Insomnia is a type of sleep disorder that is characterised by difficulty in sleep initiation or maintenance at night and is usually accompanied by daytime symptoms such as fatigue, sleepiness, irritability and loss of concentration(Reference Buysse1). Transient insomnia occurs at a rate of approximately 30 % among adults,(Reference Saddichha2) while chronic insomnia is reported in approximately ~10–30 % of adults and more common in those who are divorced or widowed, elderly, female or suffer from psychiatric or medical diseases(Reference Saddichha2,Reference Bhaskar, Hemavathy and Prasad3) . Chronic insomnia may adversely affect daily functioning and if prolonged may be associated with increased risk of deleterious health conditions including obesity, diabetes mellitus, hypertension and other CVD(Reference Javaheri and Redline4,Reference Mesarwi, Polak and Jun5) .
There is evidence to suggest that increased dietary Ca intake, which is mainly obtained from dairy products(Reference Rozenberg, Body and Bruyere6), is associated with improved quality of sleep and reduced insomnia(Reference Grandner, Jackson and Gerstner7,Reference Nisar, Mohammad and Arshad8) . Total plasma Ca was found to be directly related to sleep as a diurnal variation in its concentration was detected during normal sleep(Reference Ridefelt, Axelsson and Larsson9). In addition, brain Ca is proposed to have a role in regulating the duration of sleep in mammals(Reference Tatsuki, Sunagawa and Shi10). The effect of dairy products on sleep could also be due to their content of tryptophan,(Reference Kitano, Tsunoda and Tsuji11) as Ca is involved in producing melatonin, the sleep-inducing neurosecretory hormone, from tryptophan in the brain(Reference Nisar, Mohammad and Arshad8).
Because Ca is necessary for proper musculoskeletal function(Reference Harvey, Biver and Kaufman12), low plasma Ca levels are usually associated with paresthesia in extremities, fatigue and muscle cramps and spasms that can be very painful(Reference Schafer, Shoback, Feingold, Anawalt and Boyce13). These symptoms may lead to some psychiatric conditions including anxiety and depression, which can also be present due to hypocalcaemia itself(Reference Schafer, Shoback, Feingold, Anawalt and Boyce13). Our previous work showed independent associations between non-cardiac musculoskeletal pain (MSP) and anxiety, as well as between anxiety and low dietary Ca intake, suggesting that anxiety and MSP could be associated with low plasma Ca levels(Reference Alkhatatbeh, Abdul-Razzak and Amara14). MSP may also be associated with insomnia and the two conditions could co-occur with each of them increasing the risk of the other(Reference Baker, McBeth and Chew-Graham15). In addition, several studies have reported a high co-morbidity between insomnia, anxiety and depression(Reference Khurshid16–Reference Oh, Kim and Na19).
The aim of the current study was to assess dairy Ca intake and its relationship to insomnia and other common co-morbidities including anxiety, depression and MSP in Jordanian university students whose academic achievement is often negatively impacted by these conditions. In Jordan, dietary Ca is mainly obtained from dairy products that are available in the Jordanian market including cheese, yogurt, milk and labanah. These types of food are very popular and rich in Ca(Reference Alkhatatbeh, Abdul-Razzak and Amara14,Reference Abdul-Razzak, Obeidat and Al-Farras20) . We hypothesised that low dairy Ca intake is highly prevalent in this population and is associated with insomnia, anxiety, depression and MSP. Understanding the relationship between Ca intake and these common ailments may be effective in improving insomnia and psychological symptoms in the study population.
Materials and methods
Study design and participants
A single institution questionnaire-based cross-sectional study was conducted between September 2019 and January 2020 at Jordan University of Science and Technology, Irbid, Jordan. The study sample consisted of 1000 enrolled undergraduate students recruited from all schools of the university. Participants were divided into two groups: ‘medical students’ who were specialising in medicine, dentistry, pharmacy, nursing or applied medical sciences and ‘non-medical students’ who were specialising in engineering, computer sciences, science and art, agriculture or architecture and design. The study procedure was ethically approved by the Institutional Review Board of the university. Written informed consent was obtained from all participants before they personally completed the questionnaires. A research assistant was available to clarify any inquiries from the participants.
Data collection
Self-reported data collection included: age, height, weight, marital status, college, academic level, smoking, number of family members, family income, exercise, as well as history of medical illness (including psychological illnesses) and Ca supplementation during the previous month. BMI was calculated from weight and height in kg/m2.
Assessment of daily dairy calcium intake
Participants were asked to report the daily frequency and type of dairy product consumed including cheese, yogurt, milk and labanah as previously described(Reference Alkhatatbeh, Abdul-Razzak and Amara14,Reference Abdul-Razzak, Obeidat and Al-Farras20) . These are the most common dairy products available in the Jordanian market and they represent the major sources of dietary Ca in this population(Reference Alkhatatbeh, Abdul-Razzak and Amara14,Reference Abdul-Razzak, Obeidat and Al-Farras20) . Frequency of dairy intake was defined as 0, 1, 2, 3 or more servings/d,(Reference Alkhatatbeh, Abdul-Razzak and Amara14,Reference Abdul-Razzak, Obeidat and Al-Farras20) where a single serve was defined as: 1 ounce of cream cheese (20 mg Ca), 1 ounce of cheddar cheese (162 mg Ca), one cup (240 ml) of milk or yogurt (300 mg Ca) and two tablespoons (2 oz) of labanah (100 mg Ca)(Reference Alkhatatbeh, Abdul-Razzak and Amara14,Reference Abdul-Razzak, Obeidat and Al-Farras20) . Daily Ca intake was then calculated in mg/d. None of the participants reported intake of Ca supplements.
Assessment of insomnia and its severity
Insomnia was assessed using an Arabic version of the well-validated Insomnia Severity Index (ISI)(Reference Bastien, Vallieres and Morin21) that was previously translated from English to Arabic using the standard forward-backward translation method(Reference Suleiman and Yates22). The Arabic translation was also pilot tested on thirty undergraduate university students who were not participants in the current study. The ISI is a self-administered seven question survey that measures severity of insomnia experienced over the previous 2 weeks. The first three questions assess the difficulty in falling asleep, difficulty in staying asleep and problems with waking up prematurely. The remaining four questions assess how the subject’s satisfaction with their current sleep pattern, how noticeable it is to others that there may be sleep problem impairing the subject’s quality life, whether the subject is worried about their current sleep pattern and how much the current sleep pattern is interfering with the subject’s daily functioning. Each of these questions is answered by selecting a number from 0 to 4 that describes the severity of the problem and the ISI score (0–28) is calculated by adding the scores of all questions together. Participants with ISI scores from 0 to 7 are considered to have no clinically significant insomnia, participants with ISI scores from 8 to 14 are classified as having subthreshold insomnia and participants with ISI scores from 15 to 28 are considered to have clinical insomnia (moderate to severe).
Assessment of psychological symptoms (anxiety and depression)
Anxiety and depression symptoms were assessed using an Arabic version of the well-validated Hospital Anxiety and Depression Scale (HADS)(Reference Zigmond and Snaith23). The standard forward-backward translation method was also used to translate the HADS from English to Arabic as previously described(Reference Alkhatatbeh, Abdul-Razzak and Amara14). The Arabic translation was also pilot tested on thirty undergraduate university students who were not participants in the current study. The HADS consists of seven questions that assess anxiety and seven questions that assess depression. Each question is answered by selecting a number from 0 to 3 considering to severity. Thus, the total score for both anxiety and depression ranges from 0 to 21. Participants were considered normal (HADS-anxiety or depression scores from 0 to 7), borderline (HADS-anxiety or depression scores from 8 to 10) or abnormal (HADS-anxiety or depression scores from 11 to 21)(Reference Zigmond and Snaith23).
Assessment of musculoskeletal pain
As previously described(Reference Alkhatatbeh, Abdul-Razzak and Khasawneh24), participants were asked to report the sites and severity of chronic MSP. Areas of MSP were indicated using an illustration of the human body consisting of twelve sites including neck, shoulders, lower back, hands, wrists, palms, arms, upper legs, knees, lower legs, hips and feet. The number of painful body sites was summed. Additionally, participants were asked to report the overall intensity of MSP during the last month using a 0–10 numerical rating scale (0 reflects no MSP and 10 reflects the maximum intensity of MSP)(Reference Alkhatatbeh, Abdul-Razzak and Khasawneh24).
Statistical analysis
Analysis was performed using the IBM SPSS Statistics software version 23. Data were presented as frequency (%), mean ± sd or median (25th–75th percentiles) as appropriate. Differences in variables according to insomnia status were determined using one-way ANOVA with Tukey post-hoc test for multiple comparisons, Kruskal–Wallis one-way ANOVA or χ 2 test as appropriate. Correlation analysis between ISI score and other continuous variables was performed using either Pearson’s or Spearman’s correlation test as appropriate. Predictors of insomnia, anxiety and depression were determined using multiple linear regression analysis. Predictors of MSP were determined using binary logistic regression analysis. All P-values were two-tailed and considered statistically significant at < 0·05.
Results
General characteristics of the participants
One thousand participants (36·7 % males and 63·3 % females) were recruited, consisting of 52·4 % medical and 47·6 % non-medical university students, whose mean age was 20·87 ± 2·69 years. According to their academic level, 55·3 % of participants were in their 1st or 2nd year (junior students) and 44·7 % of participants were in their 3rd–6th year (senior students). Participants had a mean BMI of 23·75 ± 4·56 kg/m2 and only 14·7 % of participants were current smokers. Other characteristics of participants are reported in Table 1.
Table 1 Differences between variables according to insomnia status
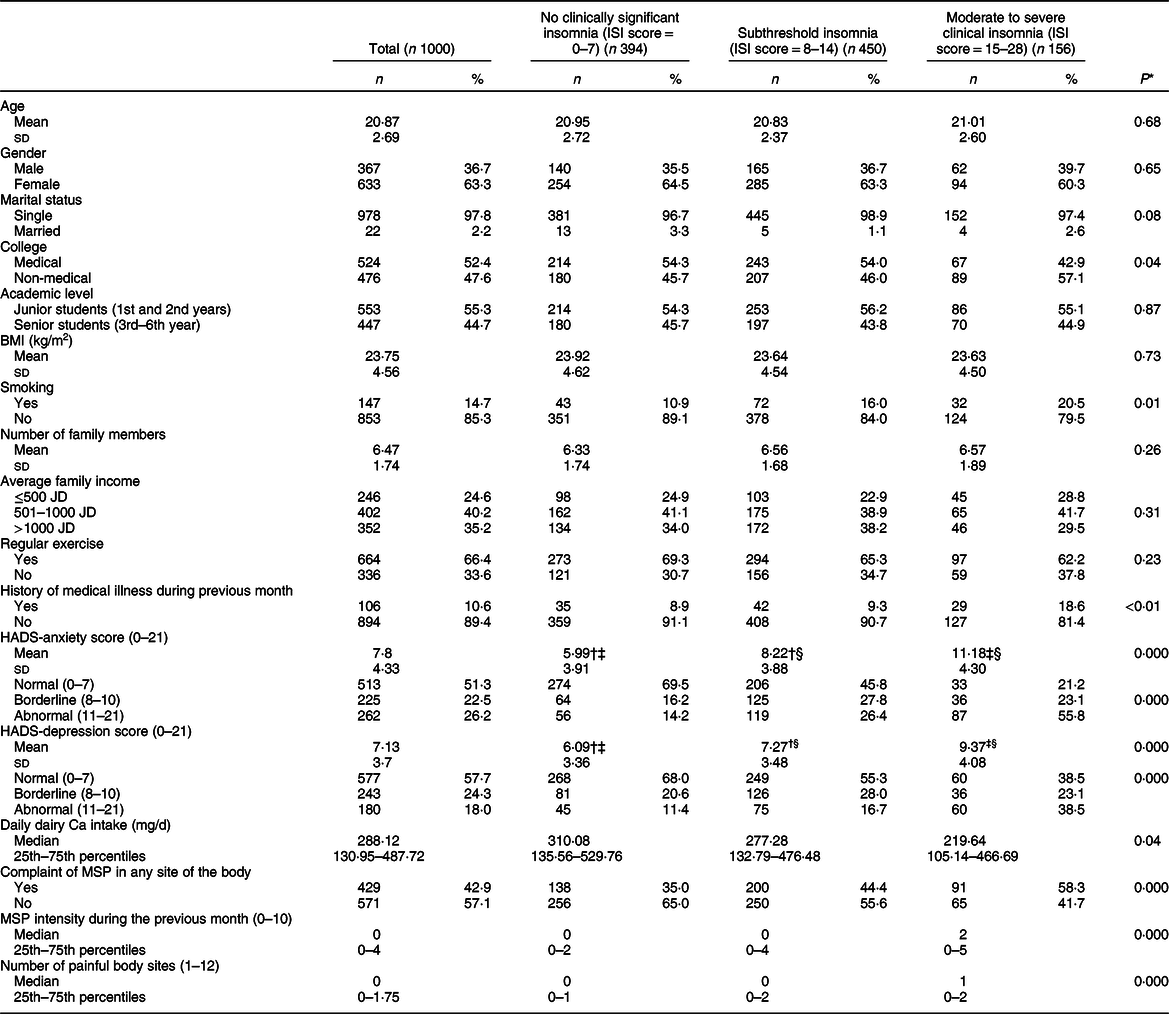
ISI, Insomnia Severity Index; HADS, Hospital Anxiety and Depression Score; MSP, musculoskeletal pain; JD, Jordanian Dinar.
* One-way ANOVA test, Kruskal-Wallis one-way ANOVA or χ 2 test as appropriate (P-values < 0·05 were considered statistically significant). Data are expressed as frequency (%), mean ± sd or median (25th–75th percentiles).
† Post-hoc analysis revealed significant difference between no clinically significant insomnia and subthreshold insomnia.
‡ Post-hoc analysis revealed significant difference between no clinically significant insomnia and moderate to severe insomnia.
§ Post-hoc analysis revealed significant difference between subthreshold insomnia and moderate to severe insomnia.
Daily dairy calcium intake
Most participants (96·5 %) reported a daily dairy Ca intake that was well below the recommended daily intake of 1000 mg/d for adults,(Reference Cormick and Belizan25) with an overall median (25th–75th percentiles) of 288·12 (130·95–487·72) mg/d.
Prevalence of insomnia and its severity
According to the ISI scoring system, 15·6 % of participants suffered from moderate to severe clinical insomnia, 45·0 % of participants had subthreshold insomnia and 39·4 % of participants had no clinically significant insomnia. The mean ISI score for all participants was 9·31 ± 5·46.
Prevalence of psychological symptoms (anxiety and depression)
According to the HADS scoring system, abnormal HADS-anxiety scores were reported in 26·2 % of participants and abnormal HADS-depression scores were reported in 18·0 % of participants. Additionally, 22·5 % of participants recorded borderline HADS-anxiety scores and 24·3 % of participants had borderline HADS-depression scores. The remaining participants had normal HADS-anxiety (51·3 %) and depression (57·7 %) scores. The mean HADS-anxiety and depression scores for all participants were 7·8 ± 4·33 and 7·13 ± 3·7, respectively.
Prevalence of musculoskeletal pain
MSP was reported by 42·9 % of participants. The median (25th–75th percentiles) MSP intensity (out of 10) during the previous month was 0 (0–4) and the median (25th–75th percentiles) number of painful body sites (out of 12) was 0 (0–1·75).
Differences between study variables according to insomnia status
As shown in Table 1, moderate to severe insomnia was more prevalent in non-medical students compared with medical students (P-value = 0·04). Current smokers, participants with a history of medical illness and those who reported MSP during the previous month reported higher frequencies of moderate to severe insomnia compared with subthreshold insomnia and no clinically significant insomnia (P-values = 0·01, <0·01, <0·001, respectively). Participants with moderate to severe insomnia had higher HADS-anxiety and depression scores, higher MSP intensity during the previous month, more painful body sites and lower daily dairy Ca intake compared to participants with subthreshold insomnia and participants with no clinically significant insomnia (P-values < 0·001).
Correlation between Insomnia Severity Index score, Hospital Anxiety and Depression Scale-anxiety and depression scores, musculoskeletal pain and daily dairy calcium intake
As shown in Table 2, there was a relatively strong correlation between the ISI and HADS-anxiety scores (r = 0·43, P-value < 0·001), and moderate correlations between ISI and HADS-depression scores (r = 0·27, P-value < 0·001) as well as between ISI and both MSP intensity during the previous month and number of painful body sites (r = 0·24, P-values < 0·001). In contrast, daily dairy Ca intake was weakly inversely correlated with both ISI score (r = −0·10, P-value <0·01) and HADS-depression score (r = −0·12, P-value < 0·001). HADS-depression score was also moderately correlated with MSP intensity during the previous month (r = 0·24, P-value < 0·001) and with the number of painful body sites (r = 0·23, P-value < 0·001). HADS-anxiety score was also moderately correlated with MSP intensity during the previous month (r = 0·35, P-value < 0·001) and with the number of painful body sites (r = 0·34, P-value < 0·001).
Table 2 Correlation between ISI score and other variables*
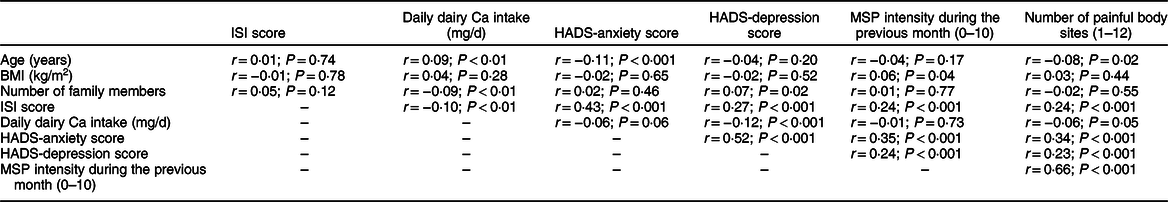
ISI, Insomnia Severity Index; HADS, Hospital Anxiety and Depression Scale; MSP, musculoskeletal pain.
* Pearson’s or Spearman’s correlation test was used as appropriate (P-values were two-tailed and considered statistically significant at < 0·05).
Predictors of insomnia
Multiple linear regression analysis (Table 3) indicated significant associations between ISI score and smoking (P-value = 0·001), HADS-anxiety score (P-value < 0·001), HADS-depression score (P-value = 0·02), complaints of MSP (P-value = 0·04), MSP intensity during the previous month (P-value = 0·02) and the number of painful body sites (P-value = 0·02). In contrast, ISI score was significantly inversely associated with daily dairy Ca intake (P-value = 0·03).
Table 3 Predictors of ISI score*
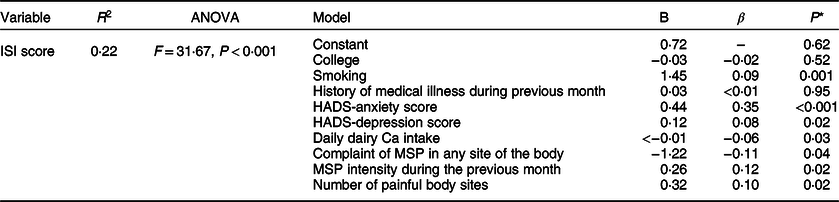
ISI, Insomnia Severity Index; R 2, squared coefficient of determination; B, unstandardised coefficient; β, standardised coefficient; F, F-statistic; HADS, Hospital Anxiety and Depression Score; MSP, musculoskeletal pain.
* Multiple linear regression analysis (P-values < 0·05 were considered statistically significant).
Predictors of psychological symptoms (anxiety and depression)
Multiple linear regression analysis (Table 4) indicated that HADS-anxiety score was significantly inversely associated with participants’ academic level (P = 0·001) and positively associated with female gender (P-value < 0·001), BMI (P-value = 0·02), ISI score (P-value < 0·001) and HADS-depression score (P-value < 0·001). HADS-depression score was also significantly associated with ISI score (P-value = 0·02) and HADS-anxiety score (P-value < 0·001) and was inversely associated with daily dairy Ca intake (P-value < 0·01).
Table 4 Predictors of HADS-anxiety and depression scores
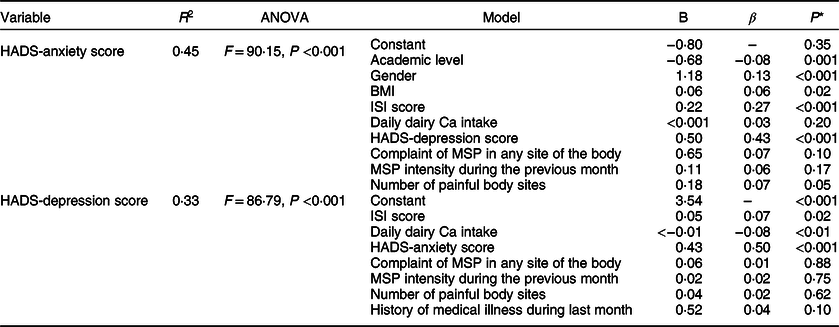
HADS, Hospital Anxiety and Depression Score; ISI, Insomnia Severity Index; R 2, squared coefficient of determination; B, unstandardised coefficient; β, standardised coefficient; F, F-statistic; MSP, musculoskeletal pain.
* Multiple linear regression analysis (P-values < 0·05 were considered statistically significant).
Predictors of musculoskeletal pain
Binary logistic regression analysis (Table 5) revealed that MSP complaints among participants were significantly associated with female gender (OR 1·39, P-value = 0·03), increased BMI (OR 1·04, P-value = 0·02), increased HADS-anxiety score (OR 1·14, P-value < 0·001) and increased ISI score (OR 1·03, P-value < 0·05).
Table 5 Predictors of MSP
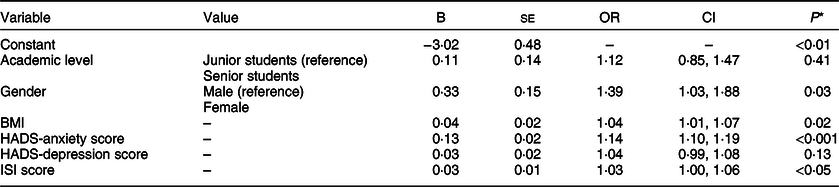
HADS, Hospital Anxiety and Depression Scale; MSP, musculoskeletal pain; ISI, Insomnia Severity Index; B, coefficient (intercept).
* Binary logistic regression (dependent variable: complaint of MSP in any site of the body), P-values < 0·05 were considered statistically significant.
Discussion
The current study reports a high prevalence of inadequate Ca intake estimated from daily food consumption among young adults of around 21 years of age. Of concern, the median dairy Ca intake in our cohort of university students was < 1/3 of the recommended daily intake for adults (1000 mg/d)(Reference Cormick and Belizan25). Low dietary Ca intake in similar age groups has also been reported by other studies using different methods to assess dietary Ca intake(Reference Rouf, Sui and Rangan26,Reference Sandoval, Coelho and Jesus27) . The low dietary Ca intake among young adults could be explained by the wide spread consumption of junk food, especially in universities, that does not contain enough Ca(Reference Lim, Ji and Hwang28). In the present study, only dairy food contributions to Ca intake were estimated and no consideration was given to Ca in other foods such as green leafy vegetables or legumes with lower Ca content and poor bioavailability. Ca is highly available in dairy products(Reference Górska-Warsewicz, Rejman and Laskowski29), and low dietary Ca intake has been linked to deleterious consequences on the skeleton leading to bone diseases such as osteoporosis(Reference Cormick and Belizan25). In addition, low Ca intake could adversely affect other extra-skeletal functions since Ca is involved in muscle contraction, neurotransmission, signalling and other functions(Reference Agrawal, Suryakumar and Rathor30). As such, our hypothesis focused on the relationship between low dairy Ca intake and other inter-related health problems that are commonly manifested in university students including insomnia, anxiety, depression and MSP.
Our major finding was the significant inverse association between insomnia (ISI score) and dairy Ca intake (Table 3). This association suggests that insomnia among university students can be predicted from their low intake of dairy Ca. This finding was also supported by the significant difference in dairy Ca intake between participants with moderate to severe insomnia and participants with no or subthreshold insomnia (Table 1). The relationship between sleep and Ca could partially be explained by the role of brain Ca in converting the amino acid tryptophan to melatonin, which is considered to be a sleep-inducing hormone(Reference Nisar, Mohammad and Arshad8). In addition, previous studies have indicated that Ca could be involved in regulating both cycles and duration of sleep in mammals(Reference Tatsuki, Sunagawa and Shi10). Our results support the increasing evidence that suggests a role for dietary Ca in improving sleep quality and reducing insomnia(Reference Grandner, Jackson and Gerstner7,Reference Nisar, Mohammad and Arshad8) .
Our results have also shown that insomnia among university students can be predicted from anxiety and depression scores, MSP and MSP intensity during the previous month, number of painful body sites and smoking (Table 3). These results were supported by the significant higher anxiety and depression scores in participants with moderate to severe insomnia compared to both participants with no clinically significant insomnia and participants with subthreshold insomnia (Table 1). In addition, a higher percentage of participants who were smokers, and participants with MSP, were classified to have moderate to severe insomnia (Table 1). Moreover, the median MSP intensity and number of painful sites were significantly higher in participants with moderate to severe insomnia compared to both participants with no clinically significant insomnia and participants with subthreshold insomnia (Table 1). The relationship between insomnia and the psychological symptoms of anxiety and depression was previously reported in the literature to be bi-directional(Reference Jansson-Frojmark and Lindblom31,Reference Rutten, Vriend and van der Werf32) . This was also supported by our findings as insomnia (ISI score) was a significant predictor for both anxiety and depression (Table 4) and vice versa (Table 3). This suggests that insomnia among university students may lead to anxiety and depression which in turn may cause insomnia. Insomnia and MSP were also previously reported to co-occur and each of them may increase the risk of the other(Reference Baker, McBeth and Chew-Graham15). Our results also supported this relationship as insomnia was a significant predictor of MSP, while MSP, MSP intensity and number of painful body sites were significant predictors of insomnia (Tables 3 and 5). The last predictor of insomnia in our study was cigarette smoking. It has been reported that sleep disturbances are more common in cigarette smokers compared with non-smokers(Reference Liao, Xie and Chen33). This is explained by the stimulant action of nicotine that can increase alertness(Reference Caviness, Anderson and Stein34), which may result in insomnia.
One of the main objectives of the current study was to find a link between low dietary Ca estimated from dairy food consumption and insomnia, anxiety, depression and MSP, as we believe that low Ca intake may contribute to the development of these conditions. Our results have shown that dairy Ca intake was inversely associated with insomnia and depression scores but not associated with anxiety scores and complaints of MSP (Tables 3, 4 and 5). These results are not completely consistent with our previous study which was conducted on subjects with non-cardiac musculoskeletal chest pain(Reference Alkhatatbeh, Abdul-Razzak and Amara14). In that study, low dairy Ca intake was associated with anxiety, and anxiety was associated with pain. This inconsistency may be explained by differences in the study design and age of participants(Reference Alkhatatbeh, Abdul-Razzak and Amara14). Because participants of the current study were younger and apparently healthy, their low dairy Ca intake may not result in musculoskeletal symptoms. Although there was no significant association between dairy Ca intake and anxiety or MSP, our results suggested an indirect relationship between them. The current study results indicate that anxiety may be affected by low dairy Ca intake through the significant association between anxiety and both insomnia and depression scores, which themselves are associated with low dairy Ca intake. Similarly, MSP may be affected by low dairy Ca intake through the significant association between MSP and insomnia scores, the latter of which is associated with low dairy Ca intake. Therefore, our results maintain support for the presence of a relationship between low dairy Ca intake, insomnia, anxiety, depression and MSP in our study population.
Taken together, the current study has exposed a relationship between low dairy Ca intake and medical conditions including insomnia, anxiety, depression and MSP, all of which are commonly present in university students. The main strengths of the current study were its large sample size and the established methods used to measure the variables of interest. All outcomes were determined using well-validated surveys that have been previously documented in the literature (refer to Materials and methods). The study was mainly limited by its cross-sectional design and the dependence on participants’ reliable self-reporting. The study is also limited by the incomplete estimate of total dietary Ca intake, which only included dairy food sources and not that of other foods and beverages with lower Ca content and often poor bioavailability. Dairy foods are the most commonly consumed Ca-rich foods by Jordanian students with highly available Ca. These limitations may prevent us from making conclusions that can be applied to the general population. However, we believe these results are reported for the first time and hope they may encourage other researchers to further investigate the potential causal relationship between low dietary Ca intake and insomnia, anxiety, depression and MSP. If proven true, further studies should be performed to determine if increasing dietary Ca intake, either via food choices or supplementation, is able to resolve some of these health issues among university students in order to increase both their lifestyle and scientific achievements.
Conclusion
Low dietary Ca intake estimated from dairy food consumption was highly prevalent and associated with insomnia and depression among university students from Jordan. Insomnia in our study participants could be predicted from increased anxiety and depression scores, complaint of MSP and smoking. Both anxiety and depression scores could also be predicted from insomnia scores, supporting a bi-directional association for both anxiety and depression with insomnia. Young adults should be advised to increase dietary Ca intake to achieve the recommended daily amount. It is also required to investigate a potential causal relationship between low dietary Ca and both insomnia and its related co-morbidities.
Acknowledgements
Acknowledgements: The authors would like to thank all individuals who participated in this study. Financial support: This work was financially supported by the Deanship of Research, Jordan University for Science and Technology under Grant (number: 20190367). Conflict of interest: None. Authorship: M.J.A. was responsible for study design, statistical analysis and manuscript writing. H.N.K. was responsible for data collection. K.K.A. was responsible for results interpretation and manuscript editing. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Institutional Review Board (IRB) of Jordan University of Science and Technology, Irbid, Jordan. Written informed consent was obtained from all subjects.







