Paediatric psychiatric emergencies typically comprise self-harm, acute manifestations of mental illness and severe behavioural disturbances including violence. Reference Edelsohen, Braitman, Rabinovisch, Sheves and Melendez1 Frequently, young people in psychosocial crisis situations also present to hospital. Accident and emergency (A&E) departments have aptly been described as ‘the only game in town’ outside normal working hours. Reference Soskis2 This is where young people in a crisis situation take themselves or are taken by others, and their numbers are increasing even though professional help is not always sought. Reference Grupp-Phelan, Harmon and Kelleher3,4 Often help is initially offered by paediatric nurses and doctors, who then liaise with child and adolescent psychiatrists. Reference Street5
Guidance regarding the management of paediatric psychiatric emergencies has mainly been published with regard to self-harm; and the need for a comprehensive specialist psychosocial assessment has been emphasised in the UK since 1998. 6,7 Although improved and timely access to specialist services is a UK government target, currently only a quarter of child and adolescent mental health services (CAMHS) provide emergency cover outside normal working hours. 8,Reference Storey and Statham9 Many CAMHS still have to establish emergency duty services. A good understanding of when demand is likely to be at its greatest will help with service planning. So far, research into cyclic variations in psychiatric emergencies has mainly focused on adults and self-harm. How often and when individuals present to psychiatric emergency services is influenced by the organisation of the wider support networks, referral pathways and admission policies. Considerable variation in these service-dependent factors has been reported. Reference Bennewith, Gunnell, Peteres, Hawton and House10-Reference Hawton, Bergen, Cassey, Simkin, Plamer and Cooper12 However, fluctuations in emergency presentations have also been linked to service-independent factors such as diurnal, seasonal and meteorological variations. For example, more individuals present in the evening and at weekends, in spring, and on days with nice weather. Reference Rushton, Bruckman and Kelleher13-Reference Blenkiron16
This study set out to investigate cyclic variations in demand for paediatric psychiatric provision outside normal working hours in a large and diverse urban population. We wanted to find out whether service-dependent factors such as the availability of liaison daytime cover, the introduction of A&E waiting targets or high A&E workload were associated with demand for out-of-hours provision. We also investigated whether service-independent factors such as school holidays, the season and the weather related to demand.
Method
Setting
This study was based at three inner-city teaching National Health Service (NHS) hospitals in north London and included University College London Hospitals, the Royal Free Hospital and the Whittington Hospital. All three sites had A&E departments providing year-round 24-hour access and paediatric in-patient facilities. The hospitals provided services for young people presenting in crisis situations. All three hospitals worked closely with the local CAMHS, which were open on working days between 09.00 h and 17.00 h. The three hospitals catered mainly for the boroughs of Camden and Islington, with a combined population of 373 817 and high ethnic and socioeconomic diversity according to 2001 census data. Reference Jessen, Steffensen and Jensen17 However, the hospitals did not have clearly defined catchment areas and young people frequently came from neighbouring boroughs or other regions of the UK owing to the hospitals' proximity to major railway links.
The out-of-hours service in child and adolescent psychiatry was provided by senior trainee doctors undertaking specialist training at the Tavistock Clinic (specialist registrars), who had access to consultant cover at all times. The trainee doctors consulted with the paediatricians and junior trainees in general psychiatry (senior house officers) at the three hospital sites. Young people in crisis were usually first dealt with by professionals on site, who then decided whether or not input from the out-of-hours service in child and adolescent psychiatry was required.
The vast majority of young people accessing the out-of-hours service did so by presenting to A&E. A minority were already in-patients on paediatric wards having been admitted for physical illness or psychosocial reasons and their paediatricians asked for management advice. Young people could self-present to A&E, or they were brought to A&E by their parents, their social worker or the police. General practitioners (GPs) could also organise a transfer to A&E. Yong people referred to the out-of-hours service typically presented with self-laceration or overdoses compounded by uncooperative behaviour or severe family dysfunction, acute episodes of mental illness or psychosocial crises leading to a need for an urgent placement outside the family home. These presentations often generated high levels of concern in the professional network.
Data collection
Data on all referrals to the out-of-hours service in child and adolescent psychiatry were collected prospectively. Trainee doctors were required to complete an electronic audit form for each referral and forms were collected centrally. Regular reminders were sent out to ensure complete ascertainment of all referrals. Monthly on-call supervision meetings were held to maximise consistency between trainees. Data collection was fully compliant with the Data Protection Act of 1998. The current study solely relied on data routinely collected for service evaluation and did not require ethics review by the NHS National Research Ethics Service.
The date and time of the referral was recorded, as was the individual's date of birth and gender. The on-call doctor documented the reason for the referral, how long they spent dealing with it, whether it was a bedside assessment or telephone consultation, and whether or not the referral was deemed appropriate for the out-of-hours service in child and adolescent psychiatry. The present study includes all young people aged 18 and under referred to the out-of-hours service in child and adolescent psychiatry in the period between 1 January 2002 and 31 December 2005.
Variables analysed
The daily referral rate was the dependent variable and the independent variables investigated are listed below.
No daytime cover
A child and adolescent psychiatry hospital liaison service was available during normal working days at each of the three hospital sites. The referral frequency on days with daytime liaison cover and those without (e.g. weekends, public holidays) was compared.
A&E workload
The number of people waiting for 3 or more hours on each day was obtained for the three hospital sites. The A&E workload was defined as ‘high’ on days when the number of individuals waiting fell into the upper quartile for the site. The site-specific quartiles were calculated separately for each year.
Changeover of senior house officers
At each of the three hospitals, all junior doctors working in A&E changed jobs in the same week in February and August. The referral frequency during the 8 weeks before changeover was compared with that of the 4 weeks afterwards.
Protocol changes
All three sites used different protocols to detail the referral pathways to the out-of-hours service in child and adolescent psychiatry. These were amended with the aim of tightening referral procedures and increasing the number of appropriate referrals at all three sites at different time points. In order to analyse whether the protocol changes resulted in a change in the referral frequency, the last 100 days before the change were compared with the first 100 days afterwards for each site.
Introduction of the 4-hour A&E waiting time target
Hospitals in England were paid incentives when they met 4-hour A&E waiting time targets as of 1 January 2004. The referral rates in the years before and after the introduction of the target were compared.
School holidays
The school dates of the borough of Camden were used to compare the referral frequency on days when pupils were expected to be in school with days when they were not.
Spring
The referral frequency for days in spring (21 March to 21 June) was compared with that of the other days in the year.
Hot and rainy days
Meteorological data were obtained from the Meteorological Office for each day during the study period. Days with a mean temperature above 20°C (i.e. 9.1% of all days during the study period) were coded as ‘hot’ and those with more than 4 mm rainfall as ‘rainy’ (i.e. 11.2%).
Statistical analysis
The chi-squared test was used to compare the distribution of referrals in the specified period with its comparison period (e.g. normal working days v. holidays). Odds ratios and their confidence intervals were calculated using EpiInfo6 (Centers for Disease Control and Prevention, USA; www.cdc.gov/epiinfo/epi6/ei6.htm) on Windows XP Professional. Stratification according to hospital site was used for the analysis of service-dependent variables and pooled odds and their confidence intervals were obtained by using the Mantel-Haenszel method. Whether pooled odds ratios could be used or whether differences over strata were significant was assessed by the Breslow-Day test. Multivariate analyses were not performed because of the covariation of the different independent variables under investigation. 18
For the power calculation it was assumed there would be one referral every 4 days and that 20% of the days in the 4-year study period carried an increased risk of a referral (e.g. no daytime cover). Given this, the present study had 81.5% power to detect odds ratios of 1.5 or greater with α = 0.05.
Results
Between I January 2002 and 31 December 2005 a total of 323 young people were referred to the out-of-hours service in child and adolescent psychiatry. Of these, 118 (36.5%) required a bedside assessment, whereas for 205 (63.5%) a consultation was given on the telephone. Based on 2001 census data, Reference Jessen, Steffensen and Jensen17 this equals to 21.6 (95% CI 19.3-24.0) referrals per 100 000 general population per year for either telephone consultations and bedside assessments taken together and 7.9 (95% CI 6.5-9.3) per 100 000 general population per year for bedside assessments only. There was no significant fluctuation in the yearly referral rate over the 4-year period, which was 76 in 2002 (95% CI 59-93), 89 in 2003 and 2004 (95% CI 71-107) and 69 in 2005 (95% CI 53-85) (χ2 = 3.024, d.f. = 3, P = 0.39).
Details of the referrals received are given separately for bedside assessments and for telephone consultation and bedside assessment combined in Table 1. The breakdown according to age revealed almost half of the referrals concerned young people over 16 years of age.
Table 1 Characteristics of referrals to the out-of-hours service in child and adolescent psychiatry
| n (%) | ||
|---|---|---|
| Phone consultation and bedside assessment combined (n = 323) | Bedside assessment only (n = 118) | |
| Gender, male | 110 (34) | 48 (41) |
| Age, years | ||
| 0–12 | 36 (11.0) | 13 (11.0) |
| 13–15 | 139 (42.9) | 51 (43.5) |
| 16–18 | 148 (46.0) | 54 (45.2) |
| Referral time | ||
| 09.00–12.59 | 55 (17.0) | 34 (28.8) |
| 13.00–16.59 | 34 (10.5) | 18 (15.3) |
| 17.00–20.59 | 93 (28.8) | 28 (23.7) |
| 21.00–00.59 | 86 (26.6) | 27 (22.9) |
| 01.00–04.59 | 41 (12.7) | 7 (5.9) |
| 05.00–08.59 | 14 (4.3) | 4 (3.4) |
| Time taken | ||
| 0–1 h | 170 (52.6) | 3 (2.8) |
| 1–4 h | 81 (25.2) | 55 (46.7) |
| >4 h | 72 (22.2) | 60 (50.5) |
| Referral was appropriate | 255 (79.0) | 106 (89.8) |
The diurnal distribution of referrals is shown in Fig. 1. Throughout the day the peak in total referrals occurred between 17.00 h and 00.59 h, and the trough in the referral activity was between 01.00 h and 08.59 h. There was an additional peak in referral activity between 09.00 h and 12.59 h, which was as a result of referrals received on days without daytime liaison cover.
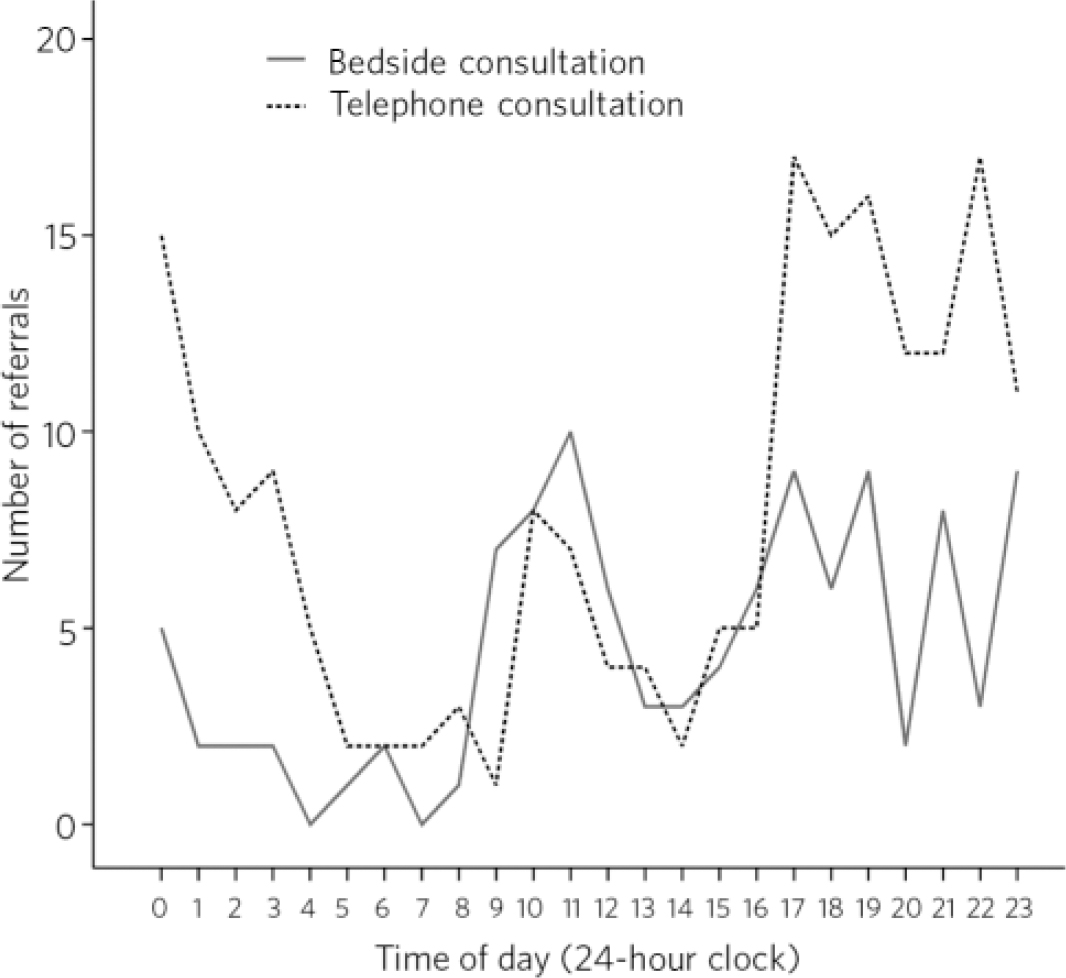
Fig 1 Diurnal variation in referrals to out-of-hours services in child and adolescent psychiatry.
Of the 205 referrals leading to a telephone consultation, 167 (81.5%) could be dealt with in less than 1 h. However, when trainee doctors had to go into the hospital to undertake a bedside assessment (n = 118), they spent more than 4 h on dealing with the referral for 60 (50.5%) individuals and for 16 (13.6%) it took more than 6 h.
The proportion of referrals considered appropriate by the trainee doctors was 79.0% and when only bedside assessments were considered this proportion rose to 89.8%. After changes were made to the referral protocol there was an increase in appropriate and decrease in inappropriate referrals at all three sites. Accordingly, when the proportion of appropriate referrals before and after the protocol changes were compared, a pooled odds ratio of 3.9 (95% CI 2.2-7.1) was obtained.
Table 2 provides information about how variables dependent on organisation of the service and those independent from it related to the referral rate. The presence or absence of daytime liaison cover and protocol changes showed a significant association with both the referral rate for bedside consultation and telephone and bedside consultation combined. The proportion of referrals leading to a bedside assessment was significantly higher on days without daytime cover (48%) than on those with cover (29%, P = 0.001). Data pertaining to service-dependent factors are given as pooled odds ratios since there were no significant differences over strata. Of the service-independent variables, only season reached significance and there were more referrals in spring than the rest of the year.
Table 2 Odds ratios for receiving referrals according to whether or not the examined service-dependent or service-independent factors were present
| Odds ratio (95% CI) | ||
|---|---|---|
| Bedside assessment and telephone consultation combined | Bedside assessment only | |
| Service-dependent factorsa | ||
| No daytime cover | 1.46 (1.15–1.87) | 2.32 (1.60–3.43) |
| High A&E workload | 1.05 (0.72–1.53 | 1.30 (0.82–2.06) |
| 4-hour A&E time target introduced | 1.00 (0.69–1.44) | 0.83 (0.56–1.21) |
| Senior house officer changeover | 1.14 (0.78–1.65) | 1.47 (0.76–2.87) |
| Protocol changes | 2.33 (1.92–3.23) | 2.08 (1.41–3.23) |
| Service-independent factors | ||
| School holidays | 0.97 (0.72–1.30) | 1.50 (0.75–1.43) |
| Spring | 1.50 (1.14–1.98) | 2.03 (1.34–3.09) |
| Hot day > 20°C | 1.47 (0.97–2.23) | 0.92 (0.44–1.86) |
| Rainy day > 4 mm | 1.22 (0.82–1.80) | 0.89 (0.46–1.71) |
Discussion
The present study set out to identify peaks and troughs in the workload of out-of-hours services in child and adolescent psychiatry covering three inner-city teaching hospitals. Our data can help with service-planning and lead to a better understanding of the precipitants of paediatric psychiatric emergencies. The results show such out-of-hours services should expect around 22 referrals per 100 000 population per year. Demand for provision outside normal working hours was at its greatest over weekends and between 17.00 h and 00.59 h on weekdays, which is in keeping with other studies focusing mainly on adults. Reference Bergen and Hawton14,Reference Bergen and Hawton15 In the majority of cases a telephone consultation to the attending paediatrician or psychiatric senior house officer was sufficient to draw up a management plan until the young person could be assessed by the regular daytime liaison team. On days without normal daytime cover, young people still required specialist mental health assessments and hence the peak in referrals between 09.00 h and 12.59 h and the higher proportion of bedside assessments on those days. In a significant proportion of cases (23%) the bedside assessment could not be delayed until the next morning and the on-call child and adolescent psychiatrist had to see the young person between 17.00 h and 09.00 h.
Nearly half of all referrals concerned young people aged 16 and over. This means that widening access to child and adolescent mental health services to include this age group, as required in England, is associated with a considerable increase in workload with resource implications. 8 Many paediatric wards with a high proportion of babies and very young children are not an adequate environment for older adolescents. Paediatricians and mental health professionals not used to dealing with older adolescents might need additional training and support when they are expected to provide services to this group. The present study also revealed paediatric psychiatric emergencies can be time consuming, with over half of bedside assessments taking over 4 h. Part of the reason for this lies in the complex nature of the work and difficulties with gathering relevant information after normal working hours. 6 However, difficulties over arranging in-patient admission were, as elsewhere in the UK, one of the most frequent causes for delay in the catchment area studied. Reference Hakko, Rasanen, Tiihonen and Nieminen19
Previous research has demonstrated how service design and planning can influence how effectively out-of-hours services in child psychiatry are used. Reference Worrall, O'Herlihy, Banerjee, Jaffa, Lelliott and Hill20 The present study showed an overall increase in referrals and simultaneous decrease in inappropriate referrals after clarification of referral pathways and criteria. Specifying that referrals should come from paediatricians or trainee psychiatrists proved a particularly effective measure. It should be acknowledged that the rating of the appropriateness of referrals was based on the judgement of the recipient of the referral. Other service-dependent factors examined in this study were not associated with how the out-of-hours service was used and how many referrals it received. For example, we had hypothesised that there would be more referrals when A&E had a high workload, when the NHS 4-hour waiting time target was introduced or junior doctors rotated jobs. However, none of these factors showed a significant association with the referral rate.
Large epidemiological studies have shown cyclic variations in psychiatric emergencies depending on season, weather or holidays. Reference Rushton, Bruckman and Kelleher13,Reference Bergen and Hawton15,Reference Blenkiron16,Reference Parker, Roberts, Williams, Benjamin, Cripps and Woogh21 This study analysed whether these factors would also be reflected in the referral pattern to out-of-hours service in child and adolescent psychiatry. The results showed no more referrals than usual during the holidays or when it was hot or rainy. However, there were 50% more referrals during spring than the rest of the year. This by far exceeds the seasonal fluctuations observed in other studies. One possible explanation is that many students in the UK sit important exams or experience other disruptions to their school life during spring (for example, 16-year-olds are on their last term of compulsory education). School stress has previously been linked to self-harm. Reference Eastwood and Stiasny22 However, the spring excess in referrals was not confined to those age groups most affected by the school situation. If the relatively large excess in referrals of young people in crisis during spring is replicated in further studies, it would be important to understand the reasons behind it better and to take this into account for service planning.
The methodological strengths of this study include the prospective data collection, the inclusion of three different sites/hospitals, the large sample size and diversity of the underlying population and the long period of observation. One of the limitations of the study was the use of only one source, the trainee doctors, for case ascertainment. When trainee doctors failed to record a referral when on call, the case was missed. The three hospitals did not have very well-defined catchment areas and this may have distorted the estimate of demand per 100 000 general population. Generalisations from our data to other services might be difficult since the study was solely based on an inner-city population and services in other parts of the country may have a different configuration. Reference Bennewith, Gunnell, Peteres, Hawton and House10,Reference Hawton, Bergen, Cassey, Simkin, Plamer and Cooper12 Our study only recorded the day and time when the out-of-hours service received the referral and there was no information as to when the young person arrived at A&E or when the crisis (e.g. taking an overdose) started. This made comparison with some studies, which had this information, more difficult. Furthermore, without multivariate analyses there was no ability to control for confounding factors. Finally, children and young people in need of mental health assessment come to hospital through a variety of pathways such as self-referral and professional referrals by GPs, social workers and school nurses. In the current study the focus was on individuals that had found their way to the hospital and were then referred to the out-of-hours service in child and adolescent psychiatry. Further study into primary referral sources might advance our understanding of pathways, with possible consequences for service configuration and allocation of resources.
This study suggests that although paediatric psychiatric emergencies are relatively rare they can take up considerable clinician time and require input from professionals experienced in this field. Bundling services together to cover large catchment areas could be one way of ensuring that resources for maintaining out-of-hours provision are well used and that the clinicians involved see enough cases to develop the relevant expertise.
Acknowledgements
We particularly want to thank Dr Louise Richards for setting the case registry up when she was a trainee on the Tavistock Rotation. All trainee doctors participating in the on-call rota helped with the collation of the data. Drs S. Lewis, Z. Davis, M. Berelowitz and S. Kraemer reliably offered clinical supervision and kindly helped with editing the manuscript. We are grateful to the Met Office for providing us with the weather data.






eLetters
No eLetters have been published for this article.