Truncus arteriosus is a congenital cardiac defect in which the arterial trunk and semilunar valves fail to separate during embryogenesis, resulting in a single artery that supplies the systemic, pulmonary, and coronary circulations. Reference Collett and Edwards1–Reference Russell, Jacobs and Anderson3 Repairing truncus arteriosus typically involves separating the pulmonary arteries from the aorta, reconstructing a right ventricular outflow tract using a valved conduit or homograft for the neo-pulmonary valve, closing the ventricular septal defect, and repurposing the truncal valve as the neo-aortic valve. Concomitant anomalies may require additional intervention at the time of initial repair. Clinically significant truncal valve insufficiency is one such anomaly. Truncal valves with moderate or greater insufficiency require intervention during initial repair because these patients can otherwise progress to profoundly decompensated heart failure secondary to neo-aortic valve insufficiency. Reference Naimo and Konstantinov4 Prior studies have reported between 12 and 28% of primary truncus arteriosus repairs requiring concomitant truncal valve intervention. Reference Bakar, Costello and Sassalos5–Reference Kaza, Burch, Pinto, Minich, Tani and Hawkins8
Truncal valve intervention can be divided into two broad categories: repair and replacement. Truncal valve repair is generally preferable to replacement because repaired valves grow with the patient. Despite this, patients undergoing truncal valve repair still require high rates of reintervention compared with patients not requiring truncal valve intervention. Reference Bakar, Costello and Sassalos5,Reference Naimo, Fricke and d'Udekem6,Reference Kaza, Burch, Pinto, Minich, Tani and Hawkins8 Repair can be achieved using a variety of surgical techniques and is generally attempted in cases of moderate insufficiency with a truncal valve that is structurally amenable to repair. Reference Patrick, Mainwaring and Carrillo9 In cases of severe truncal valve insufficiency, truncal valve replacement may be required during the primary repair of truncus arteriosus. Reference Bove, Lupinetti and Pridjian10–Reference Ebert, Turley, Stanger, Hoffman, Heymann and Rudolph12 In studies reporting patients undergoing truncal valve replacement at the time of initial truncus arteriosus repair, outcomes have been mixed and patient numbers in individual studies are too few for robust statistical analysis.
While many studies have sought to evaluate the impact of truncal valve intervention on patient outcomes, Reference Bakar, Costello and Sassalos5,Reference Naimo, Fricke and d'Udekem6,Reference Russell, Pasquali and Jacobs13 there is a paucity of literature analysing outcomes for the subset of these patients requiring truncal valve replacement during the primary repair of truncus arteriosus. Therefore, to better characterise the outcomes of these patients, we performed a meta-analysis of published outcomes.
Materials and methods
Study strategy
This systematic review and meta-analysis follow the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines. Reference Moher, Liberati, Tetzlaff and Altman14 PubMed, Scopus, and CINAHL Complete were searched from inception until 2021 for studies evaluating outcomes after truncus arteriosus repair with concomitant truncal valve replacement. The queries for each database are described in detail in the Supplemental Materials. The search was conducted on 17 December, 2022. Search results were filtered by title using the key words as a reference, then potentially eligible articles were accessed and filtered according to predefined inclusion and exclusion criteria. The references of each included article were also screened to identify additional relevant studies.
Inclusion and exclusion criteria
The main criterion for inclusion was: all studies reporting outcomes of truncal valve replacement in infants and neonates during the primary repair of truncus arteriosus, defined as less than 12 months of age. This particular age range was chosen because truncus arteriosus is repaired early in current practice. Reference Bove, Lupinetti and Pridjian10,Reference Ebert, Turley, Stanger, Hoffman, Heymann and Rudolph12 Criteria for exclusion were: articles with non-infant study populations, articles that did not report separate outcomes for those undergoing truncal valve replacement, and articles where no truncal valve replacement occurred during the primary operation. Moreover, if there were multiple studies from the same centre, only the most recent or most complete study was included to avoid duplication of cases.
Outcome measures
The primary outcome was early mortality, defined as death within the first 30 days after the index operation. Secondary outcomes were late mortality occurrence rates (%/year, defined as death occurring >30 days after the index operation per patient-year) and reintervention occurrence rates (%/year, defined as total number of reported reinterventions per patient-year). Follow-up in patient-years was determined by multiplying the reported mean or median follow-up time by the total number of patients. If studies did not report separate follow-up times for patients undergoing truncal valve replacement, the median reported follow-up time was assumed to be the same as the follow-up time for the entire study population. Two authors verified and extracted the data from the included articles to populate a predefined database with all relevant variables for this meta-analysis.
Statistical analysis
Data analysis was conducted using R version 4.0.5 (The R Foundation), and the meta (version 6.0) R package was used to perform a meta-analysis of proportions and relative risks to evaluate early mortality and a meta-analysis of rates to evaluate late mortality and reintervention rates. Reference Balduzzi, Rücker and Schwarzer15 Individual proportions of the included studies were transformed using the Freeman–Tukey double arcsine transformation Reference Freeman and Tukey16 and aggregated using the DerSimonian–Laird random effects method. Reference DerSimonian and Laird17 This result was then converted into a pooled proportion using the inverse Freeman–Tukey double arcsine transformation. Reference Miller18 The Clopper–Pearson method was used to generate 95% confidence intervals. Relative risks were pooled using inverse variance weighting and the DerSimonian–Laird random effects method. For all corresponding 2 × 2 tables with zero cell counts, 0.5 was added only to the number of events for continuity correction. The Freeman–Tukey double arcsine transformation was unable to be used for rate calculations because the reported rates returned too small of a transformed proportion to invert. Reference Schwarzer, Chemaitelly, Abu-Raddad and Rücker19 Therefore, the log transformation was used in the calculation of rates. For studies reporting no events, 0.5 events were assumed for the sake of continuity correction. For rate calculations, a normal approximation was used to calculate 95% CI. Estimations and overall effect sizes were illustrated using forest plots. The heterogeneity of each meta-analyzed value was determined using the Cochran’s Q test and the I2 index. Reference Cochran20,Reference Higgins and Thompson21 Visual inspection of funnel plots and the Egger test were used to test for publication bias. Reference Egger, Smith, Schneider and Minder22 Additionally, survival and freedom from reintervention were examined using interval censored Kaplan–Meier analysis through the survival (version 3.4-0) R package. Reference Therneau23
Results
Literature search
Three hundred and thirty records were identified from the initial literature search, and 153 records were duplicates (Fig 1). Screening revealed that 132 studies were relevant to the analysis. Of these studies, 18 were excluded because they had a non-infant study population, 82 were excluded because truncal valve replacement was not performed during the primary repair, 12 were excluded because they did not report separate outcomes for truncal valve replacement, and 7 were excluded because there were later or more complete studies from the same centre. Three additional studies were identified form references, yielding a total of 16 studies for inclusion in the meta-analysis. Reference Naimo, Fricke and d'Udekem6,Reference McElhinney, Reddy, Rajasinghe, Mora, Silverman and Hanley7,Reference Bove, Lupinetti and Pridjian10,Reference Elkins, Steinberg, Razook, Ward, Overholt and Thompson24–Reference Seese, Turbendian, Castrillon and Morell36 These studies comprised a total of 41 infants undergoing truncal valve replacement at the time of primary repair for truncus arteriosus. Of these, 15 were single-center studies and 1 was a multi-institutional database study.
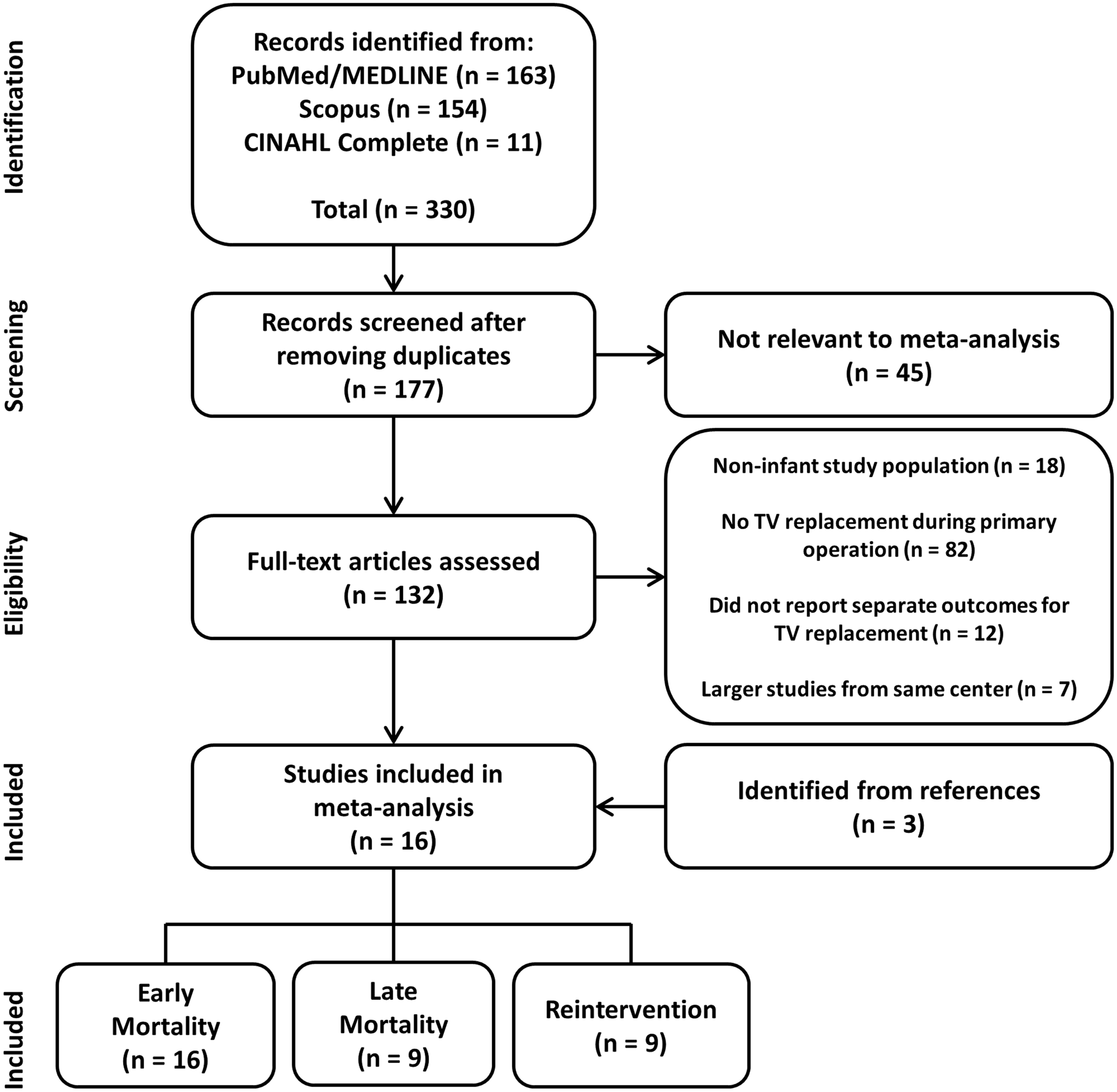
Figure 1. Preferred reporting items for systematic review and meta-analyses flow diagram depicting the study selection process.
Study characteristics
A total of 16 studies were included in the meta-analysis of early mortality, summarised in Table 1. These studies comprised a total of 908 patients undergoing repair of truncus arteriosus, with 41 undergoing concomitant truncal valve replacement. Each of the included studies reported ≤8 truncal valve replacements in infants. Eight studies originated in the United States, two from the United Kingdom, one from Japan, one from France, one from Belgium, one from Canada, one from Australia, and one from the Congenital Heart Surgeons Society database. Twelve of the 16 studies specified the type of valve replacement used, comprising 32 patients. Mechanical valves were used in 9 patients, homograft replacements were used in 22, and a bioprosthetic valve was used in 1.
Table 1. Characteristics of studies included in the analysis.

Abbreviations: No., number; TA, truncus arteriosus; TV, truncal valve; H, homograft; M, mechanical valve; B, bioprosthetic valve; CHSS, Congenital Heart Surgeons Society database. Follow-up is specific to patients undergoing TV replacement unless otherwise noted.
“-“ = not reported. “*” = median. “†” = not separately reported, assumed to be same as overall study population. “§” = not separately reported, assumed to be the same as population undergoing concomitant TV interventions.
Patient characteristics
The pooled pre-operative patient characteristics are summarised in Table 2. The majority of patients in this study were neonates, and most had severe truncal valve insufficiency. Most studies did not report truncal valve stenosis. The majority of patients were not reported to have other associated cardiac diagnoses. The most commonly reported associated cardiac diagnosis was interrupted aortic arch in four patients, followed by anomalous coronary anatomy in two patients.
Table 2. Summary of pre-operative characteristics of patients in the included studies.

Abbreviations: No., number; TV, truncal valve; IAA, interrupted aortic arch; HCM, hypertrophic cardiomyopathy.
Primary outcome
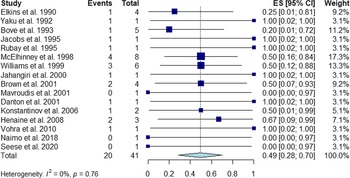
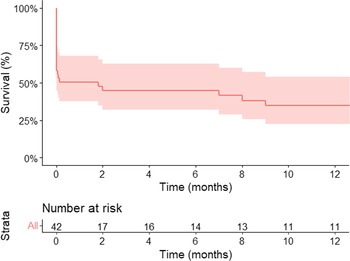
All 16 studies were available to evaluate early mortality after truncal valve replacement at initial truncal arteriosus repair, comprising a total of 41 patients. Meta-analysis revealed a pooled early mortality rate of 49.4% (95% CI: 28.4–70.5) (Fig 2, Table 3). Additionally, Kaplan–Meier analysis indicated a 1-month mortality of 49.4% (95% CI: 32.0–62.4) (Fig 3). Among individual studies, early mortality ranged from 0 to 100%, and there was no significant heterogeneity between the included studies (I2 = 0%; Cochran’s Q test p = 0.76). The funnel plot (Supplemental, Figure S3) and Egger test (p = 0.20) did not indicate publication bias.

Figure 2. Forest plot of early mortality following truncal valve replacement (CI, confidence interval; ES, effect size).

Figure 3. Kaplan–Meier analysis of survival following truncal valve replacement. The shaded area represents the 95% confidence interval.
Table 3. Results of meta-analyzed outcomes for patients undergoing TA repair with concomitant truncal valve replacement.

Data for proportions are formatted as percentage (95% CI). Data for rates are formatted as percentage per year (95% CI). “-“ indicates that variable was not reported in study. In rate calculations, studies with no reported events were assumed to have an occurrence of 0.5 events for continuity correction.
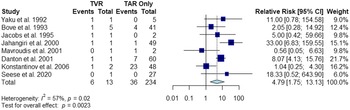
Of these 16 studies, 8 were included for the evaluation of relative risk of early mortality in infants undergoing truncal valve replacement and truncus arteriosus repair compared to those only undergoing truncus arteriosus repair without truncal valve replacement. Two studies were excluded because they lacked a truncus arteriosus repair control group, Reference Elkins, Steinberg, Razook, Ward, Overholt and Thompson24,Reference Rubay, Raphael and Sluysmans27 and six were excluded because they did not report separate outcomes for infants in the control group. The relative risk of truncal valve replacement in infants at the time of truncus arteriosus repair is 4.79 (95% CI: 1.75–13.13; p < 0.01) (Fig 4). There was significant, moderate heterogeneity between the included studies (I2 = 57%; Cochran’s Q test p = 0.0220). Additionally, the funnel plot (Supplemental Figure S4) and the Egger test (p = 0.58) did not demonstrate publication bias.

Figure 4. Forest plot of relative risk of early mortality in infants undergoing truncus arteriosus repair with concomitant truncal valve replacement compared to truncus arteriosus repair only (TVR, truncal valve replacement; TAR, truncus arteriosus repair; CI, confidence interval).
Late mortality
Nine of the 16 included studies were available for the evaluation of late mortality (Table 3). Among these patients, the linearised late mortality rate was 15.3%/year (95% CI: 5.8–40.7). Additionally, Kaplan–Meier analysis indicated a 1-year survival of 34.8% (95% CI: 22.5–54.0). Although the Egger test was insignificant (p = 0.20), the funnel plot of late mortality rates showed two outliers (Supplemental, Figure S5). These outliers were the studies by Elkins et al. Reference Elkins, Steinberg, Razook, Ward, Overholt and Thompson24 and Henaine et al., Reference Henaine, Azarnoush and Belli34 both of which had considerably short mean follow-up times compared with other included studies, which is the likeliest explanation for this finding. There was no significant heterogeneity between the included studies (I2 = 39.3%; Cochran’s Q test p = 0.11).
Reintervention
The same 9 of 16 studies used to evaluate late mortality rates were available to evaluate reintervention rates (Table 3). For these patients, the linearised reintervention rate was 21.7% (95% CI: 8.4–55.7). Kaplan–Meier analysis demonstrated a 1-year freedom from reoperation of 77.0% (95% CI: 59.9–99.1). Again, the Egger test (p = 0.30) was insignificant for publication bias. However, the funnel plot did demonstrate one outlier: the study by Henaine et al. Reference Henaine, Azarnoush and Belli34 Again, the likely explanation for this finding is the relatively short follow-up time of patients in this study. There was statistically significant, moderate heterogeneity (I2 = 57.2%; Cochran’s Q test p = 0.0156) between the included studies. This is also likely the result of the short follow-up time of the Henaine et al. Reference Henaine, Azarnoush and Belli34 study, leading to a comparatively inflated reintervention rate (Table 3).
Discussion
The purpose of this study was to systematically collect and analyse outcomes of infants (<12 months) undergoing concomitant truncal valve replacement during the primary repair of truncus arteriosus. This study found that truncal valve replacement during the primary repair of truncus arteriosus carries a considerably high early mortality and late mortality rate. Reintervention rates following this surgery are also substantial. The findings of this study underscore the dismal outcomes associated with unrepairable pre-operative truncal valve regurgitation warranting truncal valve replacement. Overall, the present analysis suggests that despite significant advances in the surgical treatment of truncus arteriosus over the past 60 years, truncus arteriosus repair with concomitant truncal valve replacement continues to be an unsolved problem in congenital heart surgery.
Early mortality
In the present analysis, patients undergoing truncal valve replacement during the initial repair of truncus arteriosus were found to have a significantly higher early mortality than those undergoing truncus arteriosus repair without truncal valve replacement. This discrepancy in outcomes is likely multifactorial, including increased perioperative acuity or prolonged aortic cross clamp and cardiopulmonary bypass times. Reference Naimo and Konstantinov4,Reference Bakar, Costello and Sassalos5 Moreover, valve implants do not grow, therefore mandating serial re-operations to replace the implants with larger implants as the children grow. Truncal valve insufficiency has also been known to be a risk factor for early mortality following the initial repair of truncus arteriosus. Ebert and colleagues reported that a majority of patients experiencing early mortality after truncus arteriosus repair at their institution had significant pre-operative truncal valve insufficiency, leading the authors to recommend truncal valve replacement in cases associated with severe pre-operative truncal valve insufficiency. Reference Ebert, Turley, Stanger, Hoffman, Heymann and Rudolph12 Despite this, not every patient undergoing truncal valve replacement in this analysis had severe insufficiency. In the earliest study in this series, Elkins and colleagues Reference Elkins, Steinberg, Razook, Ward, Overholt and Thompson24 asserted that the truncal valve should be replaced during primary repair for any clinically significant pre-operative stenosis or insufficiency. Other studies reporting truncal valve replacement in the absence of severe insufficiency did not provide a rationale for performing the replacement. It can only be speculated that these centres used a similar decision-making process to that of Elkins and colleagues, which is supported by the fact that all reported patients had either a degree of truncal valve insufficiency, stenosis, or a combination of both.
Few of the included studies detailed the cause of death for individual patients experiencing early mortality. Elkins and colleagues Reference Elkins, Steinberg, Razook, Ward, Overholt and Thompson24 reported an early death in a neonate with moderate truncal valve insufficiency and diabetic hypertrophic cardiomyopathy that was unable to wean from bypass and died shortly after repair. Another neonate with severe truncal valve insufficiency reported by Bove and colleagues Reference Bove, Lupinetti and Pridjian10 also died within hours of repair, likely as a result of coronary artery occlusion. Similarly, Rubay and colleagues Reference Rubay, Raphael and Sluysmans27 reported an early death from sudden haemodynamic decompensation in a non-neonatal infant with mild truncal valve insufficiency and an interrupted aortic arch. Rubay et al., Reference Rubay, Raphael and Sluysmans27 Jahangiri et al., Reference Jahangiri, Zurakowski, Mayer, del Nido and Jonas29 and Danton et al. Reference Danton, Barron and Stumper32 reported patients experiencing early mortality from right ventricular failure, congestive heart failure, and left ventricular failure, respectively. Lastly, Henaine and colleagues Reference Henaine, Azarnoush and Belli34 reported two early deaths of patients that both died from low cardiac output syndrome.
Late mortality and reintervention
Late mortality and reintervention rates of patients in the present analysis were substantial. As noted by many authors of the included studies, these rates are likely associated with the valve replacement itself. Reference McElhinney, Reddy, Rajasinghe, Mora, Silverman and Hanley7,Reference Elkins, Steinberg, Razook, Ward, Overholt and Thompson24,Reference Mavroudis and Backer31 Prosthetic valves pose some risk associated with anticoagulant usage and prosthetic valve endocarditis. Reference Jahangiri, Zurakowski, Mayer, del Nido and Jonas29,Reference Etnel, Elmont and Ertekin37 More importantly, in this young patient population, replacement valves fail as the patients outgrows their valves, requiring reintervention in the form of valve exchange. Reference Jahangiri, Zurakowski, Mayer, del Nido and Jonas29,Reference Mavroudis and Backer31 Several valve exchanges can be expected over the course of the patient’s life, and each exchange is associated with a risk of mortality.
The causes of late death were varied. Elkins et al. Reference Elkins, Steinberg, Razook, Ward, Overholt and Thompson24 reported one late death 2 months after the operation resulting from Staphylococcus aureus bacteremia. McElhinney et al. Reference McElhinney, Reddy, Rajasinghe, Mora, Silverman and Hanley7 reported one patient with a mechanical valve replacement died 8 months after operation due to the valve being lodged open, resulting in free insufficiency. Henaine et al. Reference Henaine, Azarnoush and Belli34 reported that one patient died 7 months after the initial repair and was found to have valve thrombosis at autopsy.
Reinterventions were described in several studies. McElhinney et al. Reference McElhinney, Reddy, Rajasinghe, Mora, Silverman and Hanley7 reported that two neonates each initially received a homograft and subsequently underwent replacement of the homograft with a mechanical valve due to severe insufficiency. These replacements occurred 6 months post-operatively in one patient and 13 months post-operatively in the other. Mavroudis et al. Reference Mavroudis and Backer31 similarly reported a neonate initially receiving a homograft replacement, who received two subsequent homograft replacements at 4 months and 4.5 years post-operatively. Henaine et al. Reference Henaine, Azarnoush and Belli34 reported one neonate initially receiving a homograft replacement subsequently required replacement 3 months post-operatively due to valve failure. The same patient developed endocarditis and received a Bentall procedure 6 weeks after this reintervention.
The choice of valve used was largely divided between truncal valve replacement using a mechanical valve or truncal root replacement using a cryopreserved homograft with coronary reimplantation. In the present analysis, homografts comprised the majority of truncal valve replacements. Homografts are advantageous in that they are non-thrombogenic and thus do not require anticoagulation. Reference Stelzer and Elkins11 Additionally, homografts offer favourable haemodynamic profiles in the immediate post-operative period. Reference Stelzer and Elkins11,Reference Elkins, Steinberg, Razook, Ward, Overholt and Thompson24,Reference Mavroudis and Backer31 However, homografts have low durability in young patients, and reintervention is often required to address progressive valvular insufficiency. Reference O'Brien, Harrocks and Stafford38,Reference Clarke, Campbell, Hayward and Bishop39 Mechanical valves were the second-most common valve type used in this analysis. In general, mechanical valves offer improved durability over homografts with lower rates of reintervention. Reference Etnel, Elmont and Ertekin37 However, mechanical valves are thrombogenic and require life-long anticoagulation. Only one patient in the present analysis received a bioprosthetic valve. Bioprosthetic valves are not typically used in current practice because they carry high rates of early failure. Reference Etnel, Elmont and Ertekin37 As suggested by the high reintervention rates reported in this analysis, regardless of the valve type used, patients will inevitably require reintervention later in life as they outgrow the replacement. Reference Elkins, Steinberg, Razook, Ward, Overholt and Thompson24,Reference Jahangiri, Zurakowski, Mayer, del Nido and Jonas29,Reference Mavroudis and Backer31
Several alternatives to truncal valve replacement have been used to address truncus arteriosus with an unrepairable truncal valve. In response to poor outcomes seen with replacement, Henaine and colleagues recommend attempting truncal valve repair first and only resort to truncal valve replacement if the patient is unable to be weaned from cardiopulmonary bypass. Reference Henaine, Azarnoush and Belli34 Certain types of truncal valve repair may potentially be a viable alternative for replacement. While many variations of leaflet-sparing truncal valve repair exist, the leaflets of severely insufficient truncal valves are often dysplastic and thus provide an inadequate substrate to perform a durable repair. The Ozaki technique, in which the native leaflets are excised and replaced with leaflets constructed from glutaraldehyde-fixed autologous pericardium, could be considered in Truncus arteriosus repair with severe truncal insufficiency. Ishidou and colleagues Reference Ishidou, Ikai and Sakamoto40 reported performing the Ozaki technique during a truncus arteriosus repair for a patient with severe truncal insufficiency. The patient was alive and stable 1 year after the operation, and echocardiography showed moderate insufficiency and mild stenosis of the reconstructed valve. The authors acknowledge that this repair may offer limited durability due to leaflet sclerosis and somatic growth of the annulus but may be used as a bridge to valve replacement later in life. When faced with multiple complex cardiac defects, transplantation may be the most attractive option. For example, Akintuerk and colleagues Reference Akintuerk, Goerlach and Valeske41 reported transplanting the heart of a patient with a severe truncal valve insufficiency and an interrupted aortic arch. The patient survived the surgery and was discharged 4 weeks after undergoing transplantation. Due to the scarcity of donor organs, transplantation will not always be feasible. Reference Sherard, Atteya and Vogel42 Recently, surgeons have corrected truncus arteriosus with severe truncal valve insufficiency by performing a partial heart transplantation, Reference Rajab43,Reference Rajab, Ochoa and Zilinskas44 wherein the pulmonary and aortic roots of a donor heart otherwise unsuitable for orthotopic heart transplantation were used to perform the primary repair. The patient remained alive after over 6 months, and echocardiographic measurements show that the transplanted valves have grown with the patient. Reference Turek, Kang and Hoover45 The durability of this method of repair remains to be seen, but present results are optimistic. Ultimately, to circumvent the need for available donors, tissue engineering would be the ideal solution in providing a growing heart valve. Despite this, no tissue-engineered heart valve has yet succeeded in clinical translation. Reference Hasan, Ragaert and Swieszkowski46
Limitations
This study has several limitations inherent to its design as a systematic review and meta-analysis. Primarily, the analysis is limited by the reporting and quality of the included studies. The retrospective design of the included studies may have resulted in selection bias, particularly when reporting late mortality or truncal valve reintervention rates. The present analysis is also potentially subject to selection bias because non-published data were not considered. The rates of late mortality and reintervention cannot be reliably extrapolated outside the range of follow-up times of the included studies. Rates may be slightly overestimated as a result of using a continuity correction. This study was unable to account for concomitantly present abnormalities that may have influenced patient outcomes. Errors related to data collection may be possible, although two reviewers independently verified the extracted data to safeguard against this.
Conclusion
The repair of truncus arteriosus with concomitant truncal valve replacement in infants has poor early and late mortality, as well as substantially high rates of reintervention. As such, truncal valve replacement remains an unsolved problem in congenital cardiac surgery. Innovations in congenital cardiac surgery, such as partial heart transplantation or tissue engineering, are required to address this difficult subset of patients.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951123000604
Acknowledgements
The authors would like to acknowledge Hiroo Kinami for his role in the analysis.
Financial support
TKR is supported by grants from the American Association for Thoracic Surgery, the Brett Boyer Foundation, the Saving tiny Hearts Society, the Emerson Rose Heart Foundation, the South Carolina Clinical & Translational Research Institute 17 (NIH/NCATS Grant Number UL1 TR001450), NIH / NHLB 1 R4 1HL169059 and Philanthropy by Senator Paul Campbell.
Conflicts of interest
None.