable even on samples of modest size. Despite there being a minority of cases where mothers with borderline personality disorder were relatively sensitive towards their babies, the within-group consistency and between-group contrasts were such that there were significant group differences.
The most important issue concerns potentially confounding variables, and the degree to which the findings may be taken as being representative of the diagnostic group under study. With regard to the former issue, one needs to examine whether it is plausible that the present set of group differences, largely predicted on the basis of psychopathological considerations, might be attributable to factors other than those of maternal diagnosis. It is evident from the almost complete data available (Table 2) that the two groups were broadly similar in educational status (all had completed school examinations at CSE level or above and over half of each group had attended university) and the majority of each group were White. Of those (the large majority) with recorded data, all but two of the mothers were cohabiting and all but one in each group came from social classes I and II. Moreover, inspection of the results did not suggest that demographic factors were consistently associated with lower or higher scores on our various measures (e.g. maternal relatedness; see Table 2). Therefore, although the groups were not tightly matched, their comparability renders it unlikely that the observed group differences could be attributed to demographic factors.
With regard to the representativeness of the results, how far can we be confident that the patterns of maternal relatedness observed are indeed characteristic of mothers with this diagnosis? There are two aspects to this question. The first is whether the present sample might represent only a special subgroup of mothers and infants, for example by virtue of recruitment procedures that biased towards higher social classes. This kind of issue can be resolved only by future studies, but the results do conform with other evidence on the nature of borderline psychopathology. The second, complementary question concerns the specificity of the observed group differences to the particular diagnostic group under study. Here, further research is needed. As noted in the introduction, intrusive insensitivity is not restricted to mothers of a particular diagnostic group, nor indeed to mothers with a psychiatric diagnosis. It remains to be established whether, in quality or degree, mothers with borderline personality disorder are distinctive in the manner of their intrusive insensitivity and whether any impact that this may have on infant development is special in kind. It is also to be determined whether the kinds of maternal relatedness and infant response observed in this study might be exacerbated or mitigated by a range of potentially interacting factors such as life adversity, the presence of a supportive spouse, and so on.
Sources of individual differences
It remains a challenge to determine how far any individual differences among mother–infant dyads are the result of characteristics of the mothers, characteristics of the infants or combinations of the two. In a cross-sectional study such as this, it is rarely possible to establish whether constitutional factors in the infants are eliciting particular forms of maternal relatedness or whether the mothers’ styles of relating are prompting specific patterns of response in the infants. Unusually, in the present instance there is suggestive evidence that maternal factors are probably most important in shaping the qualities of infant response.
There are three lines of evidence in this regard. First, there is clinical and quasi-experimental evidence that women with borderline personality disorder are prone to intense, disturbed and often insensitive relations with other people, and it is in accord with such observations that we recorded intrusive insensitivity in the context of mother–infant relations. Similar styles of interaction were observed when we videotaped mothers with borderline personality disorder (including some of the present sample) relating to their infants at 12 months of age (paper in preparation). Second, evidence from the pre-still-face phase of the present study suggested that although the mothers with borderline personality disorder were behaving insensitively, their infants showed little evidence of being abnormal in their responsiveness and positive engagement, so it seems unlikely that the infants were eliciting the maternal behaviour. Third, group differences in the infants became manifest in the context of the stress of the still-face procedure and its aftermath. The signs were not in the infants’ availability for positive engagement, but rather in their looks away from the mother, in their dazed looks, in their increasingly negative affect and in the less satisfying re-engagement with the mother. Given the meaning of such kinds of behaviour in other infant studies, one reasonable interpretation is that they reflected decompensation in the infants of the borderline group because they found it more difficult to turn to and ‘use’ their mothers to maintain their equilibrium during and after the still-face challenge. However, it cannot be ruled out that these signs indicated infant constitutional factors, and that the mothers’ behaviour had been shaped over previous interactions with their infants.
Whatever the case in this respect, the evidence is that the intrusive insensitivity of most of the mothers with borderline personality disorder was associated with distinctive patterns of infant response to the special kind of interpersonal stress constituted by the still-face challenge. These patterns not only conformed to the kinds of response previously observed in infants of insensitive mothers, but they also carried over into the period that succeeded the still-face encounter.
CONCLUSIONS
The present study has yielded evidence that, as a group, mothers with borderline personality disorder tend to be intrusively insensitive with their young infants. Moreover, even as early as 2 months of age, there are signs that the infants of such mothers manifest atypical social–emotional responses to interpersonal stress. The evidence is suggestive but not conclusive that these infant characteristics probably reflect the impact of maternal relatedness, and it is possible that they represent early signs of potentially dysfunctional infant self-regulation. Whether they are also harbingers of subsequent developmental psychopathology is an issue that deserves serious attention.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Mothers with borderline personality disorder tend to relate to their 2-month-old infants in a way that might be called ‘intrusively insensitive’.
-
▪ There is evidence that, in the face of interpersonal stress (the ‘still-face challenge’), infants of these mothers tend to show more looks away and more dazed looks.
-
▪ Mother—infant interactions after the still-face challenge suggested that the dyads with a mother having borderline personality disorder were more unsettled than control dyads, and the infants showed continuing effects of this stressor.
LIMITATIONS
-
▪ The sample sizes were small.
-
▪ The specificity of the infant responses to maternal psychopathology and/or styles of relatedness, and the contribution of associated variables, are still to be established.
-
▪ It remains to evaluate the bearing of additional factors such as adversity and social support on the interactions between mothers with borderline personality disorder and their infants.
Acknowledgements
This study was supported by Fellowships from the US National Institute for Mental Health to Dr Crandell and the Wellcome Foundation to Dr Patrick, and funding from the Joseph Levy Charitable Foundation and the Charles Hayward Charitable Trust. We are very grateful to the mothers and infants who took part. We are deeply indebted to the contributions of Rosa Garcia-Perez and Tony Lee, to Lynne Murray for giving so generously of her time and advice, and to the late Channi Kumar for help in locating participants. We also thank Leezah Herzmann for her help with aspects of the study. A special thank you to Howard Steele for thoughtful advice and suggestions.






eLetters
No eLetters have been published for this article.