Book contents
- Temperament Based Therapy with Support for Anorexia Nervosa
- Temperament Based Therapy with Support for Anorexia Nervosa
- Copyright page
- Dedication
- Contents
- Figures
- Tables
- Contributors
- Foreword
- Preface
- Acknowledgments
- Introduction
- Section 1 Temperament Based Therapy with Support (TBT-S) Overview
- Section 2 Setting Up Treatment
- Section 3 TBT-S Treatment Interventions
- Section 4 TBT-S Augmenting Eating Disorder Treatments
- Book part
- Glossary
- References
- Index
- References
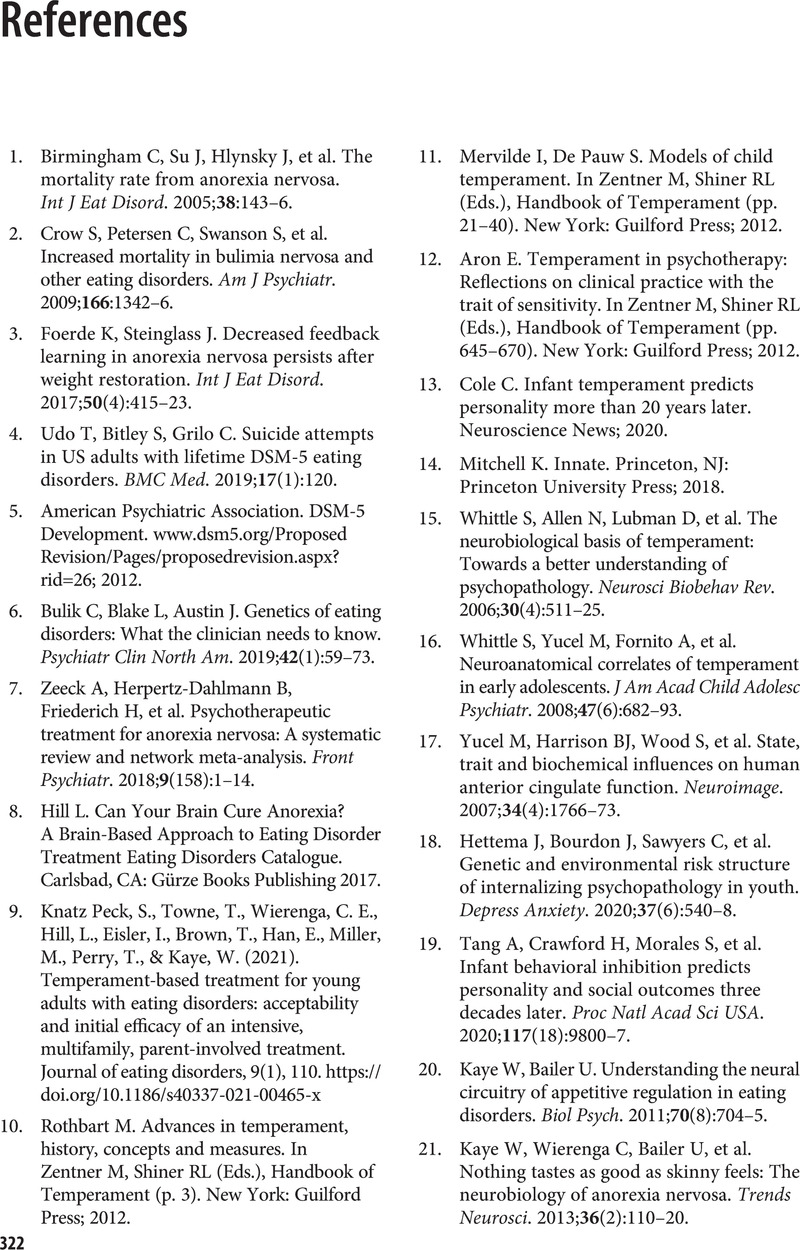
References
Published online by Cambridge University Press: 31 March 2022
- Temperament Based Therapy with Support for Anorexia Nervosa
- Temperament Based Therapy with Support for Anorexia Nervosa
- Copyright page
- Dedication
- Contents
- Figures
- Tables
- Contributors
- Foreword
- Preface
- Acknowledgments
- Introduction
- Section 1 Temperament Based Therapy with Support (TBT-S) Overview
- Section 2 Setting Up Treatment
- Section 3 TBT-S Treatment Interventions
- Section 4 TBT-S Augmenting Eating Disorder Treatments
- Book part
- Glossary
- References
- Index
- References
Summary
- Type
- Chapter
- Information
- Temperament Based Therapy with Support for Anorexia NervosaA Novel Treatment, pp. 322 - 330Publisher: Cambridge University PressPrint publication year: 2022