In-patient resources in psychiatry are increasingly limited, with only the most seriously ill or at risk patients being admitted in many regions throughout the country. Evidence is emerging for increased admission rates for young men with major mental illnesses in Scotland (Reference Cavanagh and ShajahanCavanagh & Shajahan, 1999). There may be many potential reasons for this, including increased morbidity in men, changing diagnostic patterns or even preferential admission of men. We hypothesised that the increased admission rate for men may be the result of men being preferentially admitted by psychiatrists, even though their ‘severity’ of illness may be the same as that of women.
The study
A questionnaire survey was devised and sent to all junior and higher psychiatric trainees (senior house officers (SHOs) and specialist registrars (SpRs) in the Lothian Region/South-East Scotland rotation. The questionnaire contained four psychiatric scenarios or case vignettes (see Appendix). These vignettes represented a range of severity of risk in terms of self-harm. At one end of the range (Scenario 1) the risk of self-harm could be perceived as relatively low. At the other end (Scenario 4) the risk could be considered substantial. The psychiatrists were asked to rate along a five-point scale (definitely to definitely not) how likely they were to admit the person that the scenario related to. Half the psychiatrists received a questionnaire where Scenarios 1 and 3 related to female patients and Scenarios 2 and 4 related to male patients. The other half received a questionnaire where Scenarios 1 and 3 related to male patients and Scenarios 2 and 4 related to female patients.
Findings
One hundred and fourteen questionnaires were sent out randomly to 79 SHOs and 35 Registrars. Eighty-nine were returned representing a response rate of 78%. Figures 1a to d show the response patterns for the various case scenarios. The distributions did not follow a normal distribution and non-parametric statistics (Kruskal-Wallis) were used to analyse the data. The Kruskal-Wallis test showed a significant effect of admission by scenario (χ2=244, P<0.0001), but no overall effect on admission due to the gender of the patient (χ2=0.86, P=0.35). Figure 1a, Scenario 1, shows that the majority of psychiatric trainees were unlikely to admit the patient concerned irrespective of whether they were male or female. At the other extreme (Fig. 1d, Scenario 4) all trainees were either ‘definite’ or ‘very likely’ to admit, irrespective of whether male or a female. Scenarios 2 and 3 represented a more ‘grey’ area where there was a greater difference of opinion as to whether admission was appropriate or not. If anything, a trend was seen in a more likely admission for a woman than a man for Scenario 3.
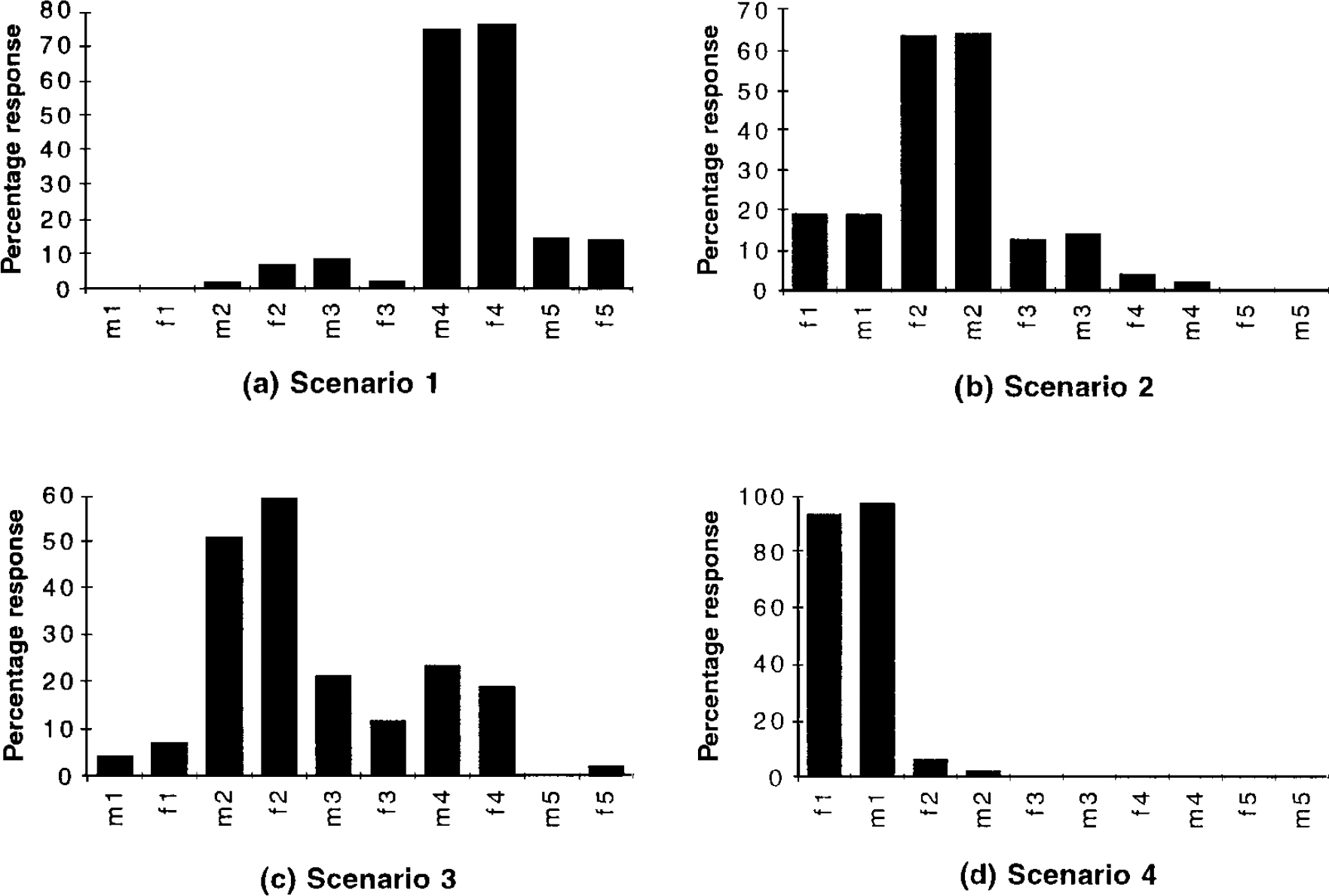
Fig. 1. 1, definite; 2, likely; 3, unsure; 4, unlikely; 5, definitely not; m, male; f, female.
Comment
Our hypothesis was not supported. Admission patterns for men and women are approximately the same. We managed a satisfactory response rate in terms of questionnaire surveys which represents the views of the majority of psychiatric trainees in this region. It is not surprising, and indeed reassuring, that psychiatric trainees are more likely to admit those patients with serious illness and who are obviously at risk of self-harm, and that there is no bias when it comes to assessing a man or a woman. It is of interest that there is less consensus when the case (Scenario 3) is less clear cut in terms of clinical risk of self-harm.
The increased first admission rate for men with major mental illness is unlikely to be due to preferential admission by psychiatrists and is more likely due to other reasons such as increased morbidity of major mental illness in men.
Appendix
Scenario 1
A 22-year-old male is referred with an eight-month history of low mood and feeling that life is not worth living. He has disturbance of sleep and appetite. On questioning he is not psychotic and does not have immediate suicidal plans. He has not responded to firstline antidepressants.
How likely are you to admit this patient?
-
□ Definitely
-
□ Likely
-
□ Unsure
-
□ Unlikely
-
□ Definitely not
Scenario 2
A 20-year-old female is referred with a two-month history of low mood and feeling that life is not worth living. She has disturbance of sleep and concentration. On questioning she feels people are talking about her and she is contemplating suicide. She has been on fluoxetine 40 mg/day for the last four weeks.
How likely are you to admit this patient?
-
□ Definitely
-
□ Likely
-
□ Unsure
-
□ Unlikely
-
□ Definitely not
Scenario 3
A 21-year-old male is referred with a four-week history of worsening auditory hallucinations and anxiety. He states that his mood is low. On questioning he feels neighbours are discussing him. He does not have any suicidal ideas. He was started on chlorpromazine 100 mg/day by his GP two weeks ago.
How likely are you to admit this patient?
-
□ Definitely
-
□ Likely
-
□ Unsure
-
□ Unlikely
-
□ Definitely not
Scenario 4
A 20-year-old female is referred with a six-month history of bizarre behaviour and social withdrawal. She has boarded up the windows in her flat saying that people are spying on her. She has impaired sleep and appetite. On further questioning she has paranoid delusions and third person auditory hallucinations. She states that she is seriously contemplating suicide.
How likely are you to admit this patient?
-
□ Definitely
-
□ Likely
-
□ Unsure
-
□ Unlikely
-
□ Definitely not



eLetters
No eLetters have been published for this article.