Book contents
- The Management of Procedure-Induced Anxiety in Children
- Reviews
- The Management of Procedure-Induced Anxiety in Children
- Copyright page
- Contents
- Preface
- Acknowledgements
- Chapter 1 Introduction
- Chapter 2 Emergent Management of Procedure-Induced Anxiety (PIA)
- Chapter 3 Non-verbal Communication
- Chapter 4 Verbal Communication
- Chapter 5 Enhanced Communication Strategies
- Chapter 6 Premedication
- Chapter 7 Disordered Behaviour
- Chapter 8 Family
- Chapter 9 Additional Anxiogenic Influences
- Chapter 10 Elective Management
- References
- Index
- References
References
Published online by Cambridge University Press: 28 May 2021
- The Management of Procedure-Induced Anxiety in Children
- Reviews
- The Management of Procedure-Induced Anxiety in Children
- Copyright page
- Contents
- Preface
- Acknowledgements
- Chapter 1 Introduction
- Chapter 2 Emergent Management of Procedure-Induced Anxiety (PIA)
- Chapter 3 Non-verbal Communication
- Chapter 4 Verbal Communication
- Chapter 5 Enhanced Communication Strategies
- Chapter 6 Premedication
- Chapter 7 Disordered Behaviour
- Chapter 8 Family
- Chapter 9 Additional Anxiogenic Influences
- Chapter 10 Elective Management
- References
- Index
- References
Summary
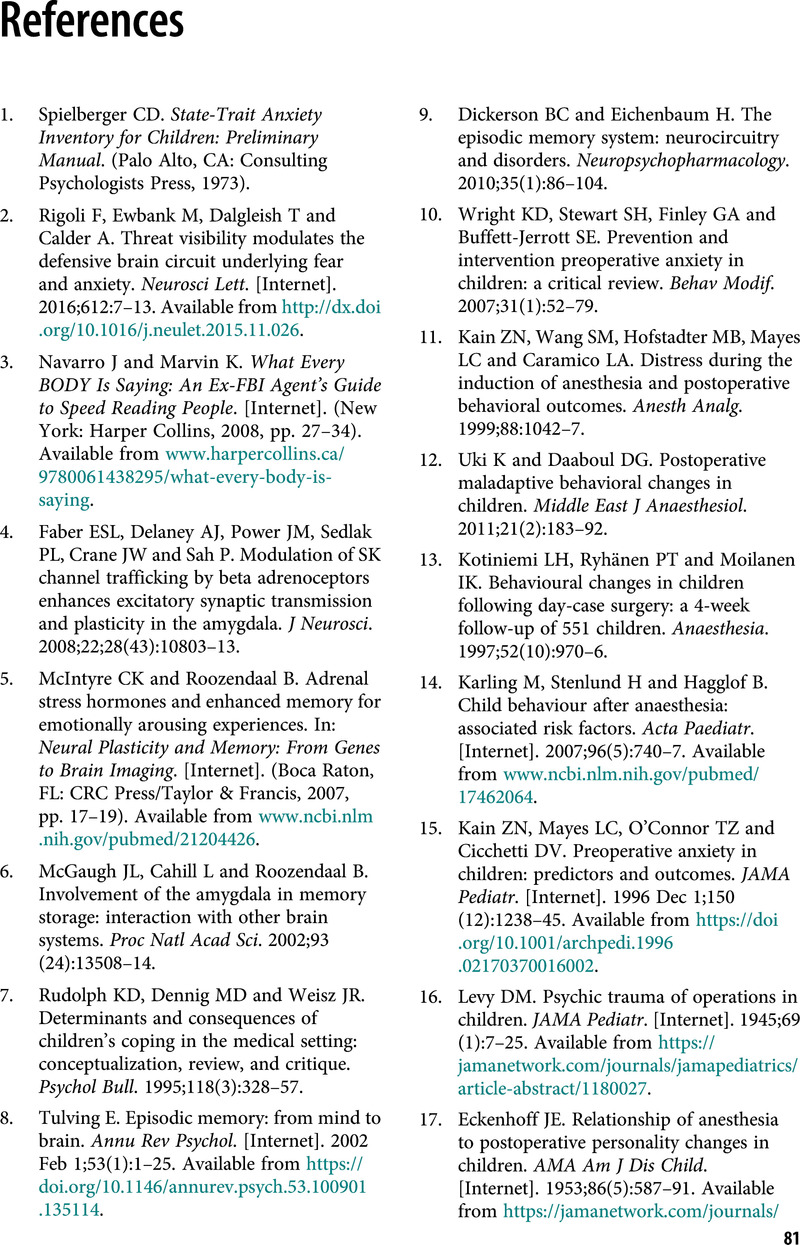
- Type
- Chapter
- Information
- The Management of Procedure-Induced Anxiety in Children , pp. 81 - 89Publisher: Cambridge University PressPrint publication year: 2021