With global ageing population demographics, the prevalence of cognitive disorders has surged(Reference Nichols, Szoeke and Vollset1). The number of individuals living with dementia, which is a major cause of loss of independence and disability in older age, has doubled between 1990 and 2016, reaching 50 million worldwide(Reference Nichols, Szoeke and Vollset1). In the UK, dementia is now the number one cause of death, responsible for about 15 % of all-cause mortality(2). Besides, dementia has an enormous economic burden, with the global cost expected to reach $2 trillion by 2030(Reference Prince, Wimo and Guerchet3).
The prevalence of mild cognitive impairment, the transition phase prior to incident dementia, has been estimated to occur in 15–20 % of the population aged over 60 years, with 8 %–15 % progressing to dementia per year(Reference Petersen4). Subjective memory complaints (SMC), which are loosely defined as a state in which individuals present with ‘self-reported’ cognitive decline relative to their previous cognitive status (which is not diagnosed by objective standard tests), occur in 50–80 % of individuals aged 70 years or older(Reference Jessen, Amariglio and Buckley5). SMC is linked to depression, anxiety and future Alzheimer’s disease risk(Reference Jessen, Amariglio and Buckley5,Reference Jessen, Amariglio and van Boxtel6) . In addition to cognitive decline, mental disorders, including depression and anxiety disorders, are prevalent, occurring in 3–5 % of the global population(7), and are one of the top three causes of non-fatal health loss in terms of years lived with disability(Reference James, Abate and Abate8). Depression is also a risk factor for future dementia(Reference Livingston, Sommerlad and Orgeta9).
Currently, Alzheimer’s disease and other dementias are irreversible with no effective treatments available to slow or reverse the condition. Therefore, behaviours (such as altered eating behaviour and nutrition status) which can prevent or delay progression of these conditions have the potential to dramatically reduce both individual risk and the population burden of the disease(Reference Jennings, Cunnane and Minihane10). A Mediterranean-style dietary pattern (MDP) is emerging as having potential positive effects on mental health status. The diet is characterised by high consumption of extra virgin olive oil (EVOO) and plant-based foods such as fruits, vegetables, nuts, legumes, whole-grain cereals; low to moderate consumption of dairy products mainly yoghurt and cheese; fish consumed two to four times a week; low amounts of red meat and moderate consumption of red wine mainly with meals(Reference Willett, Sacks and Trichopoulou11). EVOO, in addition to being the major component of a MDP, has been shown to independently confer neuropsychiatric and cardiovascular benefits(Reference Visioli, Franco and Toledo12), attributed to its high monounsaturated fatty acids (MUFA) and phenolic content(Reference Gorzynik-Debicka, Przychodzen and Cappello13).
The cardiometabolic health benefits of a MDP, first reported in the Seven Countries Study in the 1950s(Reference Kromhout, Menotti and Bloemberg14), are now well established(Reference Bendall, Mayr and Opie15–Reference de Lorgeril, Salen and Martin17). An improved cardiometabolic phenotype is thought to in part underlie the emerging cognitive benefits of this dietary pattern. However, the majority of this evidence has been acquired from observational studies, such as European Prospective Investigation into Cancer-Norfolk(Reference Shannon, Stephan and Granic18), with a dearth of randomised controlled trials (RCT) which report on the causal benefits of a MDP on long-term cognitive and overall mental health. The Prevencion con Dieta Mediterranea (PREDIMED) was the first RCT testing the long-term effectiveness of a MDP in primary prevention which had incidence of CVD as the primary point(Reference Martínez-González, Corella and Salas-Salvadó19). In a sub-group secondary analysis, the MDP interventions enriched with either EVOO or nuts were shown to improve cognitive function(Reference Martinez-Lapiscina, Clavero and Toledo20) and depressive symptoms(Reference Sanchez-Villegas, Martinez-Gonzalez and Estruch21). Available systematic reviews and meta-analysis focus on the long-term mental health benefits of a MDP, with adherence associated with an overall risk ratio of 0·79 (95 % CI 0·70, 0·90) of developing cognitive disorders(Reference Wu and Sun22). Although no association was observed in the cohort analysis, data from nine cross-sectional studies indicate a negative relationship between adherence to a MDP and risk of depression (OR = 0·72; 95 % CI 0·60, 0·87)(Reference Shafiei, Salari-Moghaddam and Larijani23).
In addition to the long-term trajectory, for the ever-increasing number of individuals with pre-existing cognitive or mental health deficits and even in healthy individuals, there is a great need and interest in identifying nutrition strategies which improve cognition, mood and anxiety in the short-term, in order to improve capabilities, independence and overall quality of life. Therefore, the objectives of the current systematic review are, (i) to conduct an evidence synthesis from RCT data to scrutinise whether a MDP has the potential to alter cognition, mood and mental well-being in the short-term and (ii) identify research need and inform the design of future acute RCT in the area.
Methods
This systematic review was written in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines(Reference Liberati, Altman and Tetzlaff24). Our systematic review protocol is available on PROSPERO with the registration number CRD42021221085(Reference Esgunoglu, Jennings and Murphy25).
Search strategy, eligibility criteria and study selection
‘Short-term’ is defined as ‘up to 10 days’ by discussions among the authors, where effects on cognition are likely to be mediated by rapidly responsive physiological processes such as brain blood flow, inflammation and oxidative status. Ovid Emabse, Ovid MEDLINE and Web of Science Core Collection were searched(Reference Bramer, Rethlefsen and Kleijnen26,Reference Gusenbauer and Haddaway27) from their inception dates to 8 December 2020 by using keywords covering ‘Mediterranean diet’, ‘olive oil’, ‘cognition’, ‘dementia’, ‘mood’, ‘mood disorders’, ‘anxiety’, ‘anxiety disorders’, ‘depression’, ‘depressive disorders’ and ‘wellbeing’. Free search terms and medical subject heading terms were combined where the databases allowed, namely Embase and MEDLINE. Final search strategies were constructed with the assistances of an expert in systematic reviews in Norwich Medical School, and the academic librarian of the Faculty of Medicine and Health Sciences, University of East Anglia. The full electronic search string used in Ovid Embase is presented in Appendix 1.
Studies were accepted eligible if they,
-
- had an RCT design,
-
- intervened with either a MDP or EVOO,
-
- had an intervention period of up to and including 10 d,
-
- assessed either cognition, mood, anxiety or depression as a primary or secondary endpoint,
-
- included adults over 18 years and
-
- published in the English language.
Observational epidemiological studies were excluded. No sex filter was applied. The reference lists of included studies were manually read in order to obtain further potential publications. Two authors (L. E. and E. S. C.) independently completed screening the titles and abstracts against the predefined eligibility criteria. Any discrepancies were resolved by discussions until an agreement was reached. EndNote X9 is used as the reference management tool.
Definition of cognitive and mental health as the primary outcomes
Cognition is defined as ‘the mental action or process of acquiring knowledge and understanding through thought, experience and the senses’(28). Memory, attention, reasoning, decision-making, visual and spatial abilities and behaviours are examples of ‘cognitive functions’. Depression and anxiety are significant mood disorders; however, mild to moderate level of psychological stress can also cause substantial reductions in the quality of life. A variety of validated tools are available to assess cognition and mood, with details of the tools used in individual studies detailed below and in Table 1.
Table 1. Study details and main outcomes
(Mean values and standard deviations)
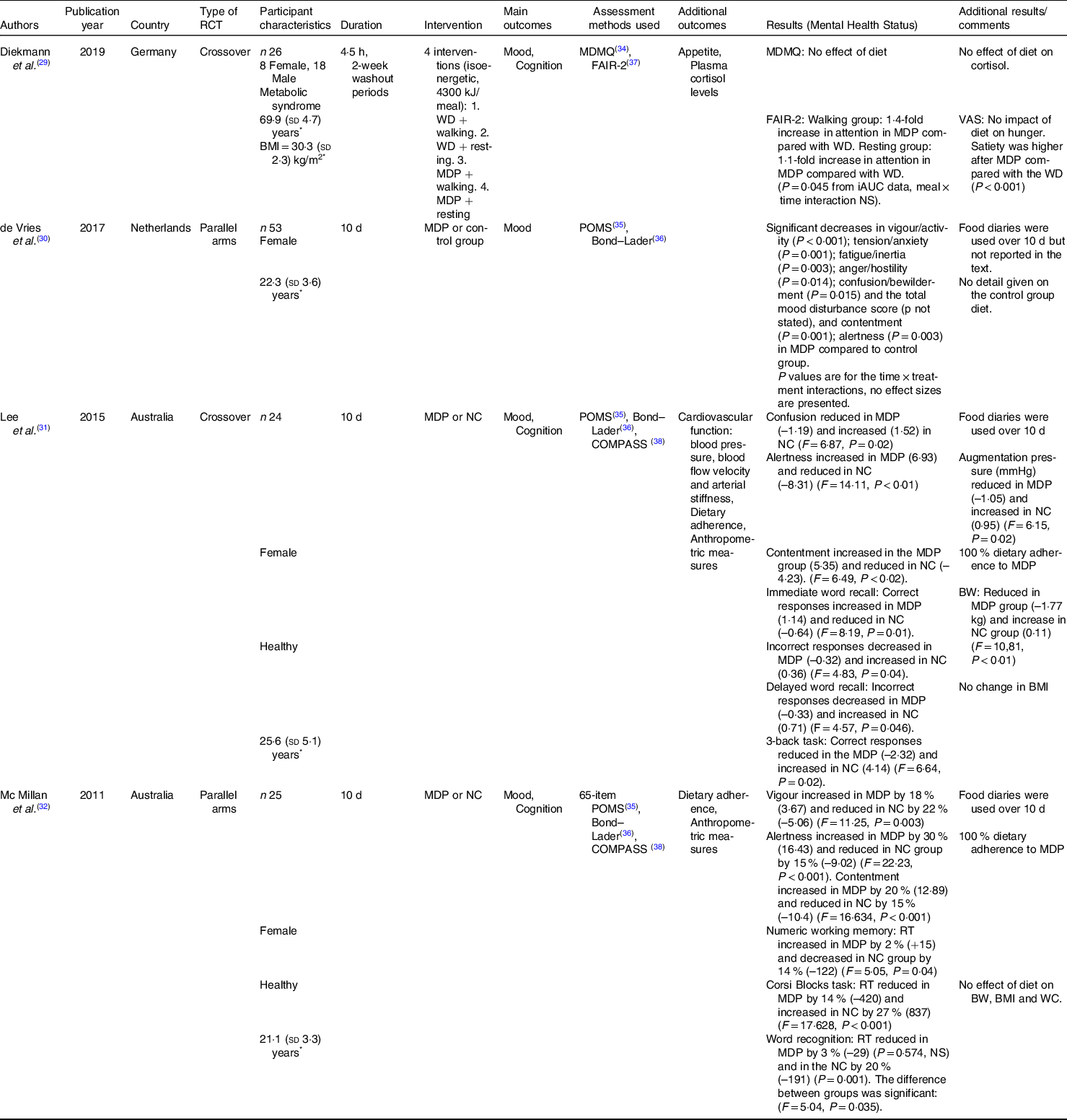
RCT, randomised controlled trial; WD, Western diet that is rich in total fat, SFA, saturated fatty acids; and animal protein; MDP, Mediterranean-style dietary pattern; MDMQ, Multidimensional Mood State Questionnaire for mood; FAIR-2, Frankfurt Attention Inventory-2 for cognition; iAUC: AUC, area under the curve; VAS, Visual Analogue Scale for hunger, appetite and satiety; POMS, Profile of Mood States questionnaire for mood (tension/anxiety, anger/hostility, fatigue/inertia, vigour/activity, confusion/bewilderment, depression/rejection and total mood disturbance score); Bond–Lader Scale for mood (alertness, contentment and calmness); NC, No change in diet; COMPASS, The Computerised Mental Performance Assessment System for cognitive domains; RT, reaction time; BW, body weight; WC, waist circumference.
* Represents mean and standard deviation unless otherwise stated.
Data extraction and quality assessment
A table which recorded the authors, publication year, country where studies were conducted in, type of RCT, participant characteristics, study duration, intervention, main outcomes, assessment methods used, results (mental health status) and additional results/comments was generated to extract the data from the included studies.
A quality assessment was done using RoB2, a revised tool for risk of bias by Cochrane(Reference Sterne, Savović and Page29), which has five domains: bias arising from the randomisation process (D1), bias due to deviations from intended interventions (D2), bias due to missing outcome data (D3), bias in measurement of the outcome (D4), bias in selection of the reported result (D5) and plus overall bias (D6). The results of bias investigation are presented by means of a traffic light plot under low risk, some concerns or high risk.
Data synthesis
A narrative approach was used to synthesise the data. No quantitative analysis was performed due to the small number of studies.
Results
Study identification
Initially, 3002 studies were obtained from the three electronic databases. After deduplication, 2261 studies remained, with 1721 from the MDP search and 540 from the EVOO search. Of these, 2253 were excluded following the title and abstract screening for reasons such as longer study durations, irrelevant outcomes, supplement interventions, epidemiological studies, animal studies, any type of reviews, meta-analysis and protocols. Full texts were screened for the remaining eight studies. Finally, four studies, three full articles(Reference McMillan, Owen and Kras30–Reference Lee, Pase and Pipingas32) and one conference proceeding(Reference De Vries, Van Schrojenstein Lantman and Hoebregts33), met the eligibility criteria and were included. These four papers yielded a reference list of eighty-five, which were scanned manually by LE and ESC, with no additional publications emerging for inclusion. The study identification process is presented in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram (Fig. 1).
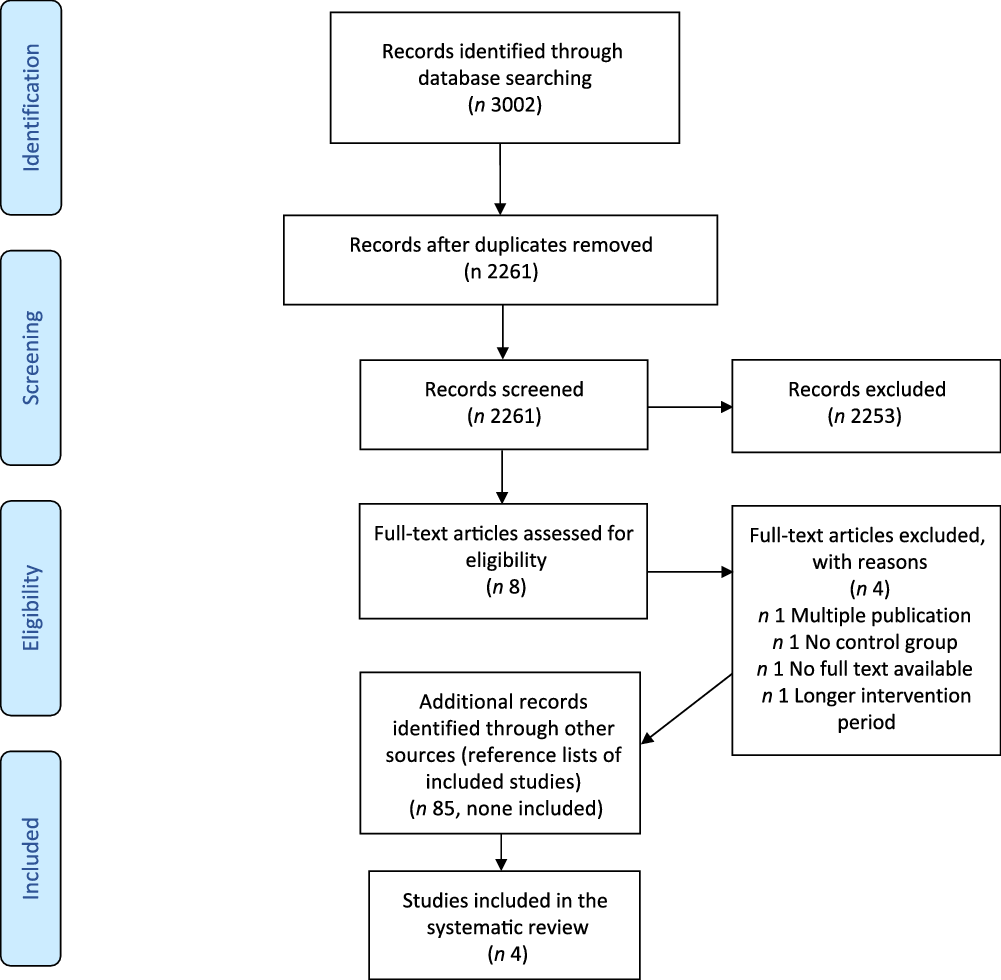
Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
Study characteristics
All included studies were RCT, two with a crossover(Reference Diekmann, Wagner and Huber31,Reference Lee, Pase and Pipingas32) and two with a parallel design(Reference McMillan, Owen and Kras30,Reference De Vries, Van Schrojenstein Lantman and Hoebregts33) . All intervened with a MDP and were carried out in non-Mediterranean countries, two Northern European(Reference Diekmann, Wagner and Huber31,Reference De Vries, Van Schrojenstein Lantman and Hoebregts33) and two Australian(Reference McMillan, Owen and Kras30,Reference Lee, Pase and Pipingas32) . The sample sizes ranged from 24(Reference Lee, Pase and Pipingas32) to 53(Reference De Vries, Van Schrojenstein Lantman and Hoebregts33). Three of the studies included young females only, with mean ages of 21·1 (sd 3·3)(Reference McMillan, Owen and Kras30), 22·3 (sd 3·7)(Reference De Vries, Van Schrojenstein Lantman and Hoebregts33) and 25·6 (sd 5·2)(Reference Lee, Pase and Pipingas32) years. The remaining study(Reference Diekmann, Wagner and Huber31) included both males and females with metabolic syndrome traits with a participant mean age of 70 (sd 5) years. None of the four RCT reported any previous cognitive or mental health issues in the participants. Three had a study duration of 10 d, with one(Reference Diekmann, Wagner and Huber31) examining the physiological response 4·5 h after the test meal. One study(Reference Diekmann, Wagner and Huber31) implemented a MDP alone or with a physical activity intervention (30 min moderate walking).
In terms of the MDP intervention, in one crossover study(Reference Diekmann, Wagner and Huber31), participants were provided with their test breakfast (4300 kJ) that consisted of ciabatta, smoked salmon, muesli, fruit and vegetables which was described as rich in unsaturated fatty acids, dietary fibre and antioxidative compounds. The remaining three studies did not provide the study foods but rather guided participants in following a MDP. De Vries et al. (Reference De Vries, Van Schrojenstein Lantman and Hoebregts33) did not provide any detail of the dietary instructions provided to participants. Lee et al. (Reference Lee, Pase and Pipingas32) requested participants in the MDP group to increase their intake of fruit, vegetables, oily fish, low-fat dairy products and nuts with a focus on healthy carbohydrates, fats and proteins, and to exclude meat, butter, margarine, caffeinated/energy drinks, added sugars and salts, alcohol, tobacco and illicit drugs during the study period. Besides, participants were also asked to consume freshly prepared foods and to avoid processed and packaged options where possible. Similarly, McMillan et al. (Reference McMillan, Owen and Kras30) asked participants to increase their consumption of fruits, vegetables, oily fish, low-fat dairy products and nuts and to combine good sources of carbohydrates (less refined carbohydrates, whole grains, legumes, fruits and vegetables), fats and proteins. Additionally, they were instructed to abstain from red meat, refined sugars, refined flour, pre-packaged and processed foods, caffeinated products, soft drinks and condiments.
Regarding dietary assessment methods, food diaries were used over the 10-d study period in order to record the dietary intake in three of the studies(Reference McMillan, Owen and Kras30,Reference Lee, Pase and Pipingas32,Reference De Vries, Van Schrojenstein Lantman and Hoebregts33) . The remaining study provided the foods, so no self-reported dietary assessment was required(Reference Diekmann, Wagner and Huber31).
While three studies examined both mood and cognition as outcomes(Reference McMillan, Owen and Kras30–Reference Lee, Pase and Pipingas32), one study assessed only mood(Reference De Vries, Van Schrojenstein Lantman and Hoebregts33). The assessment methods for mood included the German version of Multidimensional Mood State Questionnaire(Reference Steyer, Schwenkmezger and Notz34) for subjective mood (good/bad mood; alertness/fatigue and ease/unease)(Reference Diekmann, Wagner and Huber31), the Profiles of Mood States questionnaires(Reference McNair, Lorr and Droppleman35) scoring the subscales tension/anxiety, fatigue/inertia, vigour/activity, confusion/bewilderment, anger/hostility, depression/rejection and the total mood disturbance score(Reference McMillan, Owen and Kras30,Reference Lee, Pase and Pipingas32,Reference De Vries, Van Schrojenstein Lantman and Hoebregts33) and the Bond–Lader visual analogue scales(Reference Bond and Lader36) for the alertness, calmness and contentment(Reference McMillan, Owen and Kras30,Reference Lee, Pase and Pipingas32,Reference De Vries, Van Schrojenstein Lantman and Hoebregts33) . For the assessment of cognition, the German version of the Frankfurt Attention Inventory 2 (test version A)(Reference Petermann37) for attention(Reference Diekmann, Wagner and Huber31) and the Computerised Mental Performance Assessment System(Reference Scholey, Ossoukhova and Owen38) battery for a variety of cognitive domains were used(Reference McMillan, Owen and Kras30,Reference Lee, Pase and Pipingas32) (Table 1).
Study quality
The study quality assessment showed that all included studies have a low risk of bias in the first three domains ((D1), bias arising from the randomisation process; (D2) bias due to deviations from intended interventions; (D3), bias due to missing outcome data), while the other two domains ((D4) bias in measurement of the outcome and (D5) bias in selection of the reported result) were assessed as having some concerns (Fig. 2).
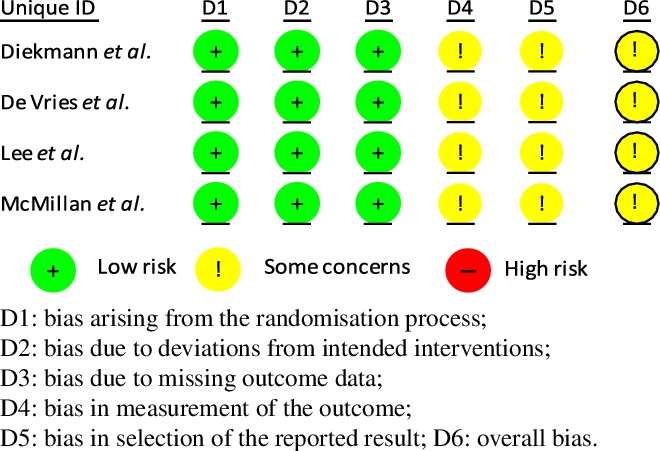
Fig. 2. Risk of bias assessment results.
Primary outcome measures
Cognition
According to the Computerised Mental Performance Assessment System results, increased correct responses (1·14, F = 8·19, P = 0·01) and decreased incorrect responses (–0·32, F = 4·83, P = 0·04) were seen in immediate word recall; reduced incorrect responses (–0·33, F = 4·57, P = 0·046) in delayed word recall were evident in the MDP group relative to the control, while correct responses significantly decreased in MDP treatment (–2·32, F = 6·64, P = 0·02) for the three-back task(Reference Lee, Pase and Pipingas32). Reaction time increased for numeric working memory task in MDP by 2 % and decreased by 14 % in the control group (F = 5·05, P = 0·04); reduced for Corsi Blocks task by 14 % (–420) in MDP treatment and increased by 27 % (+837) in the control group (F = 17·628, P < 0·001)(Reference McMillan, Owen and Kras30). Whilst reaction times reduced in the word recognition task in both arms, it was not significant in the MDP (3 %, –29, P = 0·574) treatment and significant in the control group (20 %, –191, P = 0·001). The difference between the groups was significant (F = 5·04, P = 0·035)(Reference McMillan, Owen and Kras30).
No overall significant effect of meal type in attention (as assessed by the Frankfurt Attention Inventory 2 method) was recorded. However, in the walking groups, a 1·4-fold increase was seen in the MDP group when compared with the WD, while this increase was 1·1-fold higher in the MDP relative to the WD in resting (P = 0·045 from iAUC data)(Reference Diekmann, Wagner and Huber31).
Mood
Using the Profiles of Mood States questionnaire, vigour/activity (P < 0·001), tension/anxiety (P = 0·001), fatigue/inertia (P = 0·003), anger/hostility (P = 0·014), confusion/bewilderment (P = 0·015) and the total mood disturbance score (P value not stated) were significantly improved in the MDP arm compared with the control group(Reference De Vries, Van Schrojenstein Lantman and Hoebregts33). Lowered confusion was observed by the MDP treatment (–1·19, F = 6·87, P = 0·02) with no other changes in the subscales of mood evident(Reference Lee, Pase and Pipingas32). Following 10 d of MDP adherence, vigour rose by 18 % (3·67, F = 11·25, P = 0·003) in the MDP condition with no other dimensions of mood significantly affected(Reference McMillan, Owen and Kras30).
Using the Bond–Lader scale, alertness and contentment were improved by MDP in all three studies used this scale. The results were as follows: alertness (P = 0·003) and contentment (P = 0·001)(Reference De Vries, Van Schrojenstein Lantman and Hoebregts33); alertness (6·93, F = 14·11, P < 0·01) and contentment (5·35, F = 6·49, P < 0·02) scores(Reference Lee, Pase and Pipingas32); and alertness (16·43 (about 30 %), F = 22·23, P < 0·001) and contentment (12·89 (about 20 %), F = 16·634, P < 0·001)(Reference McMillan, Owen and Kras30). No significant change was reported for calmness.
Using the Multidimensional Mood State Questionnaire test, no main effect of meal type interventions was observed for mood(Reference Diekmann, Wagner and Huber31).
Secondary outcome measures
Two of the studies reported dietary adherence. In the Lee et al.’s study(Reference Lee, Pase and Pipingas32), all of the participants (n 24) an average MDP adherence of 94 % was evident which ranged from 80 % to 100 %. Similarly, in the McMillan et al.’s study(Reference McMillan, Owen and Kras30), a mean MDP adherence of 93 % for meals (range 80–100 %) and 95 % for snacks (85–100 %) was reported.
No significant impact of a MDP meal v. WD meal on plasma cortisol levels was evident(Reference Diekmann, Wagner and Huber31). Only Lee et al. assessed the impact of intervention on blood pressure, blood flow velocity and arterial stiffness(Reference Lee, Pase and Pipingas32). A significant decrease (–1·05, F = 6·15, P = 0·02) in augmentation pressure (mm Hg) was observed in the MDP condition relative to the control group.
Diekmann et al. assessed the desire to eat(Reference Diekmann, Wagner and Huber31). The overall hunger was not influenced by meal, while satiety was higher after MDP as compared with the WD (P < 0·001).
Body weight and BMI were tracked in two of the studies. Lee et al. (Reference Lee, Pase and Pipingas32) reported a significant weight loss in the MDP (–1·77 kg, F = 10,81, P < 0·01) group. McMillan et al. (Reference McMillan, Owen and Kras30) observed no significant main effect of diet on body weight, BMI or waist circumference between the two groups.
Discussion
This is the first systematic review to report the short-term effects of a MDP on cognition and overall mental well-being. The findings suggest that a MDP has the potential to affect cognition and mood in as little as 10 d. The findings have also identified important research gaps notably; there are few reported studies and of the studies available most were conducted in young people, aged 18–38 years(Reference McMillan, Owen and Kras30,Reference Lee, Pase and Pipingas32,Reference De Vries, Van Schrojenstein Lantman and Hoebregts33) and all conducted in individuals without cognitive or mental health complaints. In addition, there was a tendency to study females with only eighteen males in the 128 participants from the four studies. Therefore, the short-term effect of a MDP on mental health status in older adults, and in particular individuals who present with evidence of cognitive or mental health decline, is currently unknown.
Specific cognitive domains improved in all of the studies assessing the cognition, although the findings were not consistent(Reference McMillan, Owen and Kras30–Reference Lee, Pase and Pipingas32). Attention was significantly improved after the MDP in one study, with the authors speculating that this difference may be caused by the higher glucose content of the MDP (carbohydrate content of the meals: 133 g in MDP v. 93·7 g in WD) as the brain uses glucose as the primary source of energy(Reference Diekmann, Wagner and Huber31). Other studies reported improvements in immediate and delayed memory recall tasks, working memory and reaction times(Reference Lee, Pase and Pipingas32), and spatial working memory(Reference McMillan, Owen and Kras30). Consistent with these short-term effects, previous studies have reported longer-term (8 weeks) effects of a MDP enriched with dairy foods on processing speed in adults at above average CVD risk in the MedDairy study(Reference Wade, Davis and Dyer39).
Mood dimensions, namely, alertness and contentment, were significantly and consistently improved by MDP in the short-term in all four studies. Vigour(Reference McMillan, Owen and Kras30,Reference De Vries, Van Schrojenstein Lantman and Hoebregts33) and confusion(Reference Lee, Pase and Pipingas32,Reference De Vries, Van Schrojenstein Lantman and Hoebregts33) were also improved following the MDP. Adherence to a MDP has previously been shown to be associated with reduced risk of depression in elderly(Reference Masana, Haro and Mariolis40), and in the MedDairy study, a reduction in depression, tension, anger, confusion and total mood disturbance score was recorded following the 8-week dietary intervention period(Reference Wade, Davis and Dyer39). Furthermore, polyphenols intake, which are considered an important bioactive in the plant-based MDP, has shown to reduce depressive symptoms(Reference Bayes, Schloss and Sibbritt41).
Previous short-term studies using other dietary intervention or health endpoints provide insight into the possible mechanistic basis for the effect of a MDP on mental health. Myette-Côté et al. (Reference Myette-Côté, Durrer and Neudorf42) examined the effects of a low-fat, low glycaemic index diet, to a low carbohydrate diet or a low carbohydrate plus post-meal walking, in type 2 diabetes on glucose levels and inflammatory factors in a RCT comprising three 4-days interventions. While improved glycaemic control was evident in the low carbohydrate diet group, plasma monocyte-derived microparticles reduced significantly in the low-fat, low glycaemic index diet group which was similar to a MDP, suggesting that cerebral hypometabolism and inflammation which are features of cognitive disorders may be positively modulated by short-term dietary strategies. Attuquayefio et al. (Reference Attuquayefio, Stevenson and Oaten43) reported a decrease in hippocampal-dependent learning and memory following a breakfast high in saturated fat, cholesterol and added sugar and low in protein relative to an isoenergetic healthy breakfast for 4 consecutive days, findings which were subsequently confirmed over a 1-week intervention period(Reference Stevenson, Francis and Attuquayefio44). The hippocampus is a core brain area for cognitive functions such as learning and memory(Reference Driscoll, Hamilton and Petropoulos45). Besides, the hippocampus is involved in anxiety-related behaviours(Reference Bannerman, Rawlins and McHugh46) and major depression(Reference MacQueen, Campbell and McEwen47). This evidence suggests that the hippocampus function can be affected negatively by an unhealthy eating pattern in as short period as 4 d.
The hippocampus also produces high concentrations of brain-derived neurotrophic factor (BDNF) which is important in attention, cognition and total behaviour(Reference Yeom, Park and Choi48). Decreased levels of BDNF have been linked to cognitive and mood disorders, and it has been identified as a therapeutic target in neurodegenerative and psychiatric impairments(Reference Teixeira, Barbosa and Diniz49). In PREDIMED study, a MDP raised BDNF levels over 3 years, whilst a MDP supplemented with nuts was linked to significant improvement in serum BDNF levels in individuals with depression(Reference Sanchez-Villegas, Galbete and Martinez-Gonzalez50). However, the existing literature does not provide any insight into the short-term impacts of a MDP on BDNF levels.
Blood brain barrier is a dynamic selective interface between the brain and the bloodstream, in which dysregulations are associated with cognitive (including Alzheimer’s disease) and psychiatric disorders(Reference Kealy, Greene and Campbell51). Although selected dietary components have been shown to affect blood brain barrier function such as permeability in animal models(Reference Youdim, Shukitt-Hale and Joseph52) and the blood brain barrier is susceptible to be impairment by a WD(Reference Hsu and Kanoski53), the impact of a MDP in short- or long-term mental health is currently unknown but should be a focus of investigation. Additionally, a reduction in cerebral blood flow is associated with cognitive dysfunction(Reference Mattsson, Tosun and Insel54). Lamport et al. (Reference Lamport, Pal and Macready55) investigated the impacts of high flavanones on cognition and cerebral blood flow in young healthy participants in an acute RCT. A high flavanone citrus juice resulted in a 2-h increase in cerebral blood flow and better performance in one cognitive task (Digit Symbol Substitution) was observed in the experimental group. McManus et al. (Reference McManus, Tejera and Awwad56) examined the acute effects of EPA or DHA, found in oily fish, on arterial stiffness in men at high risk of CVD. Four hours following to the test meal, vascular function was significantly improved by the DHA-rich oil. Besides, a MDP is known to chronically affect systematic vascular function(Reference Shannon, Mendes and Köchl57).
The influences of the gut microbiota on cognition and overall mental well-being are well-recognised(Reference Foster and McVey Neufeld58,Reference Proctor, Thiennimitr and Chattipakorn59) . Therefore, nutritional strategies targeting the gut health may represent a meaningful strategy for delaying or even reversing neuropathology(Reference Bischoff60). David et al. (Reference David, Maurice and Carmody61) demonstrated that the gut microbiota can be changed through both animal-based and plant-based diets in 5 d. Moreover, in a 1-year longitudinal study, the gut microbiota responded to daily changes in diet(Reference David, Materna and Friedman62). Hence, accumulating evidence suggests that the gut–brain axis could mediate the even short-term effects of a MDP on cognition and mental well-being.
The current review highlighted that all of the participants in the MDP treatments from the two studies tracking dietary adherence(Reference McMillan, Owen and Kras30,Reference Lee, Pase and Pipingas32) reported high dietary adherence with no side effects. Besides, a MDP was linked to higher satiety in one study(Reference Diekmann, Wagner and Huber31) and significant weight loss despite no energetic restriction in the another study(Reference Lee, Pase and Pipingas32). Considering the fact that maintenance of healthy eating behaviours is not an easy task even in the short-term, this available evidence suggests that a MDP is an acceptable implementable approach even in non-Mediterranean countries.
The review has also highlighted a lack of consistency in how the MDP is applied. Despite the small number of included studies, none of them used the same dietary procedure, although the two Australian studies gave similar instructions to their participants(Reference McMillan, Owen and Kras30,Reference Lee, Pase and Pipingas32) . Abdelhamid et al. (Reference Abdelhamid, Jennings and Hayhoe63) have previously reported the high inconsistencies in food and nutrient intake through when adopting a MDP. Davis et al. (Reference Davis, Bryan and Hodgson64) also reported discrepancies in how the MDP was defined and the resulting nutrient intakes, with vegetable intakes, for example, ranged from 191 to 500 g/d in high MDP adherers. A greater standardisation in the definition of a MDP is needed in order to integrate data from difference sources and translate it in dietary recommendations focussed on improved short- and long-term health.
The main strength of the present paper is that it is the first systematic review to examine the short-term impact of a MDP on mood and cognition. Second, the database combination used ensured optimal coverage of the data(Reference Bramer, Rethlefsen and Kleijnen26,Reference Gusenbauer and Haddaway27) and has been shown by others to retrieve 95·9 % of available references(Reference Bramer, Rethlefsen and Kleijnen26). Third, the review covers all available literature up to December 2020. As for limitations, the number of studies found was small; therefore, the conclusions are preliminary rather than robust. However, this limitation provided an opportunity to identify research gaps. The second limitation is the high heterogeneity in the dietary and mental health status assessments used. This methodological variability restricted making comparisons between studies.
In conclusion, the possible short-term beneficial impacts of a MDP on cognitive and mental health have been reviewed systematically for the first time. The results provide some initial evidence that short-term dietary interventions can confer health benefits which directly and/or indirectly improve cognitive and mental health. However, future studies are required to elucidate which cognitive and other mental health domains could be beneficially affected and what are the underlying physiological mechanism mediating the effects. Short-term strategies to improve cognition, mood and anxiety are not only of interest to improve quality of life and capabilities in those with existing mental health deficit but also in healthy individuals. The definition of the MDP in future studies should be carefully considered, with attention given to its population adoption taking into account social, geographical and cultural mediators of eating behaviours.
Acknowledgements
We would like to thank to Lee Hooper, RD, PhD, an expert in systematic reviews, and Matthew Smith, the academic librarian of the Faculty of Medical and Health Sciences, University of East Anglia, for their contributions throughout the review.
L. E. is financially supported by the Ministry of National Education, The Republic of Turkey. Our ongoing (A. M. M. and A. J.) research programmes at UEA on the MDP and cognitive health are funded by Alzheimer’s Research UK (ARUK, PRRF2017-006), MRC (MR/T001852/1) and the ESRC (ES/S010408/1). K. J. M. and A. M. M. are chief investigators on a National Health and Medical Research Council funded research programme looking at the cognitive benefits of a MDP+walking in older Australian adults (NHMRC, APP1171300).
A. M. M. and K. J. M. formulated the research question. L. E. and E. S. C. conducted the systematic review of the literature. L. E. and A. J. conducted the risk of bias analysis. A. M. M., A. J. and L. E. interpreted the data. L. E. drafted the manuscript with all authors contributing to the manuscript ad approving the final version.
None to report.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114521002567





