Introduction
Research suggests that large numbers of individuals experiencing mental health difficulties meet criteria for multiple diagnoses, and thus are presenting with co-morbid difficulties (Kessler et al., Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2005a; Kessler et al., Reference Kessler, Chiu, Demler and Walters2005b; Nock et al., Reference Nock, Hwang, Sampson and Kessler2010). This has been found to be true not only for clients presenting with mood and anxiety difficulties, but also with personality difficulties (Lenzenweger et al., Reference Lenzenweger, Lane, Loranger and Kessler2007) and psychotic presentations (DeVylder et al., Reference DeVylder, Burnette and Yang2014; Kiran and Chaudhury, Reference Kiran and Chaudhury2016). Thus, it is important for mental health practitioners to be able to work effectively with complex co-morbidities, and there is a need for research which highlights how evidence-based approaches can be implemented with this population.
Cognitive behavioural therapy (CBT) remains one of the most well-evidenced forms of psychological intervention, with a well-established evidence base showing it to be effective when working with varied presentations, including anxiety, mood and psychotic difficulties (Hofmann et al., Reference Hofmann, Asnaani, Vonk, Sawyer and Fang2012; Jauhar et al., Reference Jauhar, McKenna, Radua, Fung, Salvador and Laws2014; Trauer et al., Reference Trauer, Qian, Doyle, Rajaratnam and Cunnington2015). As such, it is critical for CBT to be appropriately utilised in mental health services, including when working with more complex, co-morbid presentations.
One way CBT may be useful when working with co-morbidity is to utilise transdiagnostic CBT approaches, for which there is a rapidly developing evidence base attesting to their effectiveness (Pearl and Norton, Reference Pearl and Norton2017). Alternatively, CBT interventions could be utilised to target a particular aspect of an individual’s presentation, drawing on diagnosis-specific CBT interventions where appropriate. This approach may be especially appropriate where a specific aspect of an individual’s presentation is particularly debilitating or preventing engagement with their treatment more generally. There is a well-established evidence base attesting to the effectiveness of diagnosis-specific CBT interventions, thus utilising a targeted, structured CBT intervention offers one way diagnosis-specific CBT can be effectively utilised when working with complex co-morbidities.
Research has shown that CBT can result in symptom reduction when used in a targeted manner in the context of a wider, complex case (Dudley et al., Reference Dudley, Dixon and Turkington2005; Kayrouz and Vrklevski, Reference Kayrouz and Vrklevski2015; Williams et al., Reference Williams, Capozzoli, Buckner and Yusko2015). However, more research replicating these sorts of findings, particularly in real-world settings, would be useful. In particular, research exploring some of the challenges involved in this targeted CBT approach is needed. When working with these complex, multi-faceted presentations, it seems likely that an individual’s co-morbid difficulties may impact on the therapeutic process and outcomes of the targeted CBT intervention. Research exploring this, particularly through drawing on specific clinical examples, would add to the existing literature and is likely to be of use to practitioners. It is this research gap that this study is looking to fill.
Aim
This case study describes the clinical treatment of a man presenting with a specific phobia of stairs alongside long-standing difficulties of delusions and auditory hallucinations. This study uses a single-case A-B design and seeks to contribute to the evidence base by detailing an example of how CBT can be used in a targeted manner to tackle a specific set of symptoms within a wider presentation of serious and co-morbid mental health difficulties.
Presenting problem
Case introduction
This case study outlines a piece of CBT with Mr A (anonymised), a White British man in his 50s. Mr A lived alone in a ground floor flat, did not work and was moderately socially isolated. Mr A had been referred to the Community Mental Health Team (CMHT) in his early 20s, following experiences of delusions and auditory hallucinations. At that time, he had received a diagnosis of schizophrenia. These psychotic experiences had been ongoing since he received this diagnosis, and had resulted in a number of admissions to in-patient units. Mr A also met criteria for a specific phobia of stairs. The current clinical work began after Mr A was referred by his CMHT care co-ordinator to the Complex Psychological Interventions team for support with the phobia. At the time of treatment, Mr A was still experiencing regular auditory hallucinations and was being prescribed an anti-psychotic medication. He was receiving ongoing support from the CMHT multi-disciplinary team to manage these difficulties in the form of monthly visits from his care co-ordinator.
Assessment
At assessment, Mr A reported experiencing high levels of anxiety in relation to stairs for 10 years. He reported experiencing anxiety both in relation to climbing and descending stairs, and at assessment could at most climb one stair if necessary. Mr A reported that this was significantly impacting his daily functioning, limiting his ability to do things he used to enjoy (such as go to coffee shops and museums, or go on holiday) and restricting his routine to a point where his social contact was significantly limited.
Mr A reported that these difficulties started following an incident where he fell down a flight of stairs 10 years ago. He reported that he sustained no significant injuries but became increasingly fixated on what could have happened from this fall (particularly, that he could have become permanently disabled). As such, Mr A reported experiencing increasingly high levels of fear when he encountered stairs and began avoiding using stairs as often as possible.
In assessment, Mr A identified a number of key cognitions triggered when encountering stairs, including: ‘I will fall and die if I go on the stairs’, ‘I will fall and become seriously disabled if I go on the stairs’ and ‘If I am disabled, I won’t be able to cope’. He also reported experiencing physical sensations, such as ‘wobbly legs’, ‘racing heart’ and ‘breathing changes’. Mr A reported several behaviours which he used to prevent the above feared responses occurring, including: avoiding stairs, limiting his routine to previously used routes, and holding on to something when using stairs.
Within assessment, some of the wider mental health difficulties that Mr A was experiencing were discussed, including his ongoing auditory hallucinations and low mood related in part to social isolation. However, it was collaboratively agreed to target our work at the specific phobia. As such, the later formulation and intervention work focused exclusively on Mr A’s phobic difficulties.
Goals
During assessment, Mr A highlighted his primary concern as the impact his fear of stairs was having on limiting his ability to engage with things that were important to him. Based on this discussion, three therapeutic goals for treatment were collaboratively set:
(1) For Mr A to be able to go up and down seven stairs by the end of treatment.
(2) For Mr A to have increased his confidence in his ability to cope with new stairs to 50% by the end of treatment.
(3) For Mr A to have restarted activities his phobia currently prevented, specifically going to coffee shops and the museum, by the end of treatment.
Design
This case employed a single-case A-B design (n = 1). The outcome measures were collected at three time points at baseline (A) and session by session during the intervention period (B).
Outcome measures
The primary outcome measure used was the Severity Measure for Specific Phobia – Adult (SMSP-A) (Craske et al., Reference Craske, Wittchen, Bogels, Stein, Andrews and Lebeu2013). This is a 10-item measure that assesses the severity of specific phobia in adults over the age of 18. Total score was used to represent severity of Mr A’s phobia. This is an emerging measure, and therefore there are limited data regarding its psychometric properties. However, it has been used in a number of studies, where it was found to be a useful measure of symptoms (LeBouthillier and Assmundson, Reference LeBouthillier and Asmundson2017). The measure was collected on a weekly basis. Mr A was encouraged to complete this measure at home at a regular time-point in order to reduce possible measurement confounding variables and to prevent the therapist’s presence biasing findings.
At the time of the case study, no validated measures existed which were applicable to this form of specific phobia (as opposed to spider phobia or agoraphobia), created for adults and were felt to be therapeutically useful. Whilst the Fear Questionnaire was considered (Marks and Mathews, Reference Marks and Mathews1979), this questionnaire is very brief and does not generate detailed information regarding phobia severity. Thus, it was felt that the SMSP-A was the best available measure at the time to track change, with the detailed nature of the measure allowing Mr A and the therapist to explore different facets of the phobia over time.
Singular items on the SMSP-A, items 3 and 6, were used to measure regularity of threat-related cognitions and avoidance of the phobic object. On these items, the client is asked to rate how regularly they have ‘had thoughts of being injured, overcome with fear, or other bad things’ (item 3) and ‘avoided, or did not approach or enter, these situations’ (item 6) on a Likert Scale from 0 to 4 (where 0 is never, and 4 is all of the time).
Additional idiosyncratic measures were collaboratively created by the therapist and Mr A of Mr A’s stair-confidence level and belief in threat-related cognitions. These were quantitative measures, scoring belief and confidence from 0 to 100%, with 0% representing no belief/confidence and 100% representing total belief/confidence. These were created in light of the key role threat-related cognitions and confidence level were hypothesised to play in the maintenance of Mr A’s phobia. These measures were created in the first therapy session as part of the formulation work. As such, no baseline measures could be collected prior to intervention.
Formulation
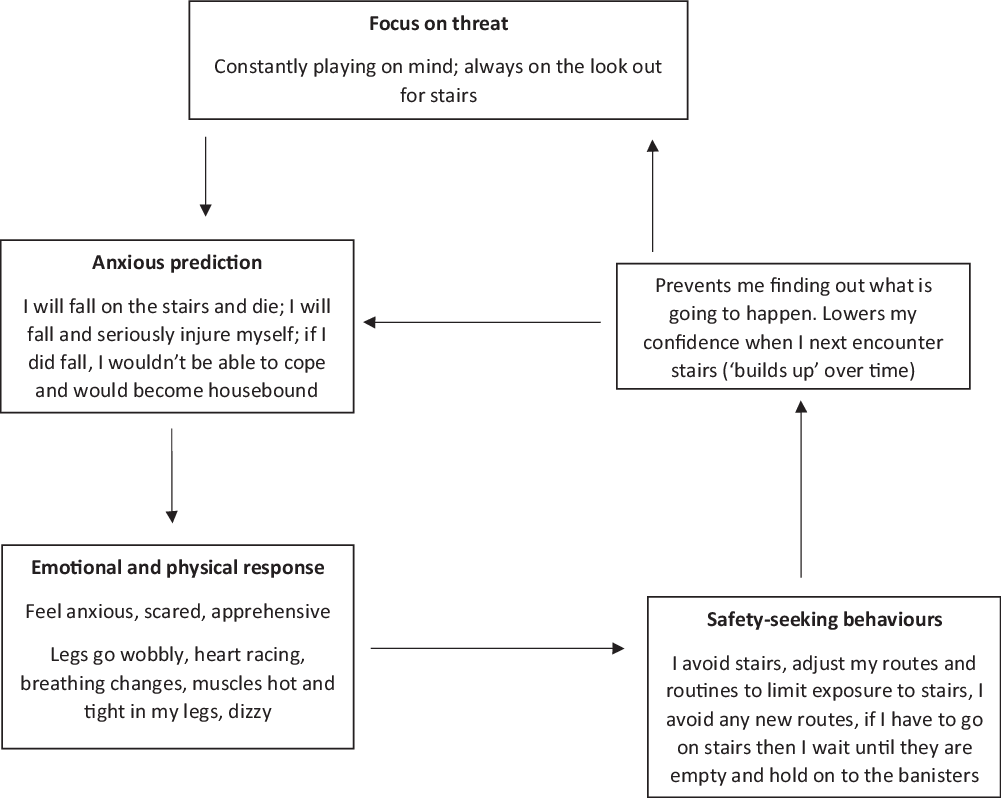
The initial focus of therapy was the collaborative development of an idiosyncratic formulation by Mr A and the therapist. The formulation was generated by exploring a recent example of Mr A’s difficulties, and drew on Kirk and Rouf’s (Reference Kirk, Rouf, Bennett-Levy, Butler, Fennell, Hackmann, Mueller and Westbrook2004) evidence-based model of specific phobia (Fig. 1).
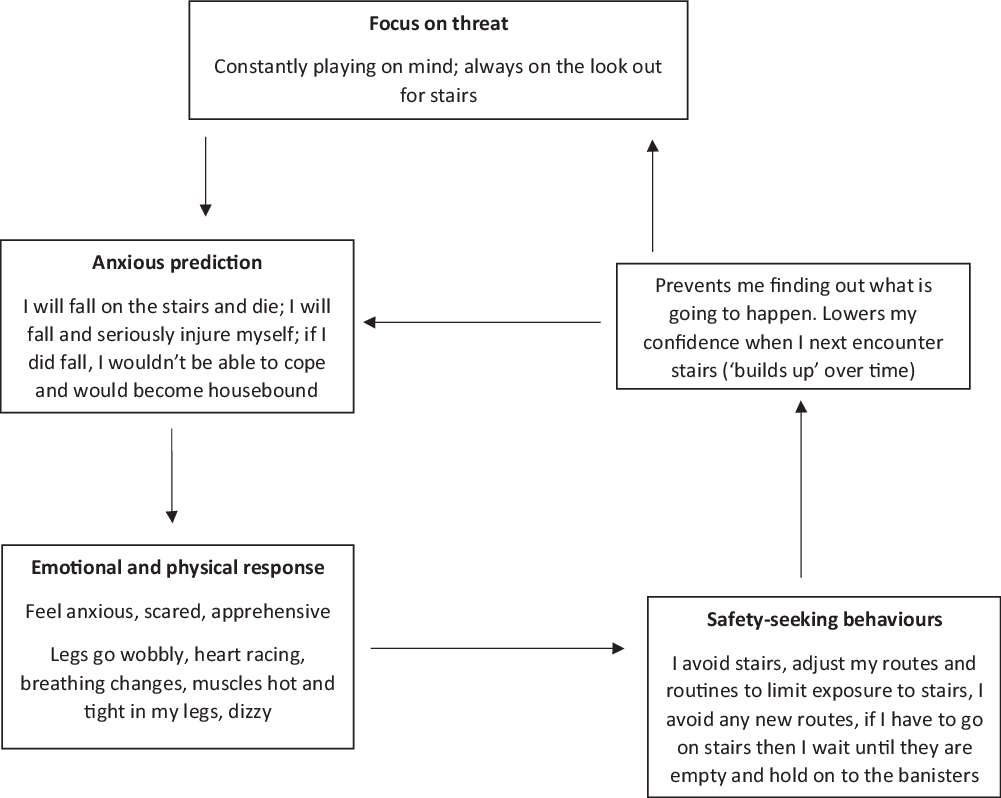
Figure 1. Cross-sectional formulation based on Kirk and Rouf (Reference Kirk, Rouf, Bennett-Levy, Butler, Fennell, Hackmann, Mueller and Westbrook2004) cognitive model of phobia (Kennerly et al., Reference Kennerley, Kirk and Westbrook2016).
It was hypothesised that Mr A’s difficulties were a result of his beliefs in relation to stairs. These thoughts were posited to have resulted from Mr A’s fall 10 years ago, which had led him to ruminate on and subsequently catastrophically over-estimate the threat level associated with stairs as well as under-estimate his ability to cope. It was hypothesised that Mr A’s interpretations of stairs as threatening and his coping ability as low were maintaining his phobic response (Raes et al., Reference Raes, Koster, Loeys and De Raedt2011; Shafran et al., Reference Shafran, Booth and Rachman1993; Thorpe and Salkovskis, Reference Thorpe and Salkovskis1995).
A number of psychological processes were hypothesised to be maintaining Mr A’s catastrophic beliefs over time. Mr A reported ongoing hypervigilance in relation to stairs. It was hypothesised that this hypervigilance was increasing regularity of his phobic responses and subsequently reinforcing his threatening appraisals of stairs via selective attention to phobic triggers (Kirk and Rouf, Reference Kirk, Rouf, Bennett-Levy, Butler, Fennell, Hackmann, Mueller and Westbrook2004; Mogg and Bradley, Reference Mogg and Bradley2006). In addition, Mr A reported subsequently experiencing high levels of anxiety and apprehension, and physical sensations of anxiety (wobbly legs, muscular tension, heart racing, etc.) when encountering stairs. It was hypothesised these unpleasant emotional and physical responses might be reinforcing his belief that stairs were ‘dangerous’ and to be feared.
Finally, Mr A reported coping with these thoughts, feelings and sensations by avoiding stairs wherever possible. If he had to climb stairs, Mr A reported ensuring he held on to something and that he was the only one on the stairs to keep himself safe. These behaviours were formulated as safety-seeking behaviours which, whilst initially alleviating anxiety, prevented Mr A in the long-term from testing his cognitions. It was hypothesised that this may in turn be maintaining Mr A’s difficulties, by preventing updating of his stair-related beliefs (Kennerley et al., Reference Kennerley, Kirk and Westbrook2016). Mr A reflected that his avoidance of stairs caused a decrease in his confidence in relation to stairs. Mr A and the therapist hypothesised this lowered confidence may be reinforcing his threat-related cognitions and fuelling his hypervigilance (Kennerley et al., Reference Kennerley, Kirk and Westbrook2016).
It was recognised that some of these maintaining factors were likely to be augmented by Mr A’s co-morbid mental health difficulties. For example, as discussed above, Mr A was moderately socially isolated at the time of treatment, lacking a support network outside of the mental health team and a structured routine. Mr A reflected that this was a result of his psychosis affecting his functioning, and making it more difficult for him to maintain a routine and relationships over time. It was hypothesised that these factors facilitated Mr A’s avoidance, by reducing the necessity of him facing his phobia regularly, and thus may have further entrenched some of his phobic responses. This was held in mind moving into the intervention, as it was appreciated the lack of a robust support system might act as a barrier to treatment.
Treatment orientation
Based on the key role Mr A’s stair-related cognitions appeared to play in his difficulties, a cognitive behavioural approach to treatment was selected as opposed to a habituation-based exposure approach, as informed by NICE guidelines (National Institute for Health and Care Excellence, 2013), existing research (Choy et al., Reference Choy, Fyer and Lipsitz2007; Thng et al., Reference Thng, Lim-Ashworth, Poh and Lim2020; Wolitzky-Taylor et al., Reference Wolitzky-Taylor, Horowitz, Powers and Telch2008) and Mr A’s idiosyncratic formulation.
Course of therapy
Mr A participated in 11 sessions over 12 weeks (one assessment session and 10 intervention sessions). Throughout the intervention, the therapist was guided by key CBT principles including collaboration and empathy, and utilised core techniques such as guided discovery and Socratic questioning (Kuyken et al., Reference Kuyken, Padesky and Dudley2017). Additionally, homework was used throughout to build on the work done in session.
Sessions 1–2: formulation and psychoeducation
An idiosyncratic formulation was developed in collaboration with Mr A (Fig. 1). The accuracy of this formulation was tested out during, and in between, sessions 1 and 2 using in vivo exposure and through Mr A completing thought diaries. Any new insights were added into the formulation until Mr A felt it was an accurate reflection of his experience (Kuyken et al., Reference Kuyken, Padesky and Dudley2017). Psychoeducation was then completed on the effects of anxiety, with a particular focus on the physiological impact. This information was used to begin cognitive restructuring, particularly focusing on Mr A’s beliefs that the physiological symptoms of anxiety he experienced were indicative of the ‘dangerous’ nature of stairs. In addition, we began to discuss the ‘thinking traps’ associated with anxiety, and identify which of these might apply to Mr A.
Sessions 3–4: cognitive restructuring
Cognitive restructuring was used to update Mr A’s beliefs about the dangers associated with using stairs. This involved reviewing evidence for and against Mr A’s stair-related beliefs, via evidence gathered via collaborative information-gathering (for example, into the mortality rates of death by stairs), surveys (for example, exploring how often other people fell down stairs and how seriously they were injured from this), and reviewing Mr A’s own experiences of stair-use.
Sessions 5–9: behavioural experiments
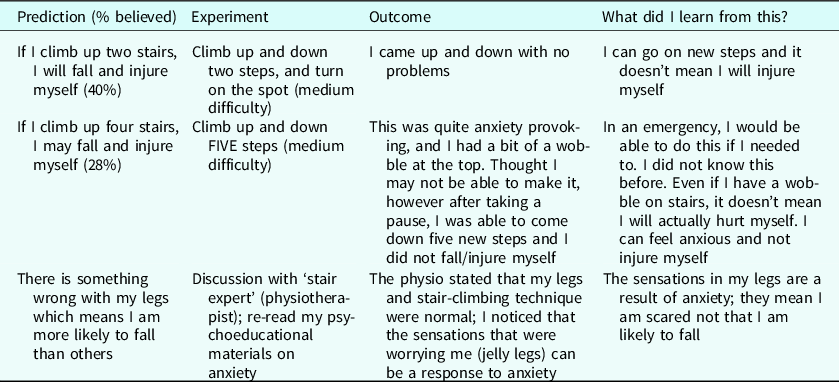
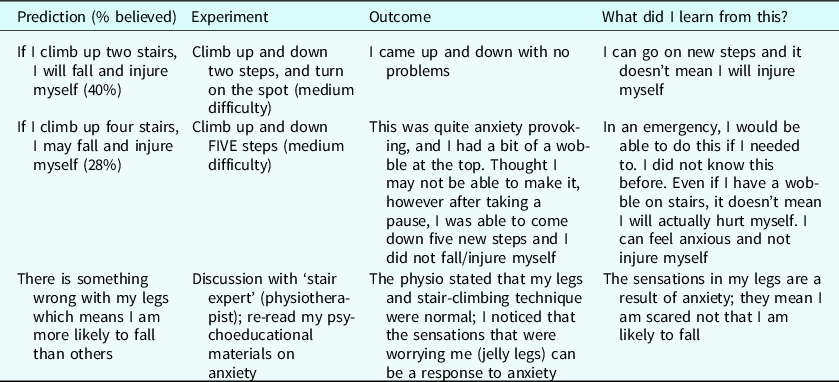
In vivo behavioural experiments were carried out in session and as homework to test out Mr A’s beliefs in relation to stairs. These primarily focused on testing Mr A’s predictions in relation to what may happen if he reduced his avoidance of stairs and reduced the use of his safety behaviours (see Table 1 for examples). An emphasis was placed on identifying key learning from the experiments and cognitive restructuring from the behavioural experiments. As a CBT approach was being used as opposed to a habituation-based exposure model, a fear hierarchy was not constructed. Instead, the focus was on collaboratively designing experiments which would test out specific idiosyncratic beliefs. These behavioural experiments included consultation with a ‘stair expert’ (a physiotherapist).
Table 1. Examples of behavioural experiments completed in session and as homework
Session 10: relapse management work
Session 10 was spent reflecting on therapeutic process, identifying key learning and what had been most helpful about the intervention. This was then incorporated into a collaboratively written therapeutic blueprint. Mr A highlighted the collaborative approach to therapy, as well as the development of a shared understanding of his difficulties, as key in helping him make positive changes. He reported finding this enabled insight into why he might be struggling, and what he could do to empower himself to overcome his difficulties. In addition, Mr A reported that the incorporation of discursive cognitive restructuring was beneficial prior to engaging in the behavioural experiments, as they introduced enough doubt in relation to his beliefs to allow him to feel more comfortable about engaging with the behavioural experiments.
Impact of co-morbid complexities on the intervention
The context of Mr A’s co-morbid difficulties was noted to impact on the process of the intervention in a number of ways. Mr A’s lack of a robust support network, in part a result of Mr A’s longer standing mental health difficulties, presented some challenges around engagement. Typically, we may hope that a client’s social network would enable the person to engage in treatment, particularly providing support at more challenging aspects of the intervention. Without this, it was noted that more work had to be done on motivating Mr A to remain engaged with the intervention, with particular attention having to be paid to supporting Mr A to generalise learning from the sessions and engage in tasks at home. Furthermore, Mr A’s lack of a varied daily routine meant his organic opportunities to challenge himself around his phobia were limited. As such, Mr A had to actively seek out opportunities to complete homework tasks which presented an additional level of challenge. In addition, the impact of Mr A’s voices on his sleep, as well as his medication, resulted in some cognitive challenges to therapy, including clarity of thought, processing speed and thus his ability to understand concepts being raised. Moreover, his longer-term psychotic experiences appeared to have left Mr A feeling less confident in himself, and thus set-backs in therapy appeared to have a more significant emotional impact than otherwise might be expected.
Throughout the intervention there was a general sense that due to the impact of Mr A’s complex co-morbidities on his life the social and internal resources he held were more limited, which in turn made engaging in therapy more challenging. Thus, there was a need for the therapist to intentionally spend more time building Mr A’s internal motivations for therapy, as well as his confidence and resilience to set-backs, to account for this lack of resources which may have enabled him to do this otherwise. This highlighted the need to consider how co-morbidities might indirectly effect the specific symptoms being targeted through impacting wider functioning and the resources an individual can draw on to engage with this treatment episode. There may be a greater need to focus on engagement when working with these complex cases, as more barriers to engagement may be encountered by this client group with less resources present which enable these to be overcome.
Outcome
Mr A’s symptoms of specific phobia showed some fluctuation at baseline (phase A). Mr A reported that this accurately reflected how his difficulties could ‘vary from week to week’, depending on encountered triggers. Mr A’s average raw score on the SMSP-A was 32, indicating a severe phobia at baseline (Craske et al., Reference Braga, Reynolds and Siris2013).
Mr A’s scores on the SMSP-A reduced over the course of therapy, with a reduction from an average score of 32 at baseline to 9 in session 11, indicating a change from a severe to mild phobia (Craske et al., Reference Craske, Wittchen, Bogels, Stein, Andrews and Lebeu2013) (Fig. 2). This suggests that Mr A’s overall phobia symptomology was significantly lower by the end of treatment.
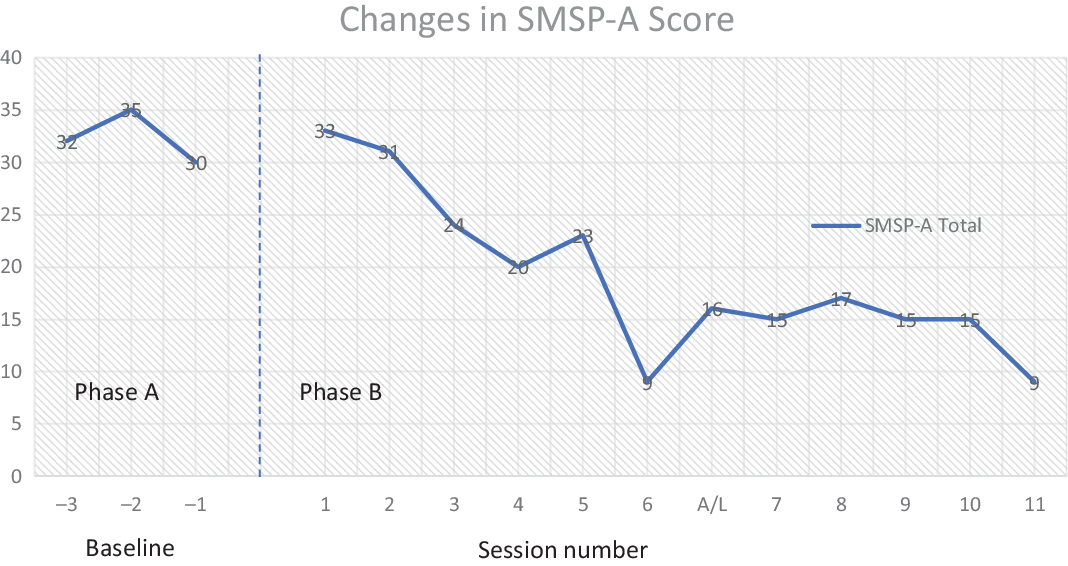
Figure 2. Changes in SMSP-A score throughout treatment.
Reductions were seen on all measure items, with changes of particular note seen on items 3 and 6. A clear reduction was seen on both items, from an average score of 4 at baseline, to 1 in the final session on item 3, and an average score of 3.3 at baseline to 0 in the final session on item 6 (Fig. 3). These changes are important given the important role threat-based cognitions and avoidance were hypothesised to play in Mr A’s phobia maintenance (Kirk and Rouf, Reference Kirk, Rouf, Bennett-Levy, Butler, Fennell, Hackmann, Mueller and Westbrook2004). This link between these aspects of Mr A’s presentation and his overall phobia severity is reflected in the comparative changes noted between items 3 and 6, and Mr A’s overall scores on the SMPS-A. In particular, there appears to be a clear parallel between the regularity of Mr A’s threat-cognitions, and his overall phobia symptoms, supporting the key role of these beliefs in his phobia as posited in the original formulation. In addition, this reduction in avoidance reflected in the measure changes is likely to have wider implications for Mr A’s wellbeing than changes in his phobia symptoms alone. In particular, a reduction in avoidance is likely to open up more opportunities for enjoyable activities and social engagement than previously were an option for Mr A. It is likely that this will have a wider impact on Mr A’s wellbeing and may enable improved mood as well as impacting positively on his ongoing psychotic symptoms.
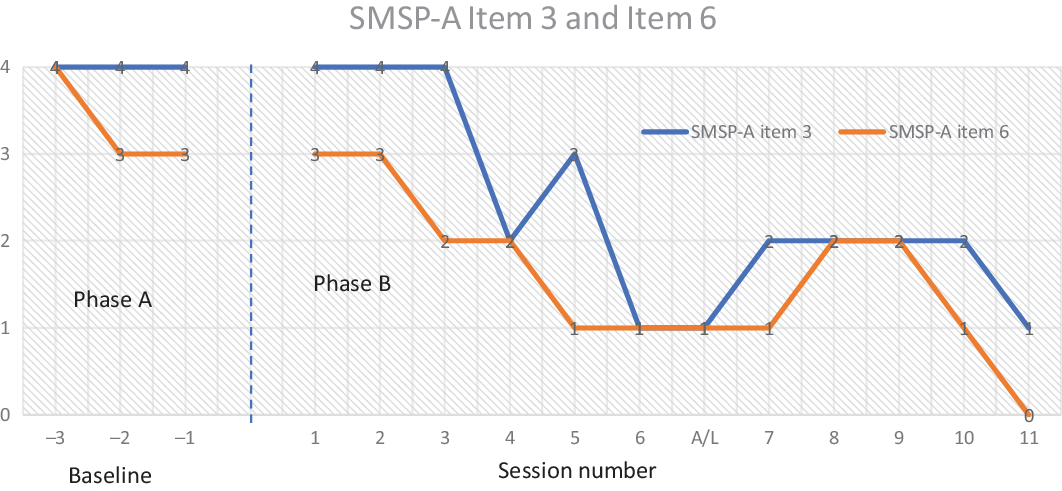
Figure 3. Changes on SMSP-A item 3 (regularity of threat-cognitions) and item 6 (regularity of avoidance) throughout treatment.
Interestingly, a slight spike is seen in symptoms between sessions 4 and 5, followed by a significant reduction in symptoms in session 6. It was hypothesised this might reflect a temporary increase in anxiety following Mr A beginning to engage in the interventive behavioural experiments. It is not unexpected that this might cause an initial increase in anxiety, as the safety behaviour of avoidance had been reduced. However, this seemed to quickly resolve, perhaps reflecting the cognitive restructuring that would have occurred after Mr A engaged in the experiments and did not experience harm.
Changes were also seen on the idiosyncratic measures designed by the therapist and Mr A. In line with changes noted above, a clear reduction in belief of threat-cognitions was seen across sessions, with a decrease from 90% in session 1 to 8% in session 11 (Fig. 4). As above, a similar trend can be seen in the reduction of Mr A’s belief in his threat-cognitions, and his overall phobia symptom level. This again is likely to reflect the key role of Mr A’s threat-cognitions within his phobia, as posited in the formulation. Interestingly, however, we do not see a spike in Mr A’s belief levels from sessions 4 to 5, as is seen on his general symptom scores. This may reflect that a change in belief levels alone is not enough to result in symptom change. Rather, this must be combined with a reduction in avoidance and behavioural changes to embed this cognitive learning further. This supports the use of both cognitive restructuring and exposure-based interventions found within CBT treatment of phobias.
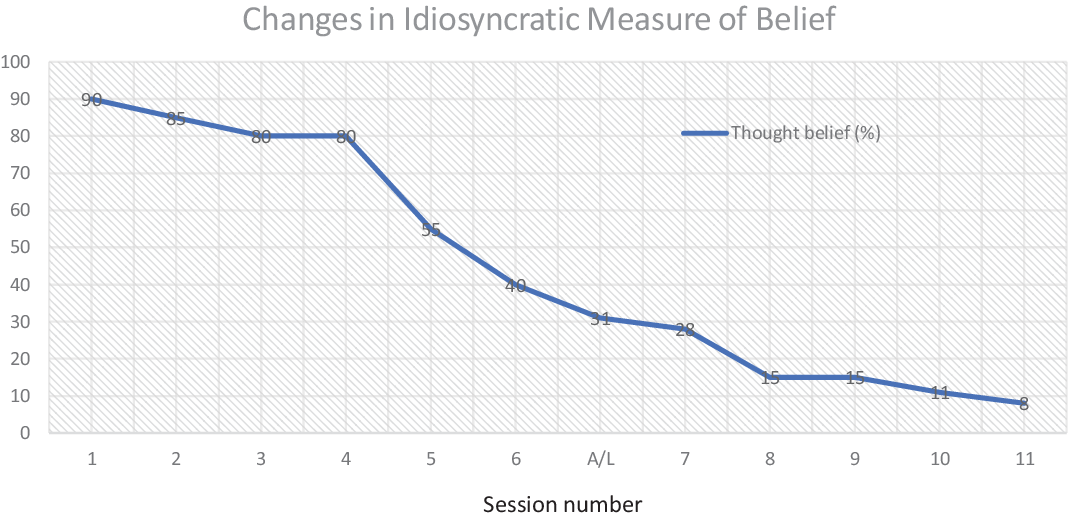
Figure 4. Changes in idiosyncratic belief rating of threat-cognitions throughout treatment.
Moreover, Mr A’s self-rated confidence level increased during treatment, from 0% in session 1 to 70% in session 11 (Fig. 5). Interestingly, whilst we did not measure this and it was not a treatment goal, Mr A did provide informal feedback that his general self-confidence and self-efficacy had positively increased from this treatment episode. Thus, it appeared the intervention may have had a further reaching impact on Mr A’s general wellbeing as opposed to only specifically impacting on the targeted symptom set.
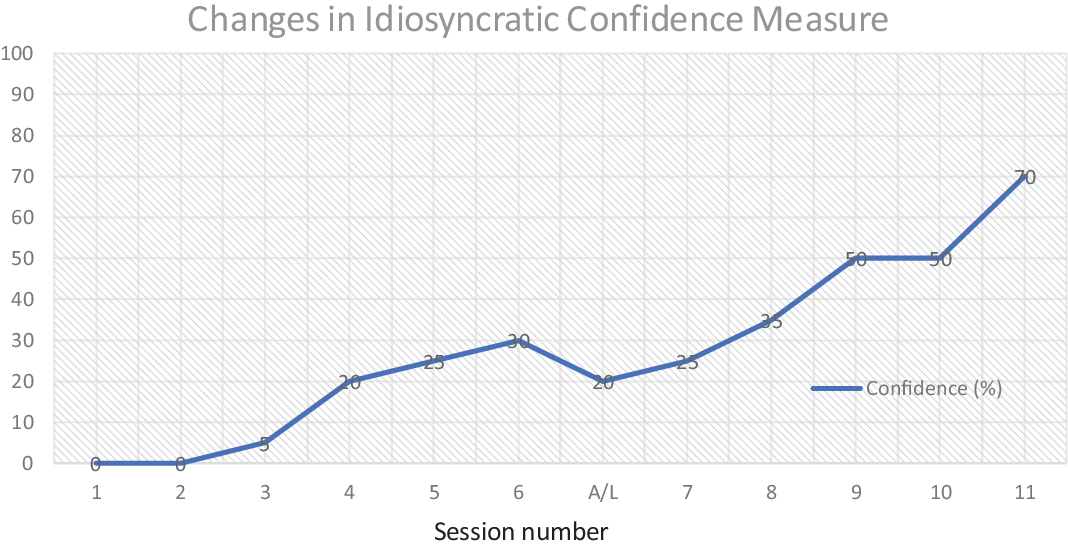
Figure 5. Changes in idiosyncratic ratings of confidence throughout treatment.
Goals
By the end of therapy, Mr A had achieved all his goals. He had managed to climb seven stairs, his confidence had risen to 70% and he was re-engaged in his identified enjoyable activities.
Discussion
This case study describes a piece of CBT work targeted at symptoms of a specific phobia of stairs in the context of a client with a long-standing co-morbid diagnosis of schizophrenia. Findings showed that the therapeutic approach was effective, with significant reductions seen in overall phobia symptoms, showing a clinically significant change from severe to mild phobia by the end of treatment. These findings cohere with other case studies where significant improvements to targeted symptom sets were seen following CBT treatment despite wider complexity (Dudley et al., Reference Dudley, Dixon and Turkington2005).
Clinical implications
This study has a number of implications for clinical practice. It not only adds to evidence that CBT interventions can be utilised effectively in this targeted manner, but also gives a detailed example of how this approach can enacted within clinical practice. This piece of work focused exclusively on Mr A’s specific phobia, and as a result a diagnosis-specific treatment approach was followed, which resulted in significant improvements to Mr A’s phobic symptoms. This indicates that diagnosis-specific CBT can be effectively used in a targeted manner within the context of existing co-morbid presentations. It also highlights that formulation and intervention can be useful when deliberately focused only on one aspect of an individual’s wider difficulties without looking to integrate understanding of that symptom set within a more thorough shared formulation. In fact, explicitly focusing on a specific aspect might be experienced as more containing and accessible for clients, particularly if their own experience of their mental health difficulties is that they are complex and overwhelming. Certainly, Mr A reported a desire within our sessions to focus exclusively on his phobia symptoms within this therapeutic episode, expressing that this helped him feel the issue we were tackling was manageable. Thus, this case study highlights one way in which clinicians can consider applying CBT theory when working with complexity and co-morbidity in their practice.
This case study highlighted the reciprocal nature of co-morbid mental health difficulties, and importance of holding this in mind when considering treatment approaches. The context of Mr A’s complex co-morbidities was noted to impact on the process of therapy, particularly around the need for the therapist to adopt a more fundamental role in intentionally building the internal resources necessary to allow meaningful engagement. Moreover, the outcomes of this specific targeted intervention appear to have a more far-reaching impact on Mr A’s general mental wellbeing than just on his phobia, with Mr A indicating his general levels of confidence and self-efficacy had increased within therapy. This highlights how additional complexities can both make targeted CBT treatment approaches more challenging, but also the wider reaching positive impact these approaches can have when carried out successfully. Moreover, it highlights the importance of the therapist holding in mind the wider complex context even when this is not the focus of the treatment, as this will alter how the individual will engage in treatment.
It may be that this targeted clinical approach is particularly appropriate where certain symptoms are impeding a client’s ability to engage more widely in their treatment and preventing general recovery goals being met. Prior to this intervention, Mr A’s phobia was limiting his functioning to a point where he was unable to partake in behavioural activation and social engagement initiatives which were felt to be important for his wider psychological recovery. This targeted intervention enabled changes with regard to a specific symptom set which in turn had wider ripple effects on his recovery journey more widely, and thus whilst a targeted therapeutic intervention might not serve as the whole of a client’s treatment, it may be a useful stepping stone which enables clients to engage with their recovery plan more effectively and reach their goals. Certainly, this coheres with studies showing diagnosis-specific CBT to have transferable effects to co-morbidities that a client may be experiencing (Allen et al., Reference Allen, White, Barlow, Shear, Gorman and Woods2010; Bauer et al., Reference Bauer, Wilansky-Traynor and Rector2012; Dudley et al., Reference Dudley, Dixon and Turkington2005;). Thus, it might be beneficial for clinicians to consider using a targeted intervention where their wider case conceptualisation suggests that a particular set of difficulties may act as a therapeutic barrier for recovery (for example, in a case where a client’s agoraphobia prevents them engaging in behavioural activation that might address their primary presenting symptoms of depression).
This case also highlights the benefits of approaching cases from a multi-disciplinary perspective. It would be difficult to work in the above-described focused therapeutic way if any complex or co-morbid difficulties were not being appropriately held by the wider team around the client, particularly where there are issues of risk. Having the multi-disciplinary structure allowed the therapist to utilise their specific skill set to work most effectively with the client on the identified issue. Thus, this case highlights the usefulness of taking a multi-disciplinary team approach to treatment particularly with complex cases, to provide space for different professionals to focus their work with these clients.
Finally, it was interesting to note that Mr A highlighted the usefulness of cognitive restructuring techniques as enabling him to feel more able to engage in the behavioural experiments that served as a key aspect of the intervention. Certainly, studies have found that whilst in vivo exposure work seems to result in significant symptom changes for phobic presentations, there are high rates of drop-out in exposure-based therapy, and that including cognitive restructuring alongside in vivo exposure can make therapy more tolerable to clients and reduce this rate of drop-out (Botella Arbona et al., Reference Botella Arbona, Bretón-López, Serrano Zárate, García-Palacios, Quero and Baños Rivera2014; Choy et al., Reference Choy, Fyer and Lipsitz2007; Foa et al., Reference Foa, Hembree, Cahill, Rauch, Riggs, Feeny and Yadin2005; Li and Graham, Reference Li and Graham2020; Mattick et al., Reference Mattick, Peters and Clarke1989). Thus, this study further supports that cognitive restructuring could serve a key role in facilitating engagement within the psychological treatment of specific phobia.
Limitations
It is important to note the limitations of this study. As a single case study, these findings lack replication and thus it is unclear how far findings can be generalised. Further research replicating these findings is needed. In addition, future studies would be strengthened by including a longer, staggered baseline.
It is also important to note that baseline measures were gathered during the assessment period. On the one hand, it is possible this may have confounded scores by contact with the therapist, and thus is a limitation of the design. However, on the other hand, it allowed a shared consensus between the therapist and Mr A on what the main difficulties were and allowed selection of measures that best captured these. Thus, whilst this might have limited the strength of the design somewhat, this was with a trade-off of more idiosyncratically appropriate measures being selected.
Mr A was receiving ongoing input from the multi-disciplinary team during treatment in the form of anti-psychotic medication and monthly visits from his care co-ordinator. As such, it is difficult to delineate the impact of this intervention on Mr A’s phobia symptoms compared with the impact of this wider care. However, Mr A had been receiving input of this type for a number of years without showing progress in his phobia and no changes to Mr A’s medication were made during this therapy episode. Thus, we may tentatively argue that a proportion of Mr A’s improvements are likely to have resulted from the above-described intervention.
Finally, the lack of follow-up data is an important limitation to note. However, this case study nonetheless is an interesting first step highlighting the important role targeted CBT can play in clinical work. Further follow-up research addressing the above identified limitations is needed to build on this.
Reflections
We were aware during assessment of Mr A how complex and long-standing his history of mental health difficulties and interactions with mental health services were. We were mindful of a pull to explore these wider aspects of Mr A’s experiences, and a desire to address those complexities within the current intervention and formulation. It was interesting to reflect that a potential barrier to completing this targeted intervention could therefore have been our own therapeutic curiosity and need to make sense of the whole picture. However, drawing on those core CBT principles of collaborative and shared meaning-making helped maintain our focused approach, as working specifically on the phobic symptoms was identified by Mr A as his primary wish. Ensuring a balance was maintained between remaining targeted in the CBT work, whilst also adapting to any additional challenges raised by the complex context within which the treatment was occurring, was a particularly challenging aspect of this work. Generally, we found working in a multi-disciplinary manner allowed us to maintain focus on how this intervention fitted into Mr A’s wider recovery plan, and thus ensure the targeted approach was maintained. Working as part of the wider multi-disciplinary team enabled us not to take responsibility for Mr A’s recovery plan as a whole, but rather specifically focus our skills on the particular contribution we could most usefully make. It feels like this is particularly effective as an approach for complex clients, with the multi-disciplinary environment enabling different professions to make distinct, useful contributions using their specific skill sets and thus ensure the best overall recovery plan is enacted for the client.
Acknowledgements
We would like to acknowledge Mr A for his hard work and bravery throughout therapy, and thank him for permitting the submission and publication of an anonymised account of his therapy by the research team.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
The authors have no conflicts of interest with respect to this publication.
Ethical statement
No specific ethical approval was required for this work, as it was an evaluation of a piece of routine clinical practice. Researchers have abided by the Ethical Principles of Psychologists and Code of Conduct as laid out by the British Psychological Society and British Association for Behavioural and Cognitive Psychotherapies. Informed consent was given by Mr A both to participate in therapy, and for this work to be written up and submitted for publication. Identifying details and names have been changed to ensure Mr A’s confidentiality is maintained.
Key practice points
(1) CBT can be effectively utilised to target particular aspects of an individual’s presentation when they are experiencing complex or co-morbid difficulties.
(2) Using targeted CBT might be a particularly useful technique where specific symptom sets are preventing an individual from being able to engage more fully in their treatment or reach recovery goals. Here, using a targeted intervention to first tackle the aspects of an individual’s presentation that might act as therapeutic barriers may enable improvements more generally in the client’s mental health.
(3) This case study highlights the utility of a multi-disciplinary approach in relation to complex cases. Utilising an MDT allows professionals to maximise their specific skill-sets by focusing their input to a client.
(4) The use of cognitive restructuring techniques were experienced as therapeutically beneficial, and enabled the client to engage more confidently in later behavioural experiments. This suggests that including cognitive techniques within phobia treatment, as opposed a pure habituation exposure-based treatment approach, might be clinically useful.






Comments
No Comments have been published for this article.