Introduction
Breastfeeding is a public health priority that aims to reduce health inequalities; as women in lower socio-economic groups are less likely to breastfeed their babies. Breastfeeding saves lives and protects the health of mothers and babies both in the short and long term (Horta et al., Reference Horta, Bahl, Martines and Victora2007). More mothers are initiating breastfeeding, but continuation rates in the United Kingdom remain among the lowest worldwide with only 50% of mothers breastfeeding by six weeks (Bolling et al., Reference Bolling, Grant, Hamlyn and Thornton2007).
UK Government policy, underpinned by National Institute for Health and Clinical Excellence (NICE) guidance, promotes the adoption and implementation of the World Health Organization (WHO)/United Nations Children's Fund (UNICEF) Baby Friendly Initiative (BFI) as the best evidence-based vehicle to raise levels of breastfeeding prevalence (UNICEF, 2010; Dyson et al., Reference Dyson, Renfrew, McFaddon, McCormick, Herbert and Thomas2006; Department of Health, 2008; NICE, 2008). The BFI seven-point community programme provides a comprehensive framework for sustaining breastfeeding and a three-day breastfeeding management course for training midwives, health visitors, neonatal nurses and other health-care staff with primary responsibility for clinical breastfeeding support (UNICEF, 2008). The course provides thorough teaching in the process of lactation and related topics, including the importance of breastfeeding, how lactation works, positioning and attachment at the breast, hand expression, recognising and treating common breast conditions and more challenging situations. Participants are also given practical training in the skills needed to support successful breastfeeding and informed decision making, including three clinical practices (two are supervised) on observing a breastfeed, teaching positioning and attachment and hand expression.
In the United Kingdom, postnatal care for women is normally provided by midwives for the first 10–14 days and then transferred to the health visiting team, made up of both health visitors and nursery nurses. Health visitors are registered nurses or midwives with at least one year of further (post registration) training; nursery nurses have a basic childcare qualification and provide support to health visitors in the care for children up to the age of five years.
The effects of implementing the BFI programme on breastfeeding initiation rates are well documented from training acute sector staff (Bartington et al., Reference Bartington, Griffiths, Tate and Dezateuax2006), but no formal evaluation has taken place of the effects in a large UK community setting such as a Primary Care Trust (PCT). A randomised intervention study in Denmark showed that 52 health visitors who received training using a WHO breastfeeding counselling course increased their knowledge of breastfeeding practice and their self-efficacy in helping mothers to overcome common breastfeeding problems compared to controls in the comparison group (Kronborg et al., Reference Kronborg, Varth and Olsen2008).
As part of their plans towards meeting Government targets to increase breastfeeding rates at eight weeks, NHS Bristol (PCT) purchased the BFI breastfeeding management course for all their health visiting teams. NHS Bristol serves a population of around 400 000 people with 24 health visiting teams across the city. All health visiting team members took part in mandatory training in a series of BFI courses from April to December 2008, and all but two staff members attended the training. In addition to providing this training, breastfeeding awareness sessions were offered to general practitioners (GPs) and Children's Centre workers; 15 GP practices (25% of total in Bristol), support workers from 17 Children's Centres (70% of total) and 15 health links translators attended awareness raising sessions. Although the implementation of BFI standards was the main intervention in place in Bristol, pre-existing breastfeeding support included a small number of breastfeeding support groups, either facilitated by peer supporters or health professionals.
This study aimed to conduct a thorough evaluation of the health visitor team training to explore the outcomes of the training on routinely collected breastfeeding rates at eight weeks; on breastfeeding attitudes, knowledge and self-efficacy of staff; and on the perceptions of mothers.
Our previous research of the effects of breastfeeding management training on primary health-care staff has reported changes in knowledge about breastfeeding for all health professionals involved in a short training session and improvement in health visitor scores on the recognition of poor attachment at the breast (Ingram, Reference Ingram2006). Using tools based on behaviour change theory to explore staff confidence in helping mothers to breastfeed may help to explain how some interventions work and indicate changes in addition to expected improvements in attitudes and knowledge.
Methodology
Infant feeding rates
These are routinely collected by GPs for all infants at their eight-week check, recorded on the Avon Child Health Surveillance system, and data are extracted by the public health analysts at NHS Bristol. Exclusive breastfeeding has been defined by WHO as an infant receiving only breast milk without any additional food or drink (not even water). Any breastfeeding includes mothers who are exclusively breastfeeding and those who are mixed feeding with some bottles of formula milk in addition to breast milk. Breastfeeding rates have been collected for many years, and exclusive breastfeeding rates collected since 2006, and thus comparisons were possible for both any breastfeeding and exclusive breastfeeding rates. Rates were monitored from 2006 onwards, plotted graphically and compared using χ 2 tests and regression analysis to explore the odds ratios of a baby being breastfed in 2009 compared to 2006.
Knowledge and attitudes of health visitor team staff
1) All staff (n = 141) were invited to take part in the evaluation process comprising a three-stage questionnaire survey. Questionnaires were given immediately before and one month after training, and six months later. The validated Breastfeeding Questionnaire (Ingram, Reference Ingram2006) measured attitudes and knowledge about their current practices and a checklist assessed evidence-based management of breastfeeding problems. A self-efficacy tool assessed staff confidence in helping and supporting mothers to breastfeed.
The Breastfeeding Questionnaire, a validated tool used by Scott et al. (Reference Scott, McInnes, Tappin and Guthrie2003) and this shorter version used by Ingram (Reference Ingram2006), has 20 questions on attitudes to and knowledge of breastfeeding. The questions use Likert scale responses ranging from strongly agree (rated 5) to strongly disagree (rated 1). The breastfeeding attitude score is the sum of responses to 13 questions with a maximum score of 65; the knowledge score has seven questions with a maximum score of 35. The second part of the questionnaire has eight multiple-choice questions on breastfeeding management covering the treatment of mastitis, breast milk insufficiency, attachment at the breast, sore nipples and nipple thrush.
The Self-Efficacy tool has five questions with a response rate from 1 (not at all confident) to 10 (completely confident) giving a maximum of 50. The tool was based on Bandura's Social Learning Theory (Self-Efficacy theory), which indicates belief and confidence about one's perceived ability to plan and carry out specific tasks (Bandura, Reference Bandura1977). Behaviour-specific scales have been developed to identify those with high or low confidence. The topics covered in the self-efficacy tool were developed, piloted and agreed in discussions with health visitor colleagues and included statements about teaching correct positioning and attachment, supporting breastfeeding women, identifying and solving breastfeeding problems and supporting exclusive breastfeeding up to six months. These topics were covered in the BFI training and in routine assessments of staff practical skills, which were part of the BFI process.
Background information collected (relevant to breastfeeding) included whether staff had any children, how many were breastfed and whether breastfeeding had been a positive or negative experience for them.
The first questionnaire was given to each course member during the pre-course lunch time and completed forms collected by the researchers before the first training session started. Staff were also invited to be interviewed by a researcher at a later date with a reply slip enclosed with the questionnaire. The second and third questionnaires were posted and telephone call reminders made two weeks later to ensure a high return rate.
Descriptive statistics (means, frequencies) were produced and plotted graphically from the staff questionnaires. Comparisons between staff knowledge, attitudes, self-efficacy scores and the correct treatment of breastfeeding problems for health visitors and nursery nurses were made using paired t-tests. Comparisons over the three time points were made using repeated measures ANOVA for staff who had returned all three questionnaires.
2) Further process evaluation of the BFI training was carried out through short semi-structured interviews of health visitors, nursery nurses and managers using a topic guide to explore their attitudes to and views of the success of the training, changes in practice and management of breastfeeding. Staff were purposively sampled from the 50 who had agreed to be interviewed, to include a range of bases, staff type and course attended, and they were interviewed by telephone two to three months after the courses. These interviews took place during the working day at a time convenient to the staff. The managers were also interviewed three months after the end of the training period in face-to-face semi-structured interviews using a topic guide. Semi-structured interviews were used to ensure that similar topics were covered with all staff in the limited time available during the working day. All interviews were digitally recorded, transcribed and analysed with NVIVO8 using thematic methods of generating codes, themes and sub-themes from the data (Silverman, Reference Silverman2000). Two researchers coded the transcripts and developed themes in an iterative process by discussion and agreement. One researcher used NVIVO8 to facilitate the process and the other coded by hand. The interviews focussed mainly on the processes involved in the training and its effects on practice.
Perceptions of mothers
Mothers (n = 101) were invited to take part in a short structured questionnaire-based interview to explore their experiences of breastfeeding and any problems they had encountered.
For two months before staff BFI training (May and June 2008) and a three-month period six months after the courses had finished (April to June 2009), mothers at nine health centres (covering 13 postcode areas across the city) were purposively sampled at clinics and postnatal groups to include a range of mothers with babies over six weeks who had started to breastfeed. All those who were approached by the researchers agreed to take part. They completed two short questionnaires with one of the researchers: the Breastfeeding Self-Efficacy Scale-Short form (Dennis, Reference Dennis2003) to assess confidence about breastfeeding; and a record of their breastfeeding experiences to assess advice and support about any problems they had encountered. The mothers’ self-efficacy score was derived from 14 questions with a score of 1 (very little confidence) to 5 (very confident), giving a maximum total of 70. The questionnaires took about 10 min to complete; most sections were self-completed with some discussion about the problems with the researcher completed as free text. Comparisons were made between mothers interviewed before and after staff training using unpaired t-tests.
Local Research Ethics and Research Governance permissions for the study were obtained. Permissions were also given by those hosting groups or running clinics to approach women attending.
Results
Breastfeeding rates
Table 1 and Figure 1 show that the increases in any breastfeeding and exclusive breastfeeding rates at eight weeks were statistically significant (P < 0.001, χ 2 tests) when comparing the rates over four years from 2006 to 2009, and comparing the rates before BFI training with those after training. Regression analysis showed that compared to 2006, a baby born in 2009 was 1.57 times more likely to be breastfed and 1.46 times more likely to be exclusively breastfed at eight weeks old. These increases are encouraging as eight-week breastfeeding rates have been static at just under 50% in Bristol for many years.
Table 1 Breastfeeding rates from 2006 to 2009 in BristolFootnote a
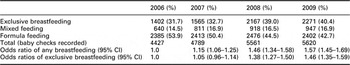
a Data from NHS Bristol public health analysts.
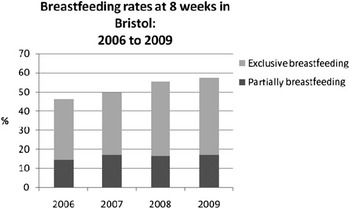
Figure 1 Breastfeeding continuation rates at eight weeks for babies born in Bristol from 2006 to 2009 (Data from NHS Bristol public health analysts).
Staff
Questionnaire survey
A total of 141 staff attended training, 137 of whom completed the baseline questionnaire (Q1) before the training session (97% of those trained) comprising 100 health visitors, 34 nursery nurses and three maternity support workers. A total of 121 staff completed questionnaire 2 (Q2), the post-training questionnaire (88.3% of 137 Q1) and 98 returned questionnaire 3 (Q3), the six-month questionnaire (71.5% of Q1; see Table 2). Thirty-nine per cent of staff needed a reminder for Q2, and 42% for Q3. The lower number of staff returning the third questionnaire was mainly due to staff leaving, being on maternity leave or off sick rather than refusal to complete the questionnaire.
Table 2 Staff background information from questionnaire returns
The mean values and standard deviations of scores for staff attitudes, knowledge and confidence about breastfeeding for health visitors and nursery nurses are shown in Table 3. There were significant increases in staff attitudes to, knowledge of and self-efficacy with supporting breastfeeding (P < 0.001) from baseline to after training, and these improvements were maintained six months later.
Table 3 Staff attitudes, knowledge and self-efficacy about breastfeeding collected at three time points, before and after BFI training and six months later (mean values and SD)
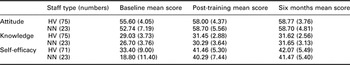
BFI = Baby Friendly Initiative; HV = health visitors; NN = nursery nurse.
Data are shown for staff who returned questionnaires at all three time points (n = 98).
Table 4 and Figure 2 show the differences in scores for health visitors and nursery nurses from before training to six months later. There were significant differences in the attitudes (P = 0.017), knowledge (P = 0.010) and self-efficacy (P < 0.001) between health visitors and nursery nurses before the courses, and no significant differences after training or six months later, showing that the training successfully reduced the differences between the groups and significantly improved the scores for nursery nurses. Repeated measures ANOVA tests confirmed that there were no significant differences after training over time or between staff groups (attitudes P = 0.752; knowledge P = 0.423; self-efficacy P = 0.678).
Table 4 Differences between HV and NNs’ attitudes, knowledge and self-efficacy scores at the three time points (t-tests; n = 98)
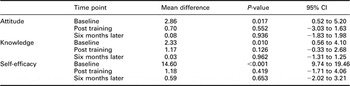
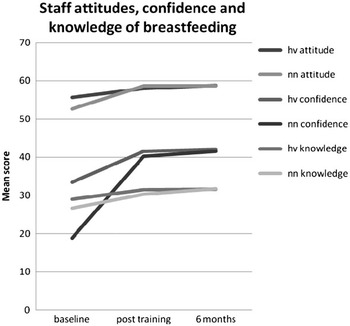
Figure 2 Health visitor (HV) and nursery nurse (NN) attitudes and knowledge of breastfeeding, and their confidence in helping breastfeeding mothers before and after BFI training (n = 98 with data at all time points).
Three quarters of the staff had children, and 95% of these had breastfed at least one child as shown in Table 2. There was a significant correlation between how much they had enjoyed breastfeeding and their self-efficacy with breastfeeding (P < 0.001, Pearson correlation = 0.4). However, there were no significant differences in attitudes, knowledge or self-efficacy between those with and without children, or between those who had breastfed or not.
Part of the Breastfeeding Questionnaire was a checklist about the management of several breastfeeding conditions, including breast milk insufficiency, poor attachment, sore nipples, mastitis and nipple thrush. All staff showed significant increases in the appropriate advice for breast milk insufficiency (P < 0.001) and mastitis (P = 0.004) after training. In addition, significant increases in recognising the symptoms of poor attachment (P < 0.001) were seen. There was some improvement in recognising the symptoms of sore nipples and nipple thrush but these were not statistically significant.
Interviews with health visitor team members
Thirty-five telephone interviews were conducted with 28 health visitors and seven nursery nurses, which each took between 10 and 20 min to complete. There was overwhelming support for the course, with many reporting that it was one of the best courses they had ever attended.
It was a vital update really; I was really pleased I went. I really enjoyed it. I did come away thinking – Oh my goodness, I have been giving duff advice on several occasions. (HV)
When asked about their previous breastfeeding training, health visitors reported receiving very little during professional qualification and had only increased their knowledge if self-motivated to do so. Prior to the BFI course, they felt under-prepared to give mothers breastfeeding support and advice. Nursery nurses had mostly had no prior breastfeeding management training.
The ease of attending the course, which ran over three days, was discussed and some felt that the course could perhaps be reduced to two full days. However, colleagues were mutually supportive in enabling each other to attend by organising cover.
Cover's always a problem, we just muddle through when someone's on training … it's something you've got to get through. (HV)
Themes developed during the analysis were:
• confidence in advising women
• changing practice
• consistent advice.
Confidence in advising women
Interviewees felt more confident and better equipped to support breastfeeding women after attending the course. It was often an assumption that health visitors should know about breastfeeding and how to advise women, but few felt really confident before the training.
It was a revelation. I've spent my whole career feeling inadequate and now I feel much better about it. (HV)
It's given me more knowledge, more skills and I feel more confident now talking to Mums. (NN)
Changing practice
Many health visitors talked about how their practice had changed, particularly in the way they explained things to mothers and the language they used. They highlighted being able to identify poor attachment, use skin-to-skin for solving problems, explain how to hand express breast milk, use educational aids to describe positioning and attachment and understand the physiology of breastfeeding better.
I think that some of the language that has been used is very useful to explain to the people you're visiting. (HV)
I think I'm a lot better at spotting poor positioning, and I'm able to be clearer about how to change it specifically. (HV)
The hormonal stuff, the idea of switching the breasts on to produce prolactin. When you're talking to mums you encourage them to let the baby touch their breasts…… babies need to have the room to do that, so that anybody clutching onto the back of the head is counter-productive- so that's caused a change in my practice. (HV)
Some things have changed slightly, like how to hand express, it's much easier…the physical way of doing it. I quite often discuss it now. (HV)
Consistent advice
Staff felt confident that, for the first time, they were all able to give consistent, up-to-date, evidence-based advice, and were singing from the same hymn sheet. This was mentioned by many who felt that previously they all had different approaches and information, which might be confusing for mothers. Training the whole team had enabled nursery nurses to become more knowledgeable and better equipped to support breastfeeding mothers, and thus health visitors now felt confident to delegate time-consuming breastfeeding input and the running of breastfeeding support groups to them. This had not been possible before as the nursery nurses had little previous experience of breastfeeding.
I think it's probably made us more consistent, so that people are getting the same information from all members of staff, which wasn't necessarily happening before. (HV)
I feel totally confident to pass mothers on to the nursery nurses now who have really benefited from training. They come back and discuss with the rest of us any difficulties they've experienced and their knowledge is fantastic now. (HV)
Managers’ interviews
Three managers were interviewed about the process of facilitating BFI training across the whole PCT. These interviews explored their views and impressions of the initial stages of the process, how they had enabled it to take place and whether it had been worthwhile.
Initially, there seemed to be some resistance towards the initiative, but this was explained by their concerns about the ramifications of training all the staff with the current low-staffing levels. A budget was provided by the PCT breastfeeding strategy managers to assist with paying for bank staff, but often there were not enough staff to provide the cover. Free childcare, in the form of a crèche at the venues, was also made available to enable part-time staff to attend courses on days when they did not have childcare provision, but not many staff used it. However, both incentives were felt to be important to enable this type of initiative to be rolled out successfully.
I think the difficulty that we had as managers was that we knew how dire our staffing levels were and wondered how on earth we were going to keep the service going with everyone needing to be trained.
The very positive feedback made by staff to their managers helped motivate managers to encourage and support more staff to attend.
I don't think I have heard a single criticism of the training, which is quite unusual for health visitors…. The reports across the board were that it was really high quality, well worth going on,… so from that point of view it was brilliant. It is very close to their clinical practice, it's stuff that they do every day, it's not like going on training that hasn't got much to do with them.
I would say that everybody, even the most cynical of them, was positive about it. I've had the most positive feedback of any training we've run, they really enjoyed it. It enthused a lot of health visitors that were maybe feeling a bit jaded, .it's what they went into health visiting to do.
When asked for any examples of changes in practice that they had noticed, they felt that these had mainly been to enable the ‘skill mix’ staff (nursery nurses, registered nurses) to take more responsibility for supporting breastfeeding women.
It has engaged not only the health visitors, but also their skill mix staff…… At the moment quite a lot of the clinical work is delegated within the team according to people's competencies, so very often the people at the coal face talking to the Mums are the skill mix staff, so that's been incredibly positive.
Mothers’ survey
The mothers’ survey was too small to show any statistically significant changes after the staff had been trained. A total of 101 mothers were involved (42 before and 59 after training); 76% first-time mothers; 85% were breastfeeding at eight weeks and 66% were exclusively breastfeeding. Many mothers (before and after staff training) had not received advice from a health visitor about breastfeeding, but had seen nursery nurses at breastfeeding groups, and they were generally satisfied with the support received.
There were some interesting observations from this survey including an increase in those who were breastfeeding exclusively from 57% in phase 1 (before staff training) to 73% in phase 2 (after staff training). There was also an increase in mothers’ self-efficacy scores from 54.1 in phase 1 to 57.8 in phase 2 (P = 0.1), but due to the small sample size the increase was not statistically significant. A power calculation showed that we would have needed to have seen three times as many women (154 in each group) as we sampled to detect this difference at the 0.05 level. However, there was not sufficient time after receiving ethical permission and before staff training started to increase the numbers of women in this part of the evaluation.
There were indications, from mothers who had experiences with previous babies, that changes had been noticed with comments such as ‘(they were) more knowledgeable about breastfeeding this time’.
There were slightly more women reporting breastfeeding problems in phase 2, but most felt that the advice had been good and their problems were resolved. The problem giving most cause for concern was nipple thrush, which was poorly recognised and treated by staff and more likely to be unresolved for mothers. This confirms the finding from the staff survey that recognition and treatment of nipple thrush is more uncertain for some staff.
Discussion
This study has shown that implementing the BFI across NHS Bristol has facilitated a significant increase in breastfeeding continuation rates since the start of training in 2008. The evaluation of the BFI training for all the health visitor teams across the PCT has highlighted increases in positive staff attitudes towards breastfeeding and improved knowledge of breastfeeding. The training also renewed enthusiasm for breastfeeding, improved the consistency of advice and raised self-efficacy levels of all staff who help mothers with breastfeeding. Managers’ concerns about training all the staff in a relatively short span of time were eased by the provision of funding for bank staff and good consultation before the process started. Recent achievement of Baby Friendly status in the PCT (March 2010), since this evaluation, has now made Bristol the first ‘Baby Friendly’ city in the United Kingdom with both maternity units and the PCT holding BFI awards, and this study is the first to evaluate the effects of training on a whole PCT.
Limitations to the study include the fact that it was only conducted in one city, and thus there are no experiences from different areas. As this was mainly a detailed process evaluation, there was no opportunity to randomise participants to receive training or not and measure the outcomes. In addition, the small size of the survey of mothers’ experiences, which was not large enough to show statistical changes in behaviour, limited the findings, but there was an increase in exclusive breastfeeding reported and signs of increased self-efficacy for breastfeeding mothers. The survey would need to have been much larger to show significant changes in outcomes for mothers, and this should be an important aim for any future studies.
Kronborg et al. (Reference Kronborg, Varth and Olsen2008) randomised health visitors to receive training in a three-day breastfeeding course and showed that this training combined with specific targeted postnatal visits to mothers increased health visitors’ breastfeeding knowledge scores and self-efficacy in breastfeeding guidance compared to controls. Mothers in the intervention group also reported more breastfeeding support from the staff. Ingram (Reference Ingram2006) showed similar increases in breastfeeding knowledge for health visitors after an interactive training session combined with a CD breastfeeding learning package.
Using a breastfeeding self-efficacy framework in this study has shown that there were large increases in health professionals’ self-efficacy after training, particularly for nursery nurses who had previously not received any training in breastfeeding but were often involved in discussions with breastfeeding mothers at support groups. This finding was supported by the interviews reporting individual feelings on how training had changed practice. Differences in mothers’ self-efficacy were also seen. It has been suggested that the mothers’ self-efficacy assessment tool used in our study could also be used to individualise care for women, as well as evaluate health-care interventions (Dennis, Reference Dennis1999). Other studies have suggested that the psychosocial aspects of breastfeeding support explored in self-efficacy theory should be taken into account by health professionals and incorporated into BFI training (Entwistle et al., Reference Entwistle, Kendall and Mead2010). Exploring the theories of behaviour change in a breastfeeding context for those supporting women and breastfeeding women themselves may help to explain how and why some interventions work or not. McMillan et al. (Reference McMillan, Conner, Green, Woolridge, Dyson and Renfrew2009) used the theory of planned behaviour to examine factors influencing breastfeeding intentions and behaviour, and suggested that it too could be a useful framework for testing the effectiveness of breastfeeding interventions.
Health visitor professional training currently may not equip them to support breastfeeding women. Wallace and Kosmala-Anderson (Reference Wallace and Kosmala-Anderson2007) surveyed the training needs of health-care practitioners in breastfeeding support skills, and concluded that practice-based training with access to evidence-based policies was required. BFI offer an assessment and accreditation programme for universities. However, to date, this is only available for midwifery courses but will soon be available for health visiting courses (www.babyfriendly.org.uk; Duffy, Reference Duffy2008). Training establishments should be encouraged to make all their courses BFI accredited so that midwives, health visitors and nursery nurses have a recognised breastfeeding qualification from when they start work, rather than having to train community staff after they are in post.
Conclusions and implications for policy, practice and research
Making the BFI training mandatory across the whole PCT has improved the confidence of all health-care staff who help mothers with breastfeeding, and these improvements have been translated into increased breastfeeding continuation rates at eight weeks.
Health visitors identified that their previous breastfeeding training was minimal, and as they are the main health professionals supporting and advising breastfeeding women after the early days, this caused a surprising lack of confidence. The BFI training not only increased their confidence, but dramatically improved the confidence of the support workers. Training the whole health visitor team enabled health visitors to delegate breastfeeding advice and the running of breastfeeding support groups to nursery nurse team members with confidence, while maintaining overall supervision. Providing this high-quality training for support workers is important to enable them to be involved in supporting breastfeeding in this way. The challenge for Primary Care and Acute Trusts is continuing the on-going breastfeeding training to maintain breastfeeding expertise among the team and new staff as they come into post.
Future research could explore the use of a breastfeeding self-efficacy tool for routine clinical assessment and wider breastfeeding research evaluations with both health professionals and mothers.
Acknowledgements
The project was funded by the Public Health Directorate of NHS Bristol. We would like to thank all the staff and mothers who took part, Nicki Symes and Sally Tedstone for facilitating the evaluation and our presence at the training sessions, and Rosemary Greenwood for advice on the statistical analysis.








