Introduction
Stroke is one of the leading causes of death and disability, with a prevalence of 700,000 cases annually in the USA. Reference Mukherjee and Patil1 It is associated with physical and neuropsychological complications, including depression. Reference Williams2 Consequently, there has been a focus on the mental health of stroke survivors, with a specific emphasis on depression, which correlates to a higher risk of mortality. Reference Bourgeois, Hilty, Chang, Wineinger and Servis3 Depression is common and serious neuropsychiatric sequelae among stroke survivors, and it is associated with longer hospital stays, decreased quality of life, poor cognitive function, and reduced engagement in the rehabilitation process, resulting in limited functional improvement and poor survival outcomes. Reference Rogers4,Reference Sugawara, Metoki and Hagii5
Obesity, generally defined as a body mass index (BMI) > 30 kg/m2, is a major public health problem, affecting more than 70 million adults in the USA, and it is a known risk factor for stroke. Reference Stevens, Singh and Lu6 Studies have also indicated that a higher BMI is associated with a chronic course of depressive symptoms. Reference De Wit, Van Straten, Van Herten, Penninx and Cuijpers7–Reference Luppino, de Wit and Bouvy9 Obesity is associated with a number of structural and functional alterations in the central nervous system that are highly comparable to those seen in depression, such as increased cell density in certain regions and impaired neuronal connectivity and excitability. Reference Rapuano, Laurent and Hagler10 Known risk factors for obesity, such as low physical activity and unhealthy eating habits, can result in chronic inflammation, which has an important role in the development of stroke and depression. Reference Dantzer11–Reference Mitchell, Cole and McArdle13
It is currently unknown if obesity modifies the association between stroke and depressive symptoms. Understanding the impact of obesity can help focus lifestyle modifications to help reduce the risk of depressive symptoms after stroke. Therefore, we conducted a cross-sectional study to evaluate the impact of BMI on the association between stroke and depressive symptoms, with the hypothesis that having a higher BMI, that is, being obese, will lead to a higher risk of depressive symptoms in those with a history of stroke compared to those without.
Methods
Study population
This study was conducted using data from the 2015–2016 Canadian Community Health Survey (CCHS) public-use microdata file. The CCHS is a repeated cross-sectional survey of the Canadian household population aged 12 years and older. Populations excluded from the survey include individuals living on reserves, institutionalized residents, and full-time members of the Canadian Armed Forces. The CCHS is delivered by Statistics Canada and contains core content, to which all regions respond, as well as optional content, which some regions respond to. For further information about CCHS, refer to the study by Beland et al. Reference Béland14 The depression module was optional in the CCHS, which restricted the study population to participating regions including Newfoundland and Labrador, Prince Edward Island, Nova Scotia, Quebec, Manitoba, North West Territories, and Nunavut. We excluded those without self-reported information on height and weight, and thus, no information on BMI, and those with missing information on history of stroke. We adhered to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational cohort studies.
Exposures
History of stroke was obtained based on the question, “Do you suffer from the effects of a stroke?” from the chronic conditions questionnaire. Responses were dichotomized as “yes” or “no.” This question has been shown to have moderate agreement (κ = 0.58) with physician claims data indicating presence of stroke. Reference Lix, Yogendran, Shaw, Burchill, Metge and Bond15 Self-reported height and weight were used to derive BMI (kg/m2). When calculating BMI, an adjustment equation was applied to minimize biases of overestimated height and underestimated weight. 16 BMI was categorized as underweight (≼18.5), normal weight (18.5– < 25 kg/m2), overweight (25– < 30 kg/m2), and obese (≥ 30 kg/m2).
Outcome measure
Depressive symptoms were measured by the 9-item Patient Health Questionnaire (PHQ-9) from the depression module of the CCHS. The PHQ-9 is a self-report measure used to assess major depressive disorder from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition diagnostic criteria by scoring the frequency of depressive symptoms over the past 2 weeks, with each answer ranging from 0 (“not at all”) to 3 (“nearly everyday”). Reference Choo, Spitzer and Williams17 The primary outcome of this study was the presence or absence of depressive symptoms, which was defined as a score of ≥ 10 on the PHQ-9. The secondary outcome was depressive symptoms severity, where the total PHQ-9 score was measured on a continuous scale ranging from 0 to 27. Severity of depressive symptoms is categorized as follows: minimal (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), and severe (20–27). The PHQ-9 is a validated tool for assessing depression symptomatology with a high sensitivity and specificity. Reference Levis, Benedetti and Thombs18 Furthermore, it has demonstrated good reliability, validity, and clinical utility when used in stroke patients who are able to communicate adequately. Reference de Man-van Ginkel, Gooskens, Schepers, Schuurmans, Lindeman and Hafsteinsdóttir19
Covariates of interest
Age, sex, race, anxiety/mood disorders, total household income, marital status, and alcohol use in the last 12 months were selected as covariates based on prior work. Reference Kutlubaev and Hackett20–Reference Goodwin and Devanand23 Age was categorized as 20–29, 30–39, 40–49, 50–59, 60–69, 70–79, or 80+ years. Sex was dichotomized as male or female. Race was categorized as “White,” “Non-White (visible minority),” or “Aboriginal - First Nations, Mètis, Inuk.” Anxiety/mood disorders were dichotomized as having at least one existing anxiety or mood disorder, or none at all. Total household income was categorized into “No income or less than $20,000,” “$20,000–$39,999,” “$40,000–$59,999,” “$60,000–$79,999,” or “$80,000 or more.” Marital status was categorized into “married or common-in-law,” “divorced, separated, widowed,” or “single.” Alcohol use in the last 12 months was categorized into “less than weekly,” “weekly,” or “daily.”
Statistical analyses
All analyses were conducted using R v 4.2.2. We used t-tests to assess differences in continuous variables and chi-squared tests to assess differences in categorical variables. Multivariable logistic regression models were used to examine the association between stroke and depression. Multivariable linear regression models assessed the association between stroke and depression severity. Partially adjusted models include only age and sex as covariates, while the fully adjusted models include all the aforementioned covariates of interest. The effect-modifying role of BMI was assessed through interaction terms (BMI category*stroke), as well as stratified analyses by underweight, normal, overweight, and obese categories. In addition, BMI was modeled as a linear variable using cubic spline terms with 3 knots to assess the potential nonlinear effects of BMI on the associations between stroke and depression. To account for multiple testing in a subgroup analysis by BMI category, a significance level of P <0.01 was used. Statistical significance was set at a level of P <0.05 in all other analyses. All models were run based on a complete case analysis. Survey weights were not used in the primary analysis due to the limited regions that completed the depression module. Analyses were subsequently repeated with survey weights, and the corresponding results are provided in the Supplementary (Tables S1-S3).
Results
Demographic characteristics
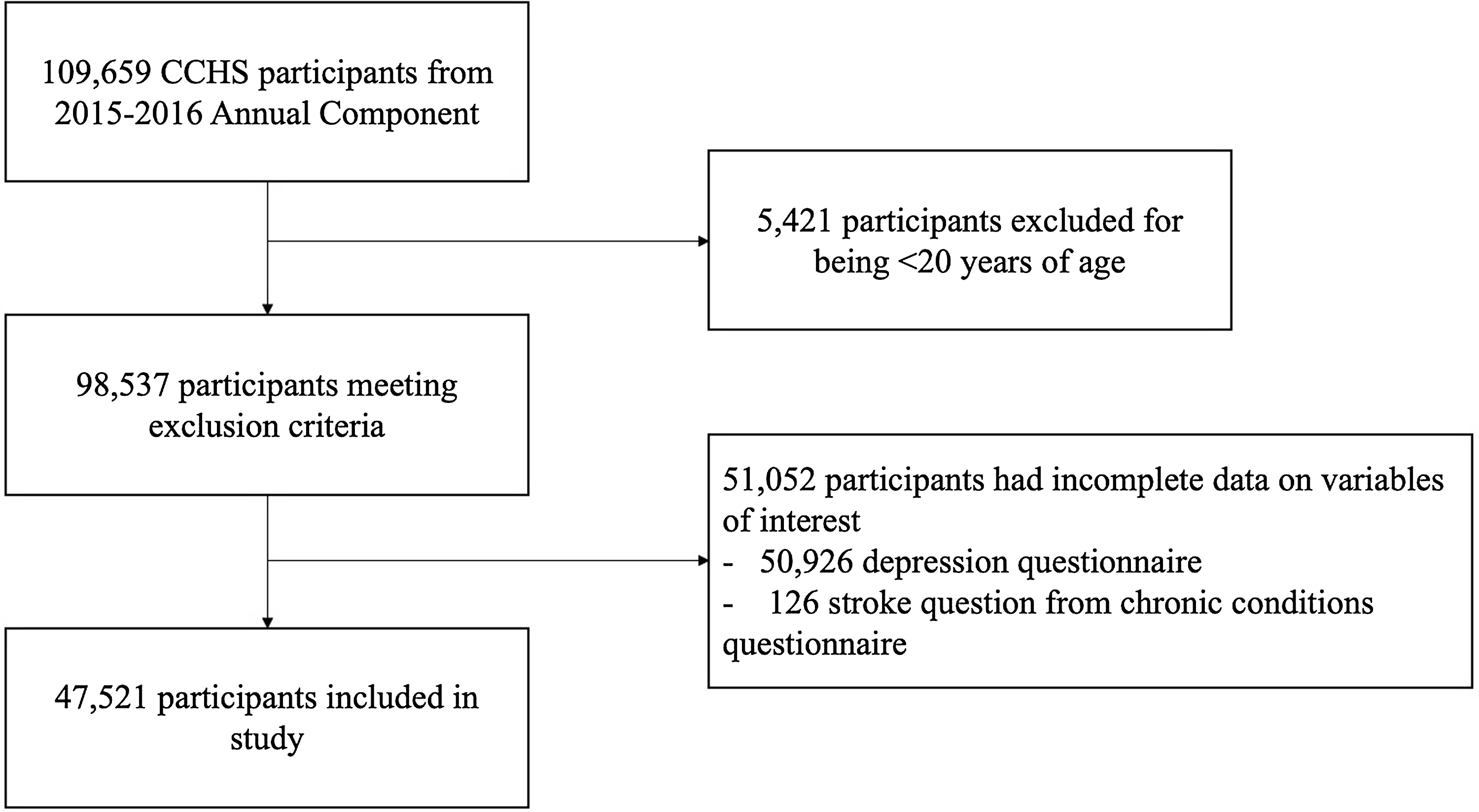
Data were collected from a total of 109,659 individuals from the 2015–2016 CCHS cycle. After excluding participants that were less than 20 years old or had missing data for the stroke question or depression questionnaire, the study population consisted of 47,521 individuals (Fig. 1). Of the included people, 694 (1.0%) reported the effects of a previous stroke, and 3314 (6.5%) reported depressive symptoms. Additionally, 16,174 (36.4%) participants were overweight, and 15,015 (29.4%) were obese. Between those with and without depression, mean BMI was 29.15 (SD = 6.87) and 27.69 (SD = 5.45), respectively. Table 1 displays the unweighted demographic characteristics of the study population and further outlines any differences between the two groups. Table S1 includes the weighted demographic characteristics.

Figure 1. Participant inclusion flowchart, 2015–2016 Canadian Community Health Survey (CCHS).
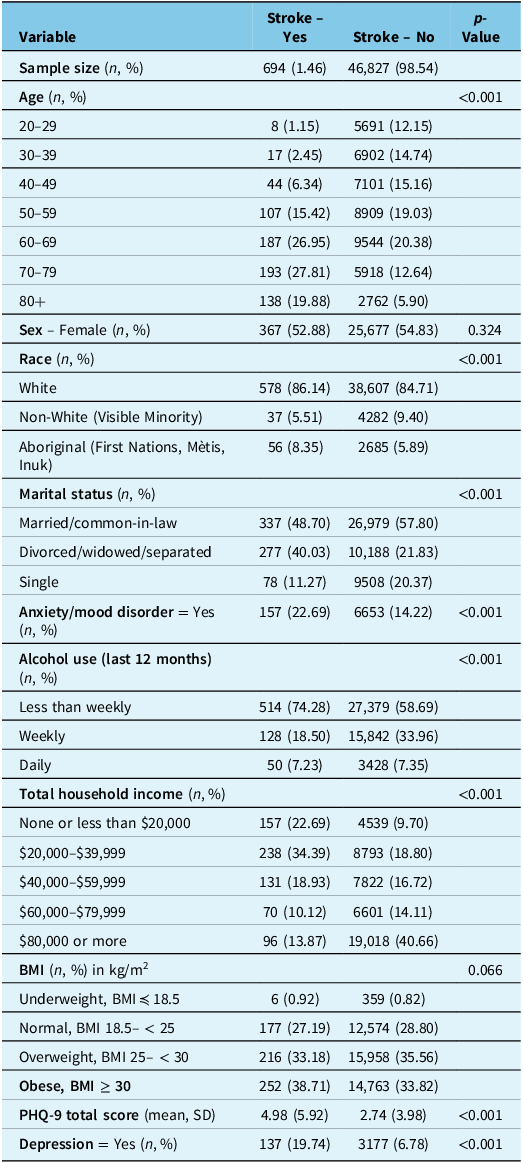
Table 1. Demographic characteristics of the study population from 2015 to 2016 CCHS (n = 47,521)

CCHS = Canadian Community Health Survey; BMI = body mass index; PHQ-9 = 9-item Patient Health Questionnaire. Categorical characteristics reported as unweighted frequency and %; continuous characteristics are reported as unweighted mean and standard deviation.
Depression as a binary variable
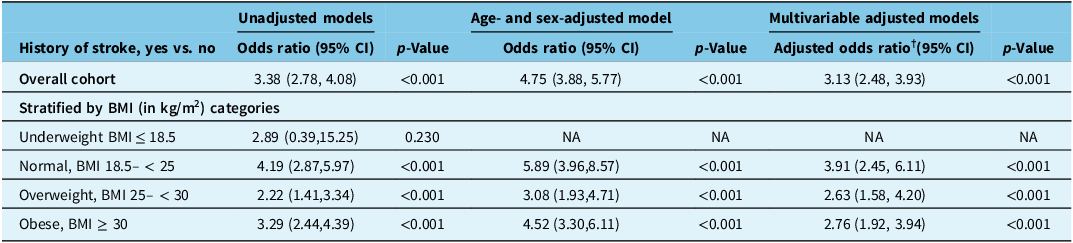
Having experienced the effects of previous stroke was associated with higher adjusted odds of reported depressive symptoms compared to those who have not experienced the effects of stroke (fully adjusted odds ratio [aOR†] = 3.13, 95% confidence interval [CI] 2.48, 3.93, p < 0.001). The association between a previous stroke and reported depressive symptoms was not modified by BMI (PBMI*stroke = 0.242). When modeled as a continuous variable using restricted cubic splines, the odds of reported depressive symptoms among individuals with a previous stroke compared to those without stroke varied depending on BMI, with higher odds ratio of reported depressive symptoms in individuals with a previous stroke compared to the general population in those with normal BMI while a lower odds ratios in those who were overweight or obese (Fig. 2). In stratified analyses, having a previous stroke was associated with higher odds of reported depressive symptoms in all categories of BMI except underweight, where the model did not converge due to small sample size: normal weight (aOR† = 3.91, 95% CI 2.45, 6.11), overweight (aOR† = 2.63, 95% CI 1.58, 4.20), and obese (aOR† = 2.76, 95% CI 1.92, 3.94) (Table 2). Adding survey weights did not change our findings (Table S2).

Figure 2. The association between stroke and depressive symptoms based on multivariable logistic regression model for varying values of body mass index (BMI), modeled as cubic spline term. Restricted cubic splines curve of multivariable logistic regression analysis according to the BMI. The solid line indicates the adjusted odds ratio according to the BMI and the dotted lines are for 95% CI. CI = confidence interval.
Table 2. Association between history of stroke and presence of depressive symptoms (PHQ-9 score ≥ 9) stratified by body mass index (BMI) categories

CI = confidence interval; NA = not applicable; PHQ-9 = nine-item Patient Health Questionnaire.
†(Adjusted odds ratio – full) model controlled for age, sex, race, marital status, anxiety/mood disorder, total household income, and alcohol use in the last 12 months; significance is set to P < 0.01 for multiple testing. All Ps < 0.001.
Depression as a continuous variable, depression severity
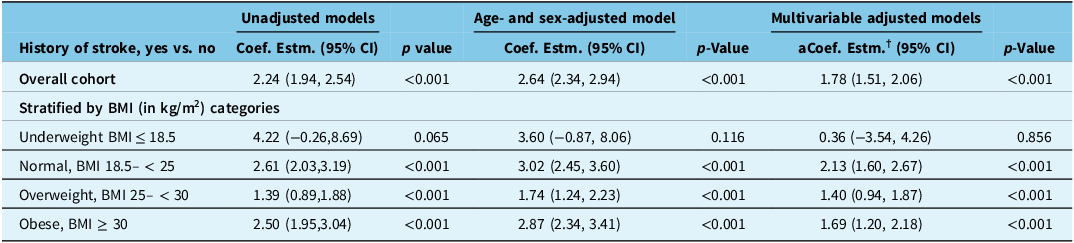
In the overall sample, after adjusting for all covariates of interest, having a previous stroke was associated with a 1.78 points higher mean PHQ-9 score compared to that in people without a history of stroke, suggesting a higher depressive symptoms severity in stroke survivors (fully adjusted coefficient estimate [aCoef. Estm.†] = 1.78, 95% CI 1.51, 2.06). There was no effect modification of the association between stroke and depressive symptoms by BMI, when categorized into the three categories (PBMI*stroke = 0.218). When modeled using restricted cubic spline terms, a U-shaped effect was again noted with higher depression severity in survivors compared to the general population at lower and higher values of BMI (Fig. 3). In stratified analyses, having a stroke compared to the general population was associated with a higher depressive symptoms severity in all categories of BMI except for those in the underweight category: underweight (aCoef. Estm.† = 0.36, 95% CI −3.54, 4.62), normal weight (aCoef. Estm.† = 2.13, 95% CI 1.60, 2.67), overweight (aCoef. Estm.† = 1.40, 95% CI 0.94, 1.87), and obese (aCoef. Estm.† = 1.69, 95% CI 1.20, 2.18) (Table 3). Table S3 shows the results using survey which indicated no significance in those in the underweight group as well as the overweight group.

Figure 3. The association between stroke and depressive symptoms severity based on multivariable linear regression model for varying values of body mass index (BMI), modeled as cubic spline term. Restricted cubic splines curve of multivariable logistic regression analysis according to the BMI. The solid line indicates the adjusted odds ratio according to the BMI and the dotted lines are for 95% CI. CI = confidence interval; PHQ-9 = nine-item Patient Health Questionnaire.
Table 3. Association between history of stroke and depressive symptoms severity (measured as PHQ-9 score) stratified by BMI categories

aCoef. Estm. = adjusted coefficient estimate; BMI = body mass index; CI = confidence interval; PHQ-9 = nine-item Patient Health Questionnaire.
†(adjusted coefficient estimate – full) model controlled for age, sex, race, marital status, anxiety/mood disorder, total household income, and alcohol use in the last 12 months; significance is set to P < 0.01 for multiple testing. All Ps < 0.001. The point estimates denote mean difference in PHQ-9 score between those with history of stroke vs. those without history of stroke.
Discussion
Using data from a nationwide representative survey of over 25,000 Canadians, we evaluated the effect of self-reported BMI on the relationship between stroke and depressive symptoms. We confirm that having a stroke is associated with higher odds of depressive symptoms and a higher depressive symptoms severity. While the odds ratio of depressive symptoms following stroke varied with different values of BMI, the interaction terms were not statistically significant when BMI was modeled either as a continuous or categorical variable.
We found a higher odds of depressive symptoms and greater depressive symptoms severity among stroke survivors compared to the general population, which is in keeping with prior studies. Reference Rajashekaran, Pai, Thunga and Unnikrishnan24–Reference Broomfield, Quinn, Abdul-Rahim, Walters and Evans26 The pathophysiology underlying this association is not fully known, and its complexity has been demonstrated by previous research, Reference Ji, Wu, Wang, Liu, Bi and Wang27,Reference Frank, Gruenbaum, Zlotnik, Semyonov, Frenkel and Boyko28 with stroke location and stroke type playing an important roles in the development of depression following stroke. Reference Rajashekaran, Pai, Thunga and Unnikrishnan24 Stroke survivors can develop depression shortly after or within the first few months of the cerebrovascular event. Reference Medeiros, Roy, Kontos and Beach29 In our study, the prevalence of depressive symptoms in stroke survivors was 17.3%. This contrasts with the results from Paolucci et al. (2008) who reported a 30% incidence of post-stroke depression. Reference Paolucci30 This difference in findings may be because the depressive symptoms questionnaire used in the CCHS only measures symptoms during the past 2 weeks. Because the depression status prior to stroke is not known for the included participants, we cannot know if the observed rate of depressive symptoms post-stroke is definitely as a result of the stroke.
Our study indicated that BMI does not modify the relationship between stroke and depressive symptoms. Although having a stroke was associated with depressive symptoms in each BMI subgroup, the global interaction was not statistically significant. To our knowledge, this is the first study that evaluated the effect modification of BMI in relation to stroke and depressive symptoms. Among studies of stroke survivors, Sarfo et al. (2017) and Lee et al. (2021) found no significant differences in the BMI of those who had depression and those who did not. Reference Sarfo, Jenkins and Singh31,Reference Lee, Jeon and Kim32 Taken together, this suggests that stroke-depressive symptoms are unlikely to vary by BMI.
The direction of change with the changes in BMI in the odds ratio of depression in those with stroke compared to those without was contrary to our hypothesis. High BMI is associated with several health complications, such as cardiovascular, musculoskeletal, neurological, and respiratory diseases, which can result in functional impairment and depression. Reference Kinlen, Cody and O’Shea33,Reference Cha, Akazawa and Kim34 As a result, individuals with a high BMI are more likely to have physical and functional limitations, an unhealthy lifestyle, and a lack of physical activity, regardless of whether they had a stroke. Reference Kurth, Gaziano and Rexrode35 In contrast, individuals with normal BMI might have generally better physical health. Reference Paolucci30 As such, physical limitations from stroke in individuals with a normal BMI may contribute to greater changes in lifestyle and physical functioning than in individuals who are obese or overweight BMI, possibly leading to greater depressive symptoms. Other explanations could be the type and severity of stroke which can vary by BMI and could influence the rates of depression. Reference Hirata, Ovbiagele, Markovic and Towfighi22,Reference Bertakis and Azari36–Reference Wang, Huang and Chen40 Unfortunately, our datasets did not have information on the stroke type, or the severity or the location of stroke.
Another explanation of our findings of the lack of effect modification of BMI on stroke–depressive symptoms association may be collider bias. The latter occurs when an exposure and an outcome each influence a common third variable and that variable or collider is controlled for in the analysis. Reference Holmberg and Andersen41 BMI is associated with both stroke and depression and when studied as an effect modifier, it may lead to a collider bias. In one study of stroke survivors, the 10-year survival after stroke was highest for obese participants and lowest for participants of a normal weight, indicating that obesity may equate to improved stroke survival, a finding attributed to collider bias by the authors. Reference Vemmos, Ntaios and Spengos42 In contrast, we included the general population as a comparison group, modeled BMI as both continuous and categorical variable, and measured depressive symptoms as a binary and continuous variable, suggesting the robustness of our findings. Yet, it is possible that in our sample obese or overweight stroke survivors were less likely to die compared to those who are normal weight. Therefore, when stratifying the entire cohort based on BMI categories, we could be measuring depressive symptoms in a proportion of selected obese stroke survivors who may also be less likely to have adverse outcomes, including depressive symptoms. Thus, our work suggests the need for dedicated prospective studies to evaluate the role of BMI on the development of depressive symptoms after stroke.
Limitations
CCHS is a cross-sectional study which limits our ability to derive causal relationships. Additionally, stroke-specific factors such as stroke type, stroke severity, acute therapies for stroke, and disability after stroke were not available in the CCHS dataset, which could all influence the odds of depressive symptoms following stroke. Reference Towfighi, Ovbiagele and El Husseini43 Self-report questionnaires were used to measure the exposure and outcome variables, which makes them susceptible to participant biases such as recall, social desirability, and nonresponse bias. Reference Sjöström and Holst44,Reference Hunger, Schwarzkopf, Heier, Peters and Holle45 Since BMI was determined primarily through self-reported data, measurement inaccuracy might have resulted in an erroneous relative risk estimate. Furthermore, the way the stroke question is framed in CCHS could influence our findings. This is because individuals who had a milder stroke, recovered fully, those who survived without disability, and those who had a transient ischemic attack might answer negatively to the question. Additionally, it’s important to note that the PHQ-9 identifies a 2-week period of reporting symptoms, which may not capture depressive symptoms occurring prior to that timeframe. We were not able to distinguish how many of the included participants had a history of anxiety or mood disorder, separately, especially the proportion of people with history of depression. Lastly, we did not have information on use of anti-depressants or anti-psychotics which could vary in those with a history of stroke and those without a history of stroke, and across different BMI categories. Our findings are only generalizable to community-dwelling stroke survivors who may be less likely to have severe stroke, which is a known risk factor for depression. Our data regarding obesity might also not be generalizable to all Canadians since studies have previously reported an obesity prevalence of 26.8% while our results showed a prevalence of 35.4%. 46
In conclusion, the association between stroke and depressive symptoms varies by different values of BMI, but there was no statistically significant interaction between BMI and stroke. The observed lower odds ratio of depression in those with stroke compared to those without among people with higher values of BMI vs. those with lower values of BMI warrants further investigation to understand the observed phenomenon. Future work with detailed phenotypic information on stroke characteristics and the timing of depression following stroke is required to understand the observed findings to help direct interventions that can help reduce the burden of depression associated with stroke.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cjn.2024.41.
Acknowledgements
None.
Author contributions
SM, MV, and VB conceptualized the study. The investigation was led by SM who was also responsible for writing the original draft. VKT and MW were responsible for the methodology, data curation, formal analysis, and visualization. WL and HJ supervised formal analysis. Study conceptualization and manuscript writing were supervised by VB and MV. All authors provided critical revisions to the manuscript for intellectual content and contributed to editing. All authors read and approved the final manuscript.
Funding statement
VB is supported by an Academic Scholar Award from the University of Toronto Department of Psychiatry and has received research support from the Canadian Institutes of Health Research, Brain & Behavior Foundation, Ontario Ministry of Health Innovation Funds, Royal College of Physicians and Surgeons of Canada, Department of National Defence (Government of Canada), New Frontiers in Research Fund, Associated Medical Services Inc. Healthcare, American Foundation for Suicide Prevention, Roche Canada, Novartis, and Eisai. MVV is supported by Heart and Stroke Foundation of Canada.
Competing interests
None.