1. Introduction
Major depression is one of the most prevalent and debilitating psychiatric disorders Reference Hamdi and Iacono[1] and ranks 5th worldwide among the leading causes of years lived with disability Reference Vos, Abajobir, Abate, Abbafati, Abbas and Abd-Allah[2]. It affects one in seven persons at some point during their life, with a lifetime morbidity risk of approximately 30% Reference Kessler, Pethukova, Sampson, Zaslavsky and Wittchen[3]. The disorder is multidimensional and involves cognitive (e.g., concentration difficulties), somatic (e.g., disrupted sleep), and emotional symptoms (e.g., feelings of guilt and/or worthlessness) and most individuals with a depressive disorder experience some difficulties in social, occupational and home functioning Reference Kessler[4, Reference McIntyre, Cha, Soczynska, Woldeyohannes, Gallaugher and Kudlow5].
Whereas memory dysfunctions are not among the core diagnostic features of depression, they are prevalent Reference Rock, Roiser, Riedel and Blackwell[6] and represent a multi-faceted and important battleground for the disorder. In addition to “cold” memory deficits for retrospective Reference Burt, Zembar and Niederehe[7, Reference Rock, Roiser, Riedel and Blackwell6] and prospective material Reference Zhou, Wang, Zheng, Zhang, Ungvari and Ng[8] that manifest already at the first episode Reference Lee, Hermens, Porter and Redoblado-Hodge[9], a number of memory distortions have been elucidated in depression that likely play a role in both the formation and maintenance of the disorder. For quite some time now, overgeneralized autobiographical memory (OGM) has been implicated as an important cognitive contributor to depression. OGM is associated with depression severity Reference Van Vreeswijk and De Wilde[10] as well as an increased risk for disease chronicity Reference Brittlebank, Scott, Williams and Ferrier[11–Reference Sumner, Griffith, Mineka, Rekart, Zinbarg and Craske15]. Another well-researched cognitive bias that has attracted attention since the 1980s Reference Blaney[16, Reference Bower17] is the mood-congruent memory (MCM) effect Reference Gaddy and Ingram[18], which refers to the phenomenon that depressed patients often show better recall and recognition for negative-valenced memory material Reference Matt, Vázquez and Campbell[19, Reference Moritz, Gläscher and Brassen20]. It has been argued that this bias is most prominent for negative information that is personally relevant Reference Gaddy and Ingram[18, Reference Matt, Vázquez and Campbell19, Reference Moritz, Voigt, Arzola and Otte21].
In addition, the phenomenon of false memories has been investigated in depression. False memories are defined as the recall of objects that were never presented, or events that never occurred Reference Roediger and McDermott[22]. Several studies have demonstrated that depression is not only characterized by enhanced loss of memory information, but also an increased susceptibility for false memories Reference Moritz, Gläscher and Brassen[20, Reference Moritz, Voigt, Arzola and Otte21, Reference Sejunaite, Lanza and Riepe24–Reference Wittekind, Terfehr, Otte, Jelinek, Hinkelmann and Moritz26]. Importantly, false memories, as retrospective memories, are often mood-congruent: Patients or individuals with a negatively-induced mood are more prone to falsely remember negative information Reference Moritz, Voigt, Arzola and Otte[21, Reference Howe and Malone23, Reference Wittekind, Terfehr, Otte, Jelinek, Hinkelmann and Moritz25–Reference Ruci, Tomes and Zelenski28]. More recently, it was found that MCM is modulated by context, as it makes a difference whether a positive word like “love” is presented with a positive or negative adjective (e.g., “no” or “much”) Reference Wittekind, Terfehr, Otte, Jelinek, Hinkelmann and Moritz[25, Reference Wittekind, Terfehr, Otte, Jelinek, Hinkelmann and Moritz26, Reference Bookbinder and Brainerd29].
The aforementioned memory distortions may lower mood in multiple ways. “Cold” (or content-neutral) cognitive dysfunction is related to psychosocial and functional outcome Reference Evans, Iverson, Yatham and Lam[30, Reference Jaeger, Berns, Uzelac and Davis-Conway31]) and cognitive dysfunction may be a primary mediator of functional deficits observed in depression Reference McIntyre, Cha, Soczynska, Woldeyohannes, Gallaugher and Kudlow[5, Reference Lam, Kennedy, McIntyre and Khullar32]. For example, low work performance is likely to lower mood via enhanced stress and other negative consequences (e.g., working over-time). However, some cognitive dysfunctions are secondary (see below) and subjective perception of decreased memory performance is more pronounced than objective problems Reference Moritz, Ferahli and Naber[33]. The former may foster unfounded worry about developing dementia or neurodegeneration, especially in middle-aged or older patients, which can foster depressive symptoms by catastrophizing Reference Kinzer and Suhr[34]. Memory preference for negative material may thus lead to a preponderance of negative information in an individuals’ consciousness and heavily distorts one's view of him- or herself and others, as well as the future [i.e., cognitive triad of depression; 35]. Accordingly, improving memory performance and “correcting” memory biases may also represent an important mechanism for mood repair. We thus concur with recent calls Reference Papakostas[35, Reference Trivedi and Greer36] to make cognitive problems a core target of depression treatment.
Psychotherapy, and particularly cognitive behavioral therapy (CBT), has shown to be effective in the treatment of depression, including relapse prevention Reference Cuijpers, van Straten, Schuurmans, van Oppen, Hollon and Andersson[37, Reference Steinert, Hofmann, Kruse and Leichsenring38]. CBT targets cognitive-affective biases, such as selective abstraction and over-generalization. In contrast, teaching patients about the aforementioned memory problems and biases is not part of standard CBT programs. Metacognitive Training for Depression (D-MCT) aims to fill this gap Reference Jelinek, Hauschildt and Moritz[39]. D-MCT amalgamates CBT exercises with a metacognitive approach that aims to modify depression-related “Beckian” emotional, as well as more general cognitive biases. D-MCT is a highly standardized open group intervention that contains eight modules. It is rooted in MCT for psychosis; for the similarities and differences between D-MCT and metacognitive therapy by Wells’ please see a recent commentary Reference Andreou, Jelinek, Balzan and Moritz[40]. One of D-MCT’s eight modules is devoted to memory. Patients are educated about memory problems in depression (and their origin), are introduced to the phenomenon of mood-congruent (false) memories and are taught how to improve their memories. It also addresses the frequent worry of patients that they may develop dementia. As discussed above, while memory impairment and other neuropsychological dysfunctions frequently occur in depression, the module uses a psychoeducational approach to inform patients that such memory difficulties may also be secondary to reduced motivation, or anxiety, as well as rumination or concentration difficulties during formal assessments Reference Moritz, Stöckert, Hauschildt, Lill, Jelinek and Beblo[41, Reference Scheurich, Fellgiebel, Schermuly, Bauer, Wölfges and Müller42]. Disclosure of these secondary influences is intended to attenuate patients’ exaggerated worries about a neurodegenerative process (normalization).
Results from a pilot study revealed positive effects of D-MCT on depressive symptoms Reference Jelinek, Otte, Arlt and Hauschildt[43]. Similar results were reported in a randomized controlled trial (RCT), in which D-MCT was found to be superior compared to an active control group with medium to strong effect sizes Reference Jelinek, Hauschildt, Wittekind, Schneider, Kriston and Moritz[44]. Additionally, patients rate the training positively at both immediate and long-term assessments Reference Jelinek, Moritz and Hauschildt[45].
This is the first study to investigate the influence of D-MCT on the proneness for false memories in depressed patients. We hypothesize that in comparison to a control intervention (i.e., Health Training), D-MCT would yield a greater effect in reducing patients’ susceptibility for false memories from baseline to post-assessment after 4 weeks.
2. Methods
2.1. Participants
This study is part of a larger trial Reference Jelinek, Hauschildt, Wittekind, Schneider, Kriston and Moritz[44], which reports results on the primary outcomes [i.e., measures of depression, dysfunctional attitudes, self-esteem and overall functioning] but not on false memories. A total of 84 patients who fulfilled DSM-IV diagnostic criteria for a depressive disorder and had no history of psychotic symptoms (i.e., hallucinations, delusions, or mania), current suicidality (Suicidal Behaviors Questionnaire Revised score ≥ 7), or intellectual disability (estimated IQ < 70). Patients were recruited from a psychosomatic outpatient day clinic (RehaCentrum Hamburg) at the University Medical Center Hamburg-Eppendorf (Germany). Patients were randomly allocated to either Metacognitive Training for Depression (D-MCT; n = 41) or Health Training (HT; n = 43). Written informed consent was obtained from all participants before participation in the baseline assessment. The study was approved by the Ethics Committee of the German Association for Psychology (DGPs) and was conducted in accordance with the Declaration of Helsinki. For the current study, participants with substance or alcohol dependence, as well as patients with a neurological disorder (including brain injury) were excluded. A total of 77 participants underwent the false memory paradigm at pre-assessment (92% from entire sample) and 68 at post-assessment [88% retention rate from subsample; D-MCT, n = 39 (pre), n = 33 (post); health training, n = 38 (pre), n = 35 (post)]. Table 1 shows group comparisons at baseline. Individuals in the two condition did not differ on any psychopathological or background characteristics, including type of medication, number of episodes and comorbid diagnoses. All participants provided written informed consent prior to participation. The study was registered at the German Clinical Trials Register (No. DRKS00007907).
Table 1 Sociodemographic and Psychopathological Characteristics of the Sample. Frequencies, Means and Standard Deviations (in Brackets).

Notes: BDI-I = Beck Depression Inventory-I, HDRS = Hamilton Depression Rating Scale, MWT-B = vocabulary test to estimate verbal intelligence.
2.2. Measures
2.2.1. Psychopathology
At baseline, each patient was interviewed with the Mini International Neuropsychiatric Interview (M.I.N.I) Reference Sheehan, Lecrubier, Sheehan, Amorim, Janavs and Weiller[46] to verify the presence of a single episode of major depression, recurrent depression, or dysthymia according to DSM-IV criteria. The 17-item version of the Hamilton Depression Rating Scale (HDRS) Reference Hamilton[47] was used to quantify depression at both assessment points. While the HDRS represents the gold standard for most clinical trials on depression, it has faced a number of criticisms Reference Bagby, Ryder, Schuller and Marshall[48, Reference Worboys49] so that depression was also captured with a self-rating instrument, the Beck Depression Inventory-I (BDI-I) Reference Beck and Steer[50, Reference Hautzinger, Bailer, Worall and Keller51].
2.2.2. False memory paradigm
The false memory effect was initially demonstrated for word lists Reference Deese[52, Reference Roediger and McDermott22], but subsequent research has replicated the phenomenon for visual Reference Miller and Gazzaniga[53] and other modalities Reference Röder and Rösler[54]. False memories were assessed with an established visual Deese-Roediger McDermott (DRM) paradigm Reference Jelinek, Hottenrott, Randjbar, Peters and Moritz[55–Reference Schilling, Wingenfeld, Spitzer, Nagel and Moritz58] for pre- and post-assessment; for details on the development of the task please refer to the respective literature Reference Jelinek, Hottenrott, Randjbar, Peters and Moritz[55–Reference Schilling, Wingenfeld, Spitzer, Nagel and Moritz58]. Each picture showed a complex scenario (i.e., “classroom”, “funeral”, “surveillance”, “beach”, “Christmas” “construction site”), in which eight details typical/central for the scenario were missing (e.g., in the beach scene, waves and a ball were not pictured). The missing, but strongly implied objects, represented “critical lures” for the recognition phase. A fixed choice of two scenarios were presented at each assessment in randomized order (i.e., “classroom” and “funeral”, “surveillance” and “beach”, “Christmas” and “construction site”). Which pair of scenes was shown at which assessment time was additionally randomized across participants. Each person was seated approximately 20 inches away from a 15-inch computer monitor and was instructed to carefully attend to the picture on the screen. Each of the two pictures was presented individually for 40 s and filled the entire screen. After the encoding phase, participants were asked to complete a vocabulary test to estimate verbal intelligence as a filler task Reference Lehrl[59], which lasted approximately 10 min. During the recognition phase, participants were presented studied, “old” items (e.g., people with sunglasses in the beach scene) and two types of non-studied items, presented as single words on the screen. Non-studied were either unrelated “new” items (e.g., “television” for the beach scene) or critical lures (e.g., “beach towel” for the beach scene). The specific order of items was randomized; a contextual cue was provided on the screen (i.e., “classroom”, “beach”, “funeral”, “surveillance”, “Christmas”, “construction site”) to clarify to which scene an item referred to. For each scenario, 24 items were presented: 12 “old” items (previously presented in the picture), 4 unrelated “new” items (not present in the picture and unrelated to the scene), and 8 “critical lures” (items not presented in the picture, but strongly related to the scene). Participants had to rate whether an item was old or new along with memory confidence on a four-point scale: 1 = old, confident, 2 = old, not confident, 3 = new, confident, 4 = new, not confident.
2.3. Design
Patients were randomly allocated to either D-MCT or HT following a fixed randomization plan. Groups met twice a week and the post-assessment occurred 4 weeks after baseline. The D-MCT intervention strictly followed the D-MCT manual Reference Jelinek, Hauschildt and Moritz[39]. The HT intervention was also performed twice weekly in a group format. Each week, patients participated in a psychoeducational group session, which provided information about general health topics (e.g., physical activity, nutrition, sleep) and included a session with physical activity (i.e., walking). At post-assessment, participants again completed all measures administered at baseline (except for the M.I.N.I.), including the visual DRM paradigm. The chosen scenarios for the DRM task were randomized over assessments (pre, post) to reduce practice effects.
2.4. Statistical analyses
Baseline differences between treatment groups regarding socio-demographic and psychopathological symptoms were examined by t-tests for independent samples. BDI data at baseline was missing for one patient. Patients with missing data on the DRM were excluded. To investigate changes in false memory performance over time, two different analyses were performed. First, a 3 × 2 × 2 ANOVA was carried out with the within-subject factors DRM Item Type (“old”, “new”, “critical lures”) and Time (pre, post), and the between-subject factor Group (D-MCT, HT) using the “old” ratings (percentage). Second, to investigate the influence of confidence, a 3 × 2 × 2 × 2 ANOVA with the within-subject factors Item Type (“old”, “new”, “critical lures”), Response (old, new), and Time (pre, post) as well as the between-subject factor Group (D-MCT, HT) was calculated using high-confident ratings only (please note that the measurement of old-confident and new-confident responses is non-redundant). An alpha level of 0.05 (two-tailed) was used for all statistical tests. Effect sizes Reference Cohen[60] were estimated with ηpartial2; ηpartial2 = 0.01 designates a small effect, ηpartial2 = 0.06 designates a medium effect and ηpartial2 = 0.14 designates a large effect.
3. Results
3.1. Participants
Participants in the two conditions did not differ on major demographic background variables or psychopathological symptoms (see Table 1). For results on the primary outcomes and remission rates, the reader is referred to the original article Reference Jelinek, Hauschildt, Wittekind, Schneider, Kriston and Moritz[44]. In short, improvement in depressive symptoms (BDI, HDRS) across time were larger in the D-MCT than in the HT group. More patients in the D-MCT group than in the control group remitted according to HDRS criteria (total score ≤ 8), which bordered significance for post-assessment (p = 0.064). Psychological well-being (subscale of the WHO QoL BREF) improved to a greater extent in the D-MCT than in the active control condition at post assessment. Emotional (“Beckian”) biases, as measured with the Dysfunctional Attitudes Scale (DAS), improved at trend level from pre to post (intention to treat analyses).
3.2. False memories and memory accuracy
The mixed 3 × 2 × 2 ANOVA (dependent variable: rating) revealed significant main effects of Item Type, F(2,66) = 628.63, p <.001, ηpartial2 = 0.905, and Time, F(2,66) = 977.54, p =.019, ηpartial2 = 0.081, which was qualified by an interaction of Item Type × Time, F(2,66) = 3.42, p =.036, ηpartial2 =.049. As shown in Fig. 1, most studied items were correctly rated as “old” and most new unrelated items were correctly rated as “new”. In contrast and speaking for the validity of the false memory paradigm, critical lures were often misattributed as “old”. The significant two-way interaction emerged because the rate of false memories (critical lures) was attenuated over time as confirmed by a paired t-test, t(67) = 3.57, p =.001. The three-way interaction (Item Type × Group × Time) revealed a linear trend, F(2,66) = 3.32, p =.073, ηpartial2 = 0.048, owing to somewhat less errors made by the D-MCT group across time.

Fig. 1. Ratings classified as “old” in the visual DRM paradigm for studied (“old”) items, unrelated new items, as well as “critical lures” across time depicted separately for the experimental (i.e., “Metacognitive Training for Depression” [D-MCT]) and the control intervention (i.e., “Health Training” [HT]). Critical lure items were frequently misclassified as “old” but this tendency decreased significantly over time (* paired t-test: p <.001).
3.3. False memories and confidence ratings
The mixed four-way ANOVA (dependent variable: high-confident judgments) revealed significant main effects for Item Type, F(2,66) = 80.10, p <.001, ηpartial2 = 0.548, and Response (old/new), F(1,66) = 34.72, p <.001, ηpartial2 = 0.345, which were qualified by a significant two-way interaction of Item Type × Response, F(2,66) = 503.35, p <.001, ηpartial2 = 0.884, as well as the three-way interaction of Item Type × Response × Time, F(2,66) = 5.27, p =.006, ηpartial2 = 0.074. As in the first ANOVA, old and unrelated new items were mainly attributed correctly (old items: 72% old-confident, 6% new-confident; new-unrelated items: 5% old-confident, 49% new-confident responses), which was not the case for “critical lures” (old-confident: 30%, new-confident: 18%). The three-way interaction emerged because for critical lures the rate of high-confident errors (i.e., old) decreased (32% to 28%) while the rate of high-confident correct (i.e., new) increased from 15% to 22% over time. For the four-way interaction, which included the Group factor, a significant linear trend emerged, F(1,66) = 5.46, p =.022, ηpartial2 = 0.076, which we followed up using single comparisons.
For each item type (“old”, “new”, “critical lures”), separate 2 × 2 × 2 ANOVAs with the within-subject factors Response (old-confident, new-confident) and Time (pre, post), as well as the between-subject factor Group (D-MCT, HT) were calculated (see Fig. 1). The mixed 2 × 2 × 2 ANOVA for “critical lures” (Fig. 2A) revealed a significant interaction of Time × Response × Group, F(1,66) = 4.63, p =.04, ηpartial2 =.07. The amount of “old-confident” responses to “critical lures” decreased from pre (D-MCT: 34%; HT: 30%) to post assessment (D-MCT: 25%; HT: 29%) to a larger extent in the D-MCT group (the pairwise t-test was significant for D-MCT, t(32) = 2.20, p =.035, but not the active control group, t(34) = 0.69, p =.492). Likewise, the amount of “new-confident” responses increased from pre (D-MCT: 17%; HT: 12%) to post assessment (D-MCT: 28%; HT: 17%) to a greater extent in the D-MCT relative to the active control condition (this was significant for the D-MCT, t(32) = 4.04, p <.001, and at a lower magnitude also for the control group, t(34) = 2.11, p =.043). For “old” and unrelated “new” items none of the effects involving Group achieved significance.
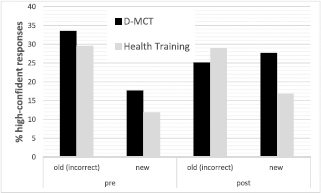
Fig. 2. Percentage of “high-confident responses” in the visual DRM paradigm for critical lure items (correct response: new) during pre and post assessment in depressive patients. In the D-MCT condition, the rate of high-confident false memories decreased more strongly over time relative to the active control condition (D-MCT vs. Health Training).
The decline in false memory (calculated separately for all high-confident false memories and responses made with high confidence) did not correlate with decline on the BDI or the HDRS (all rs < 0.22, all ps >.1). Also, none of the memory parameters were correlated with BDI or HDRS scores at baseline (|r| < 0.2; p >.1). Finally, we examined the possibility that false memories increased during treatment, which was seen for only a small subgroup of patients; 8.6% of the participants in the control group showed more false memories (irrespective of confidence) at post than at baseline (criterion: increase of more than one false memory over time) and only 6.1% of the experimental group. The difference was not significant, χ2(1) = 0.157, p =.692.
4. Discussion
For the first time, we explored whether Metacognitive Training for Depression (D-MCT) reduces the susceptibility of depressed patients for false memories. Memory dysfunction and more subtle distortions in memory, such as false memories, are implicated in the pathogenesis of depression and the amelioration of memory distortions may improve mood and other depressive symptoms (see Introduction). These aspects are therefore actively addressed in D-MCT and patients are given advice how to improve their memories.
In line with prior studies on the visual variant of the DRM paradigm Reference Jelinek, Hottenrott, Randjbar, Peters and Moritz[55–Reference Schilling, Wingenfeld, Spitzer, Nagel and Moritz58], false memories were induced for more than half of the stimuli at baseline. Over time, both tested interventions led to a decrease in false memories, which unlikely represents a practice effect as parallel versions were used. Regarding “critical lures”, the percentage of “old” ratings decreased more strongly (trend level) in the D-MCT group from pre- to post-assessment (61% vs. 50%) compared to the HT group (61% vs. 56%) providing initial evidence that patients in the D-MCT group are less prone to false memories after treatment.
We also specifically measured high-confident judgments, as judgments that are not held in check by doubt may lead to momentous false decisions that are particularly “toxic” Reference Moritz and Van Quaquebeke[61, Reference Moritz and Woodward62]. For high-confident judgments, the amount of false memories was significantly reduced over the course of treatment in the D-MCT group compared to the HT group, suggesting that a central goal of D-MCT has been met, that is, to attenuates usceptibility to false memories in depression. For both intervention groups (D-MCT and HT), no significant change in confident ratings occurred for “old” items and unrelated “new” items.
Interestingly, both groups showed an increased tendency towards “new-confident” ratings for “critical lures” at post-assessment and again this effect was more pronounced in the D-MCT group compared to the HT group. This finding may indicate that D-MCT does not lead to an overall increase of doubt, but rather a better calibration of confidence. Further studies are necessary to replicate this important finding.
While false memories have often been studied in Postraumatic Stress Disorder Reference Bremner, Snobe and Kihlstrom[63–Reference Hauschildt, Peters, Jelinek and Moritz65], less attention has been given to false memories in other psychiatric diseases, including depression. Importantly, the consequences of false memories on the course of depression and the changeability of the susceptibility to false memories, for example through therapy, have not been studied so far. In our study, we confirm the high rate of false memories in depression and, for the first time, describe the amelioration of false memories using a metacognitive training approach that was designed to evoke doubt.
To date, we may only speculate on the consequences of reducing false memories in depression, but it may be postulated that the amelioration of an important cognitive distortion may contribute to overall mood stabilization in patients with depression. This would be in line with one of the purported mechanisms of change in cognitive therapy for depression, such that the reduction of “Beckian” cognitive distortions leads to symptom improvement Reference Beck, Rush, Shaw and Emery[66, Reference Cristea, Huibers, David, Hollon, Andersson and Cuijpers67]. Interestingly, decline in false memories was uncorrelated with symptom change tentatively suggesting that D-MCT improves cognitive biases and mood independently.
The current study has some limitations that we would like to acknowledge. First, we only looked at short-term changes and thus cannot determine how stable the reported changes regarding false memories were. The lack of association between improved false memories and mood awaits to be tested more rigorously. Cognitive biases are assumed to foster psychopathology and a “sleeper effect” has been supported by previous work such that this association was found only using longer (e.g., 3 years) follow-up periods Reference Moritz, Veckenstedt, Andreou, Bohn, Hottenrott and Leighton[68]. Second, due to randomization we could not explore whether the effect was moderated by valence, that is, if the reduction is stronger for salient and negative-valenced material. Future studies should explore mood-congruent (negative) memories. Verbal false memory lists using lure words with validated emotional content are perhaps best suited to explore this. Third, although we assume that the effect observed was particularly due to the MCT module on memory, all D-MCT modules address thinking and cognitive biases and, therefore, the mechanism of action remains unclear. An overarching aim of D-MCT is to enhance reflection, and thus lower overconfidence in distorted self-appraisal (e.g. “I am ugly”), as well cognitive judgments (e.g., “I had a bad childhood, no one loved me). As such, this could have fostered the reduction of confidence in false memories. It would also be of interest to examine, for example, whether reduced confidence for false memories transfers to autobiographical information. We have already started to look at the module-specific effects of MCT for psychosis by collecting cognitive and psychopathological data from participants before and after each session Reference Schneider, Cludius, Lutz, Moritz and Rubel[69].
To conclude, the current study revealed a positive “add-on” effect of D-MCT for patients who also received an intense standard treatment in a psychosomatic hospital. Apart from the previously reported positive effects of D-MCT on depressive symptoms and psychological well-being Reference Jelinek, Hauschildt, Wittekind, Schneider, Kriston and Moritz[44], D-MCT seems to have a beneficial effect on memory biases, suggesting that D-MCT is a promising approach to correcting cognitive biases typical for depressed patients, including over-confident false judgments. Future studies should investigate whether D-MCT ameliorates other cognitive biases (e.g., OGM, MCM) as well and explore their putatively moderating role on psychopathology.
Public significance statement
Many patients with depression display false memories. Metacognitive training for depression (D-MCT) may help to reduce the susceptibility for false memories in depression.
Acknowledgements
We would like to thank Dr. Ruth Veckenstedt, Francesca Bohn, Natalia Steiner, Martina Fieker, Irmgard Musyal, Mirja Schwarz, Mario Broccucci, and Dr. Gabriela Kuhn for their help with recruitment of participants. The study was funded by a grant from the “Verein zur Förderung der Rehabilitationsforschung in Hamburg, Mecklenburg-Vorpommern und Schleswig-Holstein (vffr) [Society to promote research on rehabilitation in Hamburg, Mecklenburg-West Pomerania, and Schleswig-Holstein]” (www.reha-vffr.de); grant #161. The vffr had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript, or the decision to submit the manuscript for publication.






Comments
No Comments have been published for this article.