Introduction
Suicide is a global mental health problem, with 800 000 incidents a year.1 The World Health Organization (WHO) made suicide prevention a global imperative and urged interventions at the individual, relational and societal level. A plethora of risk and protective factors are known to delineate the context in which suicidal ideation and behaviour in women and men develop, and account for differences in prevalence between groups of individuals and communities.1–Reference Oyesanya, Lopez-Morinigo and Dutta6 Less studied are country-level factors that can provide insights and new ideas regarding the management of suicide. This study investigated whether the vulnerability paradox, the tendency for vulnerability to predict greater disorder risk at the individual level but less risk at the country level, contributes to explaining differences in suicide prevalence across 100 countries.
A standard measure of the vulnerability or risk attributable to different countries is updated annually and freely available (see, for instance, Welle and BirkmannReference Welle and Birkmann7). Each country receives an overall score based on publicly available metrics such as income equality, good governance, access to professional healthcare providers, public and private health expenditure, life expectancy at birth, literacy and access to clean water and nutrition. The vulnerability index was used in recent cross-national comparison studies reporting that, contrary to expectations based on studies of individual risk, lower vulnerability levels at the country level are accompanied by a higher prevalence of mental health problems, especially when populations experience a higher exposure to traumatic events. This counterintuitive ‘vulnerability paradox’ was first identified for post-traumatic stress disorder (PTSD) in 24 countries.Reference Dückers, Alisic and Brewin8 Similar findings have been reported for substance and anxiety disorders and, most markedly, for mood disorders in 17 countries.Reference Dückers and Brewin9 The paradox in PTSD was shown to apply equally to women and men in a sample of 11 countries.Reference Dückers and Olff10
Concerns about the vulnerability paradox's validit
Although the report of a vulnerability paradox has sometimes been met with a sceptical response,Reference Vermetten, Stein and McFarlane11 McNally has commented that such scepticism is likely an example of the ‘ecological fallacy’. This arises when ‘one assumes that associations between variables at the ecological (group or aggregate) level necessarily apply to associations between these variables at the level of the individual’ (p. 33).Reference McNally12 Moreover, there are already reasons to believe the vulnerability paradox could apply to suicide. When countries are clustered according to World Bank income categories (high income, upper-middle income, lower-middle income and low income), suicide rates are higher in countries with higher income levels.1 These data contrast with within-country studies of economic factors that demonstrate recessions, and the associated increase in unemployment and indebtedness, are linked to a rise in suicide rates, particularly in high-income countries such as European states and the USA.Reference Oyesanya, Lopez-Morinigo and Dutta6
Although the studies above support the notion of a vulnerability paradox in the cross-national prevalence of mental health problems, they all suffer from the same limitations, namely a relatively small sample size and a reliance on the instruments and methodological heritage of the WHO World Mental Health Survey Initiative (i.e. clinical interviews with thousands of adults from representative household samples, using the Composite International Diagnostic Interview).Reference Kessler and Üstün13, Reference Kessler and Üstün14 They were not designed ‘to optimize examination of the reasons for cross-national differences’, but ‘to search for patterns of central tendency and to highlight the most stable of such patterns across countries’ (Kessler et al: pp. 33).Reference Kessler, Heeringa, Pennell, Sampson, Zaslavsky, Scott, de Jonge, Stein and Kessler15 Additionally, we were not able to ascertain whether the findings were attributable to a simpler metric such as broad differences in average income levels. In the current study focusing on explaining cross-national differences in suicide rates, we aimed to verify the existence of the vulnerability paradox, using data from a substantially larger country sample and coming from an entirely different source.
Method
Data sources
In 2014, the WHO published the report Preventing Suicide: A Global Imperative.1 This report contains the estimated age-standardised suicide rates of women and men (per 100 000 people) in 2012 in 172 countries that were used as a primary data source for the current study. In the report, four data quality levels are distinguished: level 1, comprehensive vital registration with at least 5 years of data; level 2, vital registration with low coverage, a high proportion of indeterminate causes or no recent results; level 3, sample registration of national population; and level 4, no vital registration. Of the countries for which estimates were made, 60 have good-quality vital registration data (level 1) that can be used directly to estimate suicide rates. The estimated suicide rates in the other 112 countries are based on modelling methods (levels 2, 3 and 4). More detailed information on the four data quality levels is not given in the report. The WHO report emphasises that the problem of poor-quality mortality data is not unique to suicide, yet given the particular sensitivity of suicide, religious and social prohibitions and the illegal status of suicidal behaviour in some countries, underreporting and misclassification are considered more likely problems for suicide prevalence estimates than for most other death causes. Suicide registration is a complicated, multilevel procedure that includes medical and legal concerns and involves multiple responsible authorities that can differ between countries. The report reminds its readers that the wide range in estimated suicide rates reported for different countries might be an artefact of different reporting and recording practices. Nevertheless, they are the best empirical material available. Moreover, regional differences have persisted despite decades of work on improving the accuracy of country-specific mortality data. The possibility that a considerable part of these observed differences are, in fact, real differences must also be considered.1 In view of these potential data limitations, we controlled for data quality in our study, using only suicide data from countries meeting data quality levels 1 and 2, and omitting data from countries with sample registration or without vital registration.
Country vulnerability data were taken from the World Risk Report of 2016.Reference Welle and Birkmann16 The vulnerability of 171 countries was summarised using 23 indicators, divided into three components and measured using worldwide and publicly accessible data. ‘Susceptibility’ describes a country's structural characteristics and conditions that can sustain harm; for example, indicators of susceptibility involve malnutrition, access to sanitation, income equality (Gini index) and gross domestic product per capita. ‘Lack of coping capacities’ refers to the inability of a country to minimise negative effects of events and includes indicators such as number of physicians and hospital beds per 10 000 inhabitants and level of public sector corruption. ‘Lack of adaptive capacities’ refers to conditions that fail to support long-term structural change. Example indicators include the adult literacy rate, combined gross school enrolment and public and private health expenditure. Country vulnerability scores are calculated on a scale, ranging theoretically from 0 (minimum) to 100 (maximum), and can be interpreted as percentage values. The five least vulnerable countries in 2016 were Switzerland (24.79), Austria (24.93), Norway (25.55), Germany (25.87) and Belgium (26.28). The five most vulnerable countries were Haiti (71.85), Afghanistan (72.12), Chad (72.86), Eritrea (74.23) and Central African Republic (74.80). The vulnerability index has been confirmed to be a stable measure over years in the earlier studies.Reference Dückers, Alisic and Brewin8, Reference Dückers and Olff10 The correlation between the vulnerability scores in the 2016 World Risk Report and the 2013 scores used in the PTSD study, for instance, is almost perfect (r = 0.991, N = 171). Background information on the vulnerability index can be found in the World Risk Report.Reference Welle and Birkmann16
As mentioned earlier, we also aimed to examine the explanatory strength of the World Bank income groups in this study in relation to the vulnerability index. The World Bank income division entails a rough wealth rating, which is also integrated in the vulnerability score together with the index's 22 other indicators because economic wealth is a relevant dimension of vulnerability.Reference Dückers, Frerks and Birkmann17 In this study, we planned to use vulnerability and income separately and together as determinants. We categorised countries using the World Bank list of economies of December 2016. All World Bank member countries (189) and other economies with populations of >30 000 are divided among income groups according to 2015 gross national income per capita, calculated using the World Bank Atlas method. The groups are low income (≤$1025), lower-middle income ($1026–4035), upper-middle income ($4036–12 475) and high income (≥$12 476).18
Analysis
Because suicide data commonly do not follow the shape of a normal distribution, researchers apply count models like Poisson. However, the assumption behind the Poisson distribution that the mean and variance are equal is not correct for our sample. Instead of using Poisson regression, we conducted negative binomial regression analyses to resolve the problem of overdispersion. The analyses were performed in multiple steps in Stata, version 13 for Windows. A likelihood ratio test was used to compare the goodness of fit of each model with an earlier model. In model 1, we tested whether the prevalence of suicide in men is higher than in women. In model 2, country vulnerability was added to determine the presence of the paradox, which would be reflected in negative correlation coefficients between suicide and vulnerability and in negative regression coefficients: lower suicide is accompanied by higher country vulnerability. Model 3 included an interaction term to verify whether the effect of vulnerability is moderated by gender. From these three models we selected the one with the best goodness of fit, adding the World Bank income categories in model 4 and, together with suicide data quality, in model 5.
Ethical approval
Ethical approval was not required for this study, which was based on aggregated country-level data extracted from freely accessible public reports.
Data availability
All primary data sources utilised in this study are publicly accessible. The data-set used for the analysis is available via (https://www.synapse.org/#!Synapse:syn18373562/wiki/588771).
Results
A data-set was created with complete information from 100 countries on the suicide prevalence in women and men, the vulnerability score, World Bank income categories (high: 48 countries, upper-middle: 37 countries, lower-middle: 14 countries, low: 1 country), and suicide data quality (level 1: 60 countries, level 2: 40 countries) (see https://www.synapse.org/#!Synapse:syn18373562/wiki/588771). The data on national suicide rates in women and men in 100 countries have an asymmetric, right-skewed distribution. The observation count decreases gradually from low to high suicide prevalence. Over 60% of national suicide prevalence rates in men are ≥10 per 100 000 inhabitants, whereas 95% of national suicide prevalence rates in women are <10 per 100 000 inhabitants.
After having explored the data for outliers (values lower than the first quartile or exceeding the third quartile by >1.5 times the interquartile range), we excluded four national records in which women had a suicide prevalence higher than 11.8 (per 100 000): Guyana, South Korea, Sri Lanka and Surinam. Similarly, four records in which male suicide was higher than 43.2 (per 100 000) were excluded: Guyana, Lithuania, Sri Lanka and Surinam. Distributional information for country vulnerability and suicide and the correlations between these variables are shown in Table 1. The average suicide prevalence in men in this country sample was approximately four times higher than in women. Country vulnerability and suicide were correlated significantly and negatively in women and men with a medium effect size (Spearman's rho: −0.32 and −0.38, respectively). The correlation between suicide in women and men across countries was significant and strong (Spearman's rho: 0.81).
Table 1 Distributional information and correlations

Source: vulnerability score: Welle and BirkmannReference Welle and Birkmann16; suicide prevalence: World Health Organization report, 2014.1
N, number of countries; Min-Max, minimum and maximum value; IQR, interquartile range.
*P < 0.05.
** P < 0.01.
*** P < 0.001.
We conducted negative binomial regression analyses to determine the effect of different predictor variables on suicide prevalence (women and men in 96 countries; N = 192). In model 1, the suicide prevalence in men was significantly higher than in women (B = 1.30; P < 0.001). In model 2, this gender effect was maintained (B = 1.29; P < 0.001) after adding country vulnerability (B = −0.02; P < 0.001). The explained variance increased from 10 to 12%. The improvement in log-likelihood between model 1 and model 2 was significant (P < 0.001). The interaction term in model 3 was not significant, did not enhance model fit and did not significantly explain additional variance. We also tested the three models using the data-set including the eight outlier records and found similar effects.
In model 4, the World Bank income categories were added to model 2, the model with gender and vulnerability, which resulted in an improvement (Table 2). The suicide prevalence in lower-income countries was lower compared with high-income groups. Vulnerability was correlated with income; when vulnerability in model 2 was replaced by income, this did not improve the goodness of fit compared with model 1 with gender alone (P > 0.05). In model 5, we found a similar effect after adding data quality: suicide prevalence is lower in countries with a lower suicide data quality, which were more vulnerable countries, grouped in lower World Bank income categories. We further examined the influence of data quality by checking whether the results of model 2 and model 4 were different when the two models were tested using the suicide data from the 58 countries with the highest data quality level (level 1). In both models the results were similar with higher levels of explained variance (model 2, with gender and vulnerability: pseudo R 2 = 0.15; model 4, with gender, vulnerability and income: pseudo R 2 = 0.16).
Table 2 Summary of negative binomial regression analysis for variables predicting suicide prevalence with control variables

N = 192 (women and men in 96 countries).
a. /Lnapha is the estimate of the log of the dispersion parameter alpha. Alpha can be obtained by exponentiating /Lnalpha.
*P < 0.05.
** P < 0.01.
*** P < 0.001.
Table 3 contains the results of a sensitivity analysis conducted within those World Bank income category country groups with sufficient data. Because Haiti was the only low-income country with available data, the category of low income could not be included in the sensitivity analysis. In each of the high (P < 0.01), upper-middle (P < 0.001) and lower-middle (P > 0.05) income countries, model 2 resulted in a negative vulnerability coefficient with about 13% of the variance attributable to gender and vulnerability (pseudo R 2 = 0.12–0.13).
Table 3 Summary of negative binomial regression analysis for variables predicting suicide prevalence in World Bank income country groups

N = 190 (women and men in 95 countries; Haiti, a low-income country, was not included).
a. /Lnapha is the estimate of the log of the dispersion parameter alpha. Alpha can be obtained by exponentiating /Lnalpha.
*P < 0.05.
** P < 0.01.
*** P < 0.001.
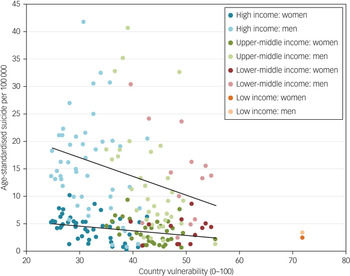
Figure 1 illustrates the vulnerability paradox in suicide in women and men as identified in model 2. The slope in men appears to be slightly steeper; however, in model 3 we could not statistically confirm the modification of vulnerability by gender. The variation in suicide between countries is higher in men than in women. Besides a darker colour scheme for women compared with men, the colours of the dots represent the World Bank categories (model 4) across the country vulnerability continuum.

Fig. 1 Association between suicide prevalence in women and men and country vulnerability across World Bank income groups. Shown here is the association between suicide rates (per 100 000) and country vulnerability in 96 countries. The upper and lower lines represent the vulnerability paradox in men and women, respectively. In both gender groups an increase in vulnerability is accompanied by lower suicide rates. From left to right, different colours are used to distinguish the World Bank income categories across the vulnerability continuum. High-income countries are displayed in blue (47 countries), upper-middle income in green (35 countries), lower-middle income in red (13 countries) and low income (1 country) in orange. The darker colour scheme is used for women and the lighter colour scheme is used for men.
Discussion
In this study we discovered that the vulnerability paradox in suicide exists in both women and men, and across and within the World Bank income groups. The results corroborate the findings from the previous studies which, were conducted in smaller samples and using a different data source. The association we found between country vulnerability and suicide in 96 countries (Spearman's rho: −0.32 to −0.38; Table 1) was not as strong as the correlation between vulnerability and PTSD in 24 countries (r = −0.49) and any mood disorder in 17 countries (r = −0.56), but larger than the correlations between vulnerability and any anxiety disorder (r = −0.22) in 16 countries and any substance disorder (r = −0.13) in 17 countries.Reference Dückers, Alisic and Brewin8, Reference Dückers and Brewin9 Consequently, we consider it less likely that the earlier findings, despite being consistent, are an artefact of the classification schemes and measures used in the epidemiological surveys. Again, mental health problems seem to be more prevalent in less vulnerable countries, even when subgroups based on gender and World Bank income categories are analysed.
The results contribute to emerging literature focusing on risk factors, exceeding the level of the individual. Recent studies ascertained the effect of risk factors such as living in a less green environment, single and repeat exposure to natural and human-made disasters and income equality on suicide in populations.Reference Helbich, De Beurs, Kwan, O'Connor and Groenewegen3, Reference Lorant, de Gelder, Kapadia, Borrell, Kalediene and Kovács19, Reference Reifels, Spittal, Dückers, Mills and Pirkis20 The review by Oyesanya et al suggests that economic changes, recessions specifically, create a risk for suicide, particularly in high-income countries.Reference Oyesanya, Lopez-Morinigo and Dutta6 What our analysis adds is the confirmation that living in a less vulnerable, high-income country is a risk factor itself. This conclusion is supported by findings from other recent studies, comparing mental health problems in different World Bank income groups, assessing the prevalence of generalised anxiety disorder in 26 countries and adult attention-deficit hyperactivity disorder in 20 countries.Reference Ruscio, Hallion, Lim, Aguilar-Gaxiola, Al-Hamzawi and Alonso21, Reference Fayyad, Sampson, Hwang, Adamowski, Aguilar-Gaxiola and Al-Hamzawi22
Explaining the vulnerability paradox
Confirming an inverse association between country vulnerability and mental health is one thing, but explaining it is another. Some of the explanations described in the initial paradox paper identified cultural factors that might increase the risk associated with living in a less vulnerable country.Reference Dückers, Alisic and Brewin8 In terms of Hofstede's classification of cultural dimensions,Reference Hofstede23 less vulnerable, more affluent countries are characterised by higher levels of individualism, a more equal distribution of power and greater indulgence within society.Reference Dückers, Frerks and Birkmann17 Consequently it was hypothesised that members of populations with higher levels of individualism, more equal distribution of power and less restraint in pursuing basic human desires, engender a greater sensitivity to social failure and the hampered realisation of aspirations. The blocking of personal aspirations and goals might be coupled, furthermore, with lower levels of protective social support and less hindrance by stigma when it comes to expressing emotions, discussing personal problems including mental health, and expressing a need for help.Reference Dückers, Alisic and Brewin8
Another possible explanation given was that variation in the availability and accessibility of professional mental health services between countries might affect the likelihood of being diagnosed with mental disorders. Moreover, it is conceivable that the lower availability of institutional and professional health capacities and systems in more vulnerable countries is accompanied, or even compensated for, by alternative supportive aspects of social capital, such as community engagement and social support within people's personal networks.Reference Dückers, Witteveen, Bisson and Olff24
Whether these explanations are more or less applicable to suicide remains to be determined. However, a study by Webster Rudmin et al, based on 33 countries, found that higher levels of individualism, a more equal distribution of power, less uncertainty avoidance and low masculinity were accompanied by more suicide.Reference Webster Rudmin, Ferrada-Noli and Skolbekken25 We interpret these results as a confirmation of the relevance of cultural characteristics in the cross-national analysis of suicide rates. It is arguably a major lacuna in contemporary knowledge that the interaction of cultural factors with better-established risk and protective factors remains poorly understood. In the international strategy and recommendations to address suicide globally put forward by the WHO, for instance, cultural aspects are mentioned several times but – apart from religious, legal and social prohibitions – without a detailed clarification of what exactly they are, why they are important, and how they can be influenced.1
What the explanations have in common is that they reflect interpretations of associations between a myriad of country-level factors based on cross-sectional data-sets. Exploration or testing of associations between mental health and other factors – unrelated to the cultural and socioeconomic country factors already discussed – will produce different explanations. We want to encourage researchers to unravel causal mechanisms. We did not add country characteristics besides the vulnerability index, income and data quality because these factors were linked to our replication objective. In the light of other theories or research questions, it remains meaningful to keep exploring the relevance of the index and its distinct constitutive elements, as well as of specific country-level characteristics left unaccounted for. This is necessary to better understand cross-national differences in mental health independently of the cultural and socioeconomic factors addressed in this study, through the lens of vulnerability.
Limitations
The cross-national analysis of PTSD and other mental disorders considered the exposure to traumatic events in the general adult population.Reference Dückers, Alisic and Brewin8, Reference Dückers and Brewin9 It was possible to test several models with trauma exposure and country vulnerability as single predictors, in combination and with an interaction term. Unfortunately, trauma exposure data were unavailable for the countries in the current study. We consider this a limitation because trauma exposure proved to be an important predictor of disorder prevalence at the country level, independently explaining even more variance in mental problems than country vulnerability – with the latter amplifying the effect of trauma exposure on PTSD.Reference Dückers, Alisic and Brewin8
The most important limitations of this study have to do with the suicide data. The analysis showed that prevalence is influenced by data quality, which is linked to vulnerability and income. We restricted ourselves to the quality levels 1 and 2, but this does not ensure that the complicated registration process is free of flaws, including misclassifications.1
Another fundamental limitation is that we are still not in the position to conduct multilevel analyses to examine the mental health of populations using large-scale data-sets that contain information on individuals, the demographic groups they belong to, nested in countries and larger regions, over a longer time period.
However, what the current study demonstrates is that cultural and socioeconomic country-level factors matter. Not only do public health problems differ between countries, so do the risk and protective factors and the capacity to adequately address them. Global mental health strategies need to be tailored to individual country contexts as they provide the background where mental problems develop and they may require different solutions. Perhaps different socioeconomic country groups can learn from each other's strategies to identify and utilise protective factors, particularly given the lower likelihood of developing mental health problems in more vulnerable countries. We only are at the beginning of understanding cross-national differences in mental health, their explanations and relation to explanatory factors and mechanisms, and their implications for policy-makers and practitioners.






eLetters
No eLetters have been published for this article.