Book contents
- Comprehensive Men’s Mental Health
- Comprehensive Men’s Mental Health
- Copyright page
- Contents
- Contributors
- Preface
- Section 1 The Developmental Context and Developmental Disorders
- Section 2 Body Image and Anxiety Disorders
- Section 3 Suicidality and Mood Disorders in Men
- Section 4 Violence, Sociopathy, and Substance Misuse in Men
- Section 5 Physical and Mental Health Overlap
- Section 6 Mental Health of Men in Later Life
- Index
- References
Section 6 - Mental Health of Men in Later Life
Published online by Cambridge University Press: 10 March 2021
- Comprehensive Men’s Mental Health
- Comprehensive Men’s Mental Health
- Copyright page
- Contents
- Contributors
- Preface
- Section 1 The Developmental Context and Developmental Disorders
- Section 2 Body Image and Anxiety Disorders
- Section 3 Suicidality and Mood Disorders in Men
- Section 4 Violence, Sociopathy, and Substance Misuse in Men
- Section 5 Physical and Mental Health Overlap
- Section 6 Mental Health of Men in Later Life
- Index
- References
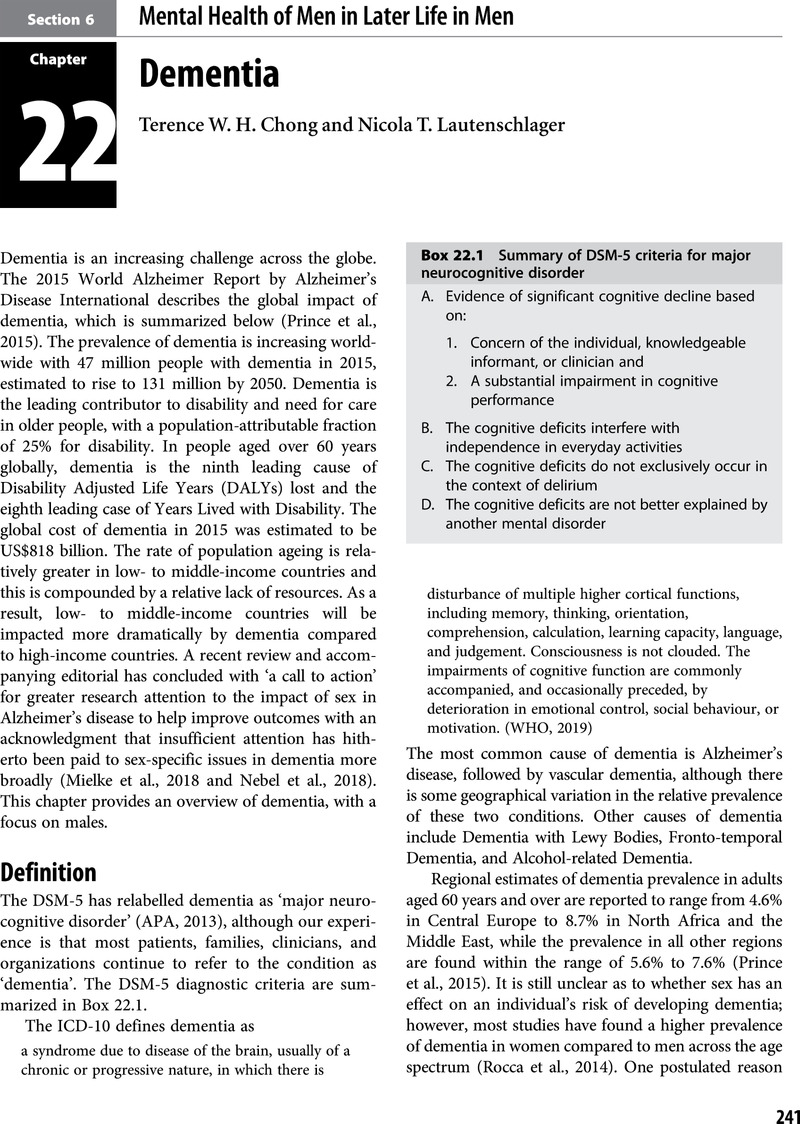
Summary
- Type
- Chapter
- Information
- Comprehensive Men's Mental Health , pp. 241 - 262Publisher: Cambridge University PressPrint publication year: 2021