In England, those living in the most affluent local area can expect to have good health for 17 years longer than those in the most deprived local area (The Marmot Review Team, 2010). A wide body of evidence has shown that health inequalities like this do not arise by chance. Health inequalities cannot be attributed simply to genetic make-up, ‘bad’, unhealthy behaviour, or difficulties in access to medical care, important as those factors may be. The conditions of people’s daily life shape their health behaviours and health outcomes, and an unequal distribution of money, power and resources in turn shape the conditions of daily life (The Marmot Review Team, 2010). Fair Society, Healthy Lives (The Marmot Review Team, 2010) set out the evidence regarding the drivers of health inequalities in England, and proposed six high-level policy objectives to inform action. These are called the ‘social determinants of health’ and include:
1. Give every child the best start in life.
2. Enable all children, young people and adults to maximise their capabilities and have control over their lives.
3. Create fair employment and good work for all.
4. Ensure a healthy standard of living for all.
5. Create and develop healthy and sustainable places and communities.
6. Strengthen the role and impact of ill health prevention.
Out of these recommendations, to essentially reduce inequalities in adult health, giving every child the best start in life is seen to be a priority policy, driven by two key facts – inequalities are evident at early ages, and inequalities accumulate. Therefore, reducing inequalities in the early years can have the greatest effect on life chances. In an ‘Equal Start’ we delve more into the drivers of inequalities in the early years specifically, and identify 21 outcomes to create lasting changes to children’s future life chances (Pordes-Bowers et al., Reference Pordes-Bowers, Strelitz, Allen and Donkin2012). These outcomes cluster into three key groups: improvements in children’s cognitive, social and emotional and physical development; improvements in parenting; and improvements in parents’ lives. The focus of this work was not purely on child health, although this would be an outcome, but also on other developmental outcomes, recognising that future health would be driven by such factors as their education, ability to control emotions and income, as much as their health in childhood: improving child health is necessary but not sufficient to ensure optimal health outcomes in later life.
This chapter takes a slightly different slant, and focuses solely on identifying the social determinants of child health and mortality, and not on the wider set of outcomes required to minimise inequalities in later life, although there will be some crossover. My approach is to identify the most common causes of mortality and poor health, and to look at the social determinants associated with these.
Birthweight
Let’s start at the beginning with infant mortality, which contributes the most to mortality rates in childhood. Deaths among babies who are born weighing less than 2,500 g (less than 5½ lbs) account for about three-quarters of neonatal deaths and two-thirds of infant deaths (Office for National Statistics, 2014). In addition, low birthweight continues to have an impact into childhood and later life, with increased risk of long-term disability and impaired development (Reichman, Reference Reichman2005). Infants born weighing less than 2,500 g are more likely than heavier infants to experience delayed motor and social development (Hediger et al., Reference Hediger, Overpeck, Ruan and Troendle2002). Lower birthweight also increases a child’s likelihood of having a school-age learning disability, being enrolled in special education classes, having a lower IQ and dropping out of high school (Reichman, Reference Reichman2005). The risk for many of these outcomes increases substantially as birthweight decreases, with very low birthweight babies (less than 1,500 g) being most at risk. There is also some evidence to suggest that there is a higher risk of obesity in later life for those born with a low birthweight (Rogers, Reference Rogers2003). Reducing the prevalence of low birthweight should therefore be a priority and action should help to reduce inequalities given that low birthweight babies are more common in mothers with lower socio-economic status (SES) (Dibben et al., Reference Dibben, Sigala and Macfarlane2006; Oakley et al., Reference Oakley, Maconochie, Doyle, Dattani and Moser2009).
The main risk factors for low and very low birthweight include multiple births (more than one foetus carried to term), maternal smoking, low maternal weight gain or low pre-pregnancy weight, maternal or foetal stress, infections and violence towards the pregnant woman (Ricketts et al., Reference Ricketts, Murray and Schwalberg2005). In addition, in the UK over 5 per cent of mothers of babies born in 2010 were under 20 years old and low birthweight rates are higher among teenage mothers, possibly because of competition for nutrients between the foetus and its mother who is also growing and developing (Baker et al., Reference Baker, Wheeler, Sanders, Thomas, Hutchinson, Clarke, Berry, Jones, Seed and Poston2009) or because teenage diets are poor (Bates et al., Reference Bates, Lennox, Prentice, Bates and Swan2012). Teenage pregnancies remain approximately twice as high for women living in the most deprived areas compared with the least deprived (Health and Social Care Information Centre, 2013).
Poor health behaviours have been associated with increased prevalence of low birthweight babies in less advantaged socio-economic groups. There are two main pathways by which living in low socio-economic circumstances can be associated with poor health behaviours. The first, relevant to diet for instance, is that incomes can be too low to afford a decent diet; the second, relevant to substance abuse, smoking and domestic violence, is that low incomes and unemployment or poor-quality work increase stress. Depression and stress can lead to negative maternal behaviours, domestic violence, poor prenatal care and substance abuse; antenatal maternal stress and poor maternal mental health have been found to impact on foetal development (Talge et al., Reference Talge, Neal and Glover2007) with maternal depression contributing to low birthweight (Gutman et al., Reference Gutman, Brown and Akerman2009; Jennings et al., Reference Jennings, Stagg and Connors1991). Given that 34 per cent of families with children are unable to afford a minimum acceptable standard of living (Padley et al., Reference Padley, Valadez and Hirsch2014), the effects of low income on nutritional adequacy, stress and poor health behaviours should not be underestimated, and efforts to address low birthweight may be ineffective without efforts to reduce poverty or mitigate its negative effects.
Cancer
After the first year of life, the most common causes of death are cancer, other non-communicable diseases and external causes including injuries. So far, the prevalence of most childhood cancers has not been linked to social determinants.
Some children inherit DNA changes from a parent that increase their risk of certain types of cancer, but most childhood cancers are the result of DNA changes that happen early in the child’s life, sometimes even before birth. Sometimes the causes of gene changes in certain adult cancers are known (such as cancer-causing chemicals in cigarette smoke), but the reasons for DNA changes that cause most childhood cancers are not known. A few environmental factors, such as radiation exposure, have been linked with some types of childhood cancers. Some studies have also suggested that some parental exposures (such as smoking) might increase a child’s risk of certain cancers, but more studies are needed to explore these possible links.
However, while there may be little evidence of social determinant causes of cancer, there is some evidence of socio-economic differences in survival. For example, a study of Norwegian children found that mortality was reduced by about 15 per cent for children with highly educated mothers and children without siblings. These effects were most pronounced for cancers predicted to encompass intense, long-lasting treatments resulting in chronic health problems. Neither earnings nor the marital status of parents affected children’s survival. The authors hypothesise that fewer time constraints and various non-economic rewards of parents from their education appear to have an impact on childhood cancer survival (Syse et al., Reference Syse, Lyngstad and Kravdal2011).
In terms of non-communicable diseases, I will focus on three issues: obesity, mental health and oral health.
Obesity
Analysis of data from the Health Survey for England for two–15-year-olds shows that obesity is approximately twice as likely in the poorest compared to the richest households, and by the Index of Multiple Deviation (IMD) that obesity prevalence was highest in the most deprived and lowest in the least deprived areas (Ryley, Reference Ryley2013). Similarly, analysis of National Child Measurement Programme data for four–five-year-olds showed obesity and overweight prevalence varied from 18 per cent in the least deprived areas to 25 per cent in the most deprived ones (Lifestyle Statistics Team, 2013), findings that are based on measurements of over 90 eligible children (Figure 3.1).
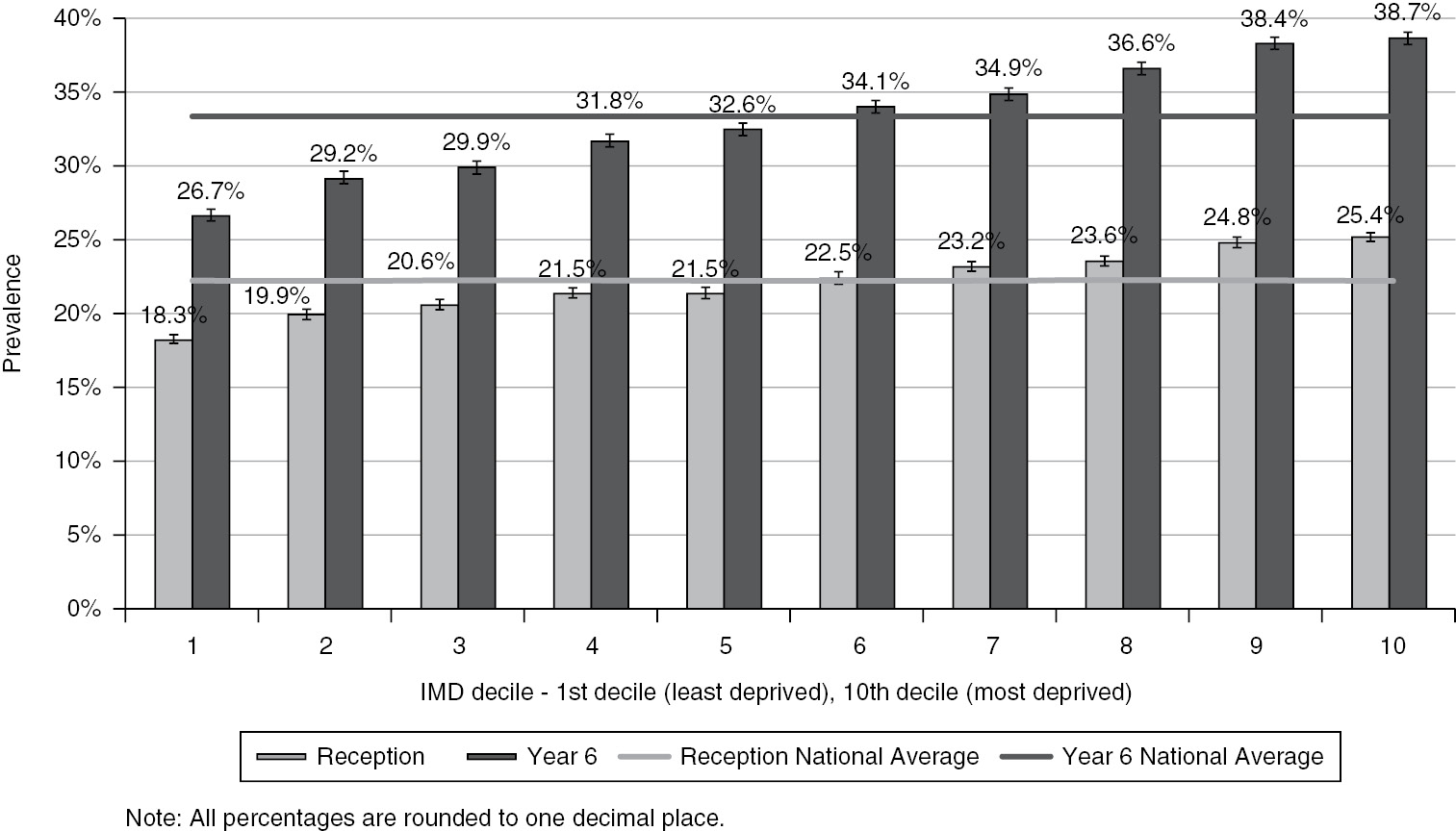
Figure 3.1 Obesity rates by deprivation decile at Reception and Year Six, 2012/13.
As previously stated in the low birthweight discussion, there is evidence to suggest that factors associated with low SES start to impact on the nutrition of the foetus in the womb. Socio-economic adversity or teenage pregnancy during the prenatal period is associated with an increased risk of having a low birthweight baby (Dibben et al., Reference Dibben, Sigala and Macfarlane2006; Oakley et al., Reference Oakley, Maconochie, Doyle, Dattani and Moser2009); however, low income women are also more likely to enter pregnancy being obese than their peers (Moody, Reference Moody2013) which, in turn, increases the risk of having a baby above the healthy weight range. Birthweight outside either end of the ideal birthweight range is associated with an increased risk of childhood obesity (Rogers, Reference Rogers2003).
Another contribution to inequalities in obesity could be inequalities in breastfeeding (which can also protect babies from infection and help prevent sudden infant death syndrome in early life). Breastfeeding is less common in more disadvantaged socio-economic groups (McAndrew et al., Reference McAndrew, Thompson, Fellows, Large, Speed and Renfrew2012). Breastfeeding, relative to formula feeding, is associated with a decreased risk of later obesity (Arenz et al., Reference Arenz, Ruckerl, Koletzko and Von Kries2004; Owen et al., Reference Owen, Martin, Whincup, Smith and Cook2005). Furthermore, maternal depression, which is more prevalent in low income households, can have a negative impact on the ability of mothers to breastfeed successfully (Gutman et al., Reference Gutman, Brown and Akerman2009; Jennings et al., Reference Jennings, Stagg and Connors1991).
While the factors above contribute to a propensity to obesity at a young age, the figures suggest that obesity levels rise dramatically during primary school years and, in particular, the social gradient becomes more marked, with overweight children more likely to become obese if they are in a more deprived area. As Figure 3.1 illustrates, 38.7 per cent of children in the most deprived areas are overweight or obese by Year 6. People living on low incomes tend to have worse diets (Roberts et al., Reference Roberts, Cavill, Hancock and Rutter2013), and there is some evidence to suggest that this gap is widening. For example, purchases of fruit and vegetables have declined since 2007, and that decline has been most marked in low income households (Defra, 2012). The rapid recent growth of food banks also suggests that the number of people facing food insecurity and nutritional vulnerability is growing, with 1,084,604 people – including 396,997 children – receiving three days’ food from the Trussell Trust’s network of foodbanks in 2014/15, compared with 913,138 in the 2013/14 financial year, an increase of 19 per cent (The Trussell Trust, 2014).
A key point here is that good food, foods that are nutrient-dense per calorie, are more expensive (Maillot et al., Reference Maillot, Ferguson, Drewnowski and Darmon2008). Therefore, people on low incomes will find it harder to buy the type of healthy diet for their children that we know we need to maintain a healthy weight – lean meat, fish and fruits and vegetables are relatively expensive forms of calories. The research has indeed shown that for any given level of energy intake, a lower consumption of fruits and vegetables was associated with lower diet cost (Drewnowski et al., Reference Drewnowski, Monsivais, Maillot and Darmon2007) and that at each level of energy intake, higher dietary energy density was associated with lower diet costs (Drewnowski et al., Reference Drewnowski, Darmon and Briend2004). In addition, in deprived areas there also tends to be a proliferation of fast-food outlets which serve large portions of unhealthy food which can lead to high levels of temptation.
Mental Health
Moving onto mental health, a key statistic is that children in the poorest households are three times more likely to have a mental illness than children in the best-off households (Department of Health, 1999). Even at an early age these differences are evident; for example, in one study at three years of age, 2 per cent of children from families in the highest income group had socio-emotional difficulties compared with 16 per cent of those from families in the lowest income group (Ermisch, Reference Ermisch2008). Also, as children get older there is evidence that the steepness of the gradient in social and emotional problems becomes greater (Power and Matthews, Reference Power and Matthews1997). The effects of poor social and emotional development can be long-lasting. In the EPPE study, for example, children whose parents reported child development problems before the age of three showed lower attainment in mathematics and English at age 11; children who had one behavioural problem had lower skills in self-regulation and fewer positive behaviours (Sylva et al., Reference Sylva, Melhuish, Sammons, Siraj-Blatchford and Taggart2010). There is also growing evidence that children from lower socio-economic backgrounds also have higher rates of mental ill-health and diagnosed mental illness (Bradley and Corwyn, Reference Bradley and Corwyn2002). Based on Melzer’s 2000 study of child mental health in Britain, Spencer argues that:
If all children had the same risk of mental disorder as the highest income groups, then there would be 40.6 per cent fewer mental disorders, 59.3 per cent fewer conduct disorders (anti-social behaviours), 53.7 per cent fewer hyperkinetic disorders (ADHD) and 34.4 per cent fewer emotional disorders. (Spencer, Reference Spencer2008)
Some of these impacts could again occur before birth. For example, foetal alcohol spectrum disorder (FASD) has been identified as a leading known cause of intellectual disability in the Western world (Abel and Sokol, Reference Abel and Sokol1986) and is linked to alcohol consumption in pregnancy. People with an FASD can have difficulty in the following areas: learning and remembering, understanding and following directions, shifting attention, controlling emotions and impulsivity, communicating and socialising, practising daily life skills, including feeding, bathing, counting money, telling time and minding personal safety. FASD-related brain damage makes it difficult to deal with routine life situations. It causes people to make bad decisions, repeat the same mistakes, trust the wrong people, and have difficulty understanding the consequences of their actions (National Institute on Alcohol Abuse and Alcoholism, n.d.). Psychosocial stress during pregnancy has also been linked to increased risk for attention deficit hyperactivity disorder, schizophrenia and social abnormalities (Mulder et al., Reference Mulder, Robles De Medina, Huizink, Van Den Bergh, Buitelaar and Visser2002).
Once children are born, the attachments that children form with their parents are important in influencing how they will relate to others (Music, Reference Music2010). Children who experience poor treatment at home (physical abuse, physical neglect, psychological unavailability or verbal abuse) are more likely to behave aggressively to peers in nursery school, even if the setting is nurturing and supportive, and this can persist into adolescence (Carlson et al., Reference Carlson, Sroufe and Egeland2004; Sroufe et al., Reference Sroufe, Egeland, Carlson and Collins2005).
The quality of family relationships can also explain some of the socio-economic gradient in social and emotional outcomes. Financial difficulty and worklessness is associated with higher levels of stress and poor mental health, including depression (Kiernan and Mensah, Reference Kiernan and Mensah2011) and increased social isolation (Gutman et al., Reference Gutman, Brown and Akerman2009), which can, in turn, lead to parents displaying more irrational and volatile behaviour, or being unable to focus on their child’s development and needs, both of which can impair the parent–child relationship. Consequently, the development of secure attachment in the child is disrupted as well as the mother’s ability to provide positive, responsive parenting and learning opportunities (Maggi et al., Reference Maggi, Irwin, Siddiqi and Hertzman2010).
Children born to mothers with poor mental health, and particularly those children exposed to prolonged or repeated maternal mental ill health, have been found to display delayed language development, greater levels of misconduct, negative social and emotional development, poor physical health and lower levels of attachment. Levels of poor mental health, stress and depression are higher in poorer socio-economic groups (see Pordes-Bowers et al., Reference Pordes-Bowers, Strelitz, Allen and Donkin2012).
Research has also shown that the presence of adverse childhood experiences (ACEs) can increase the chances of children and young people experiencing mental illness or a low level of mental well-being, including low self-esteem, depression and relationship difficulties. WHO Euro reports that post-traumatic stress disorder has been reported in as many as a quarter of abused children (World Health Organisation, 2013).
An analysis of the 1958 British birth cohort study estimated the impact of childhood adversities on psychopathology (anxiety/affective/mood symptoms and diagnoses) across the life course (Clark et al., Reference Clark, Caldwell, Power and Stansfeld2010). This is one of the few studies that focus on older children. Figure 3.2 summarises some of the results related to adversity in the home.
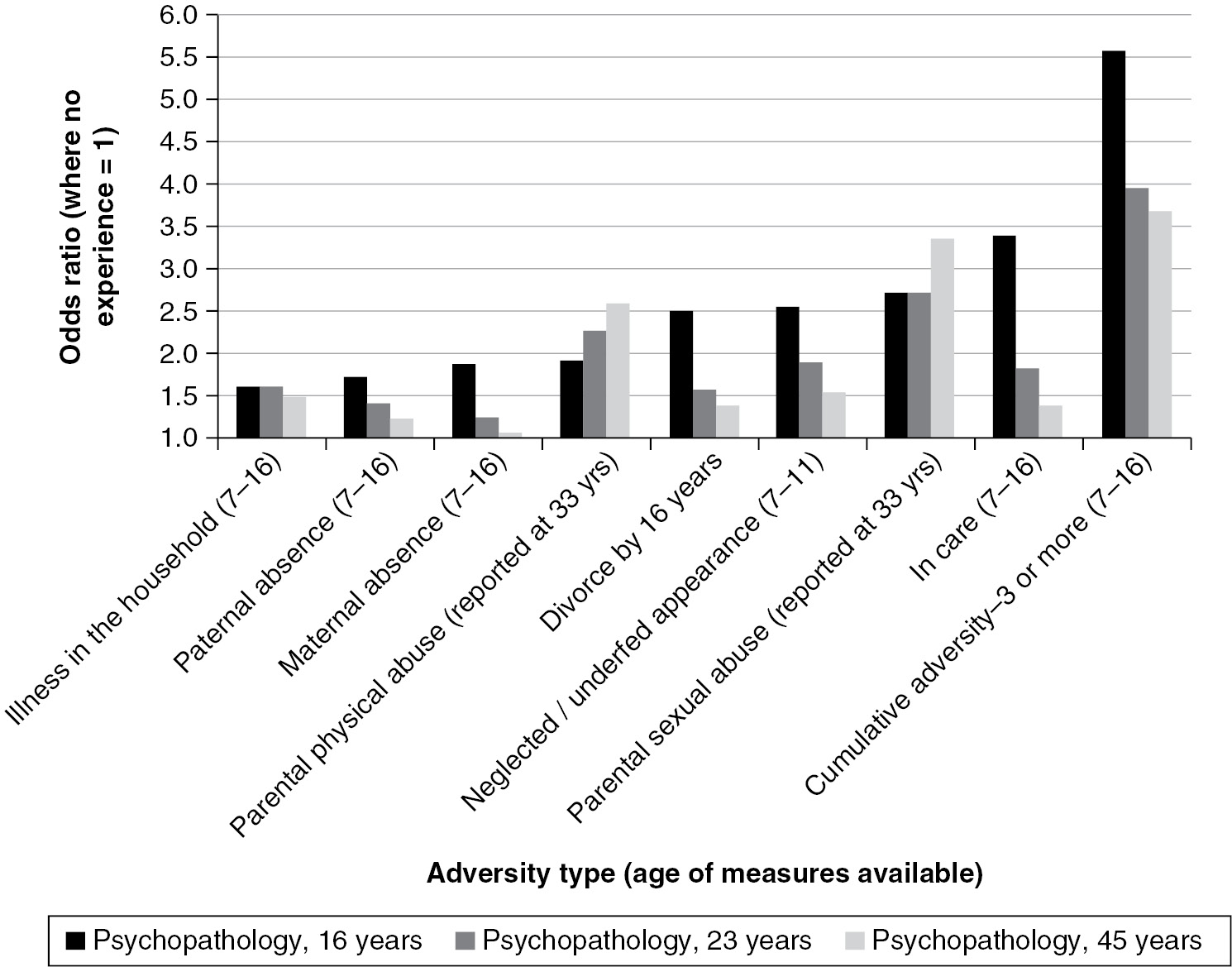
Figure 3.2 Varying impacts of different ACEs over time.
Figure 3.2 shows varying impacts of different ACEs over time. For example, some ACEs, such as divorce of parents, have a higher impact on mental illness at younger ages, which declines over time. Conversely, the impact of physical or sexual abuse seems to increase with advancing age. The Chief Medical Officer’s recent report on mental health has estimated that child abuse is responsible for between a quarter and a third of all adult mental illness (see Howard et al., Reference Howard, Shaw, Oram, Khalifeh and Flynn2014, p. 228).
It is possible that exposure to ACE during childhood and adolescence increases the likelihood of an individual adopting health-harming behaviours, including substance misuse, alcohol misuse, smoking, sexual risk behaviour, violence and criminality, or behaviours leading to obesity. An English study published in 2014 also found a correlation between number of ACEs and health-harming behaviours. The increased odds ratios associated with four or more ACEs varied from 2.0 for poor diet to 11.34 for incarceration. Heroin or crack cocaine use also showed a significantly increased odds ratio of 10.88 (Bellis et al., Reference Bellis, Hughes, Leckenby, Perkins and Lowey2014).
Adolescents and young people who grow up in disadvantageous conditions face higher risks of external injury, and are more likely to engage in excessive alcohol intake and other risk behaviours. More than half of deaths among adolescents are from external causes; the major modes are transport injuries, intentional and non-intentional injuries including suicide and violent deaths (Wolfe et al., Reference Wolfe, Macfarlane, Donkin, Marmot and Viber2014).
Oral Health
Finally, we do need to say something about inequalities in oral health. The 2003 Children’s Dental Health Survey (Office for National Statistics, 2003) found that children attending primary schools in socially deprived areas of the UK were reported to have experienced more tooth decay than children in schools in non-deprived areas. In deprived areas, 60 per cent of five-year-old and 70 per cent of eight-year-old pupils have obvious decay in their primary ‘milk’ teeth, compared with 40 per cent of five-year-olds and 55 per cent of eight-year-olds attending schools in non-deprived areas. Among both five- and eight-year-olds the probability of having decay into dentine or obvious decay experience of the primary teeth was about 50 per cent higher in the lowest social group than in the highest.
Policy Options
This chapter provides a broad view of some of the social determinants of poor child health and from this there are some key messages to improve child health, for example, increase breastfeeding, ensure good maternal and child nutrition, reduce smoking and drug and alcohol misuse and ensure children visit dentists regularly. However, all of these are socially graded and if the impact of poverty and education on the ability to buy healthy diets or give up bad behaviours is ignored, then health promotion messaging around these is likely to have limited impact. There are essentially two options for reducing the impact of inequalities – reducing inequalities or mitigating the impact.
Reducing Inequalities
Absolute child poverty is an increasing problem in the UK, with 35 per cent of households with children not having an income high enough to ensure an acceptable standard of living (Padley et al., Reference Padley, Valadez and Hirsch2014). Pressures on families are increasing throughout Europe, and are likely to be exacerbated by ongoing economic problems and reduced public service funding. There are frequent news stories about increasing strain on the National Health Service (NHS) and on Child and Adolescent Mental Health Services (CAMHS). Food poverty and hunger are growing problems in the UK, with over a million households using foodbanks (The Trussell Trust, 2014).
A key policy priority should be to ensure a minimum income for healthy living. In Fair Society, Healthy Lives we set out the importance of setting a minimum income for healthy living for addressing inequalities (The Marmot Review Team, 2010). The minimum income for healthy living includes the costs relating to purchasing those things that are needed to ensure adequate levels of nutrition, physical activity, housing, psychosocial interaction, clothing, transport, heating and hygiene (Morris et al., Reference Morris, Donkin, Wonderling, Wilkinson and Dowler2000). The University of York have developed a Minimum Income Standard which has a similar focus, but which also includes sufficient resources to participate in society and maintain human dignity, consuming those goods and services regarded as essential in modern-day Britain.
The level of income that a family has is a function of their wages, the available social protection and the costs of the goods and services that they buy. Any attempts to increase incomes should also consider these in the round. A significant challenge is that over half of British children in poverty now live in households where someone is working (MacInnes et al., Reference MacInnes, Aldridge, Bushe, Kenway and Tinson2013), and we therefore need to seek ways of improving the incomes of working-poor households. A living wage, based upon how much it costs to live a healthy life, should be available to those earning less than that amount as a first step; however, this is still very low and efforts should be made to ensure that all households across the income distribution earn enough through work. Many councils have adopted the living wage; in addition, ensuring that contracts are awarded to those adopting the living wage is another method of promoting this, as well as the use of local business advisors. For example, Islington Council was one of the first authorities to receive London Living Wage accreditation through Citizens UK, in March 2012. They pay all directly employed staff the living wage and agreed a schedule to ensure all council contracts will meet the living wage criteria by 2014 (Islington Council, 2012). The council is also working with a range of organisations in the borough, including schools, public sector providers and private businesses, to encourage and support them to pay the living wage (Islington Council, 2012).
Social protection (the benefit system) should support those who are unemployed and who do not earn enough to support a family. Ensuring that social protection is sufficient to support a family to live a healthy life is a role for central government. Supportive family policy can help protect children from the damaging effects of poverty and inequality. Countries that spend more on social protection for families have lower child mortality rates (World Health Organisation, 2014). Identifying where money is insufficient and intervening with discretionary grants is a role for local authorities. Local authorities should ensure that they have effective safety nets, and efforts could be made to curb rises in the prices of goods and services and housing at a local level. For example, many local authorities across the country, such as Coventry and Hammersmith and Fulham, chose to absorb the 10 per cent reduction in Council Tax Benefit that was made when the benefit was passed to councils to administer. This relieves some of the pressure on incomes of many households facing financial difficulties.
Mitigating Actions
Inequalities accumulate and so it makes much sense to reduce them as early as possible. Inequalities in the womb and in family life can lead to inequalities in children’s health and educational outcomes which then translate to health and economic inequalities later in life.
We need to get better at early identification and treatment of maternal depression, alcohol and drug misuse in pregnancy and we need to provide good quality support to improve parenting skills by communicating ‘what works’ to all parents, with interventions available to those who might be most at risk.
There are insufficient policies designed to improve social determinants of health, in part because while the public health sector understands the issues, the levers rest with other disciplines and government departments. Anxious to do something, public health officials revert to policies to modify health behaviours. However, these are often set to fail because people with social disadvantages may not have the self-esteem, personal agency, financial resources or positive mental health required to make lasting lifestyle changes. Improving negative health behaviours such as smoking and alcohol consumption requires a nuanced and evidenced approach to health policy. We need to tackle stress alongside asking people to change their behaviours, by, for instance, providing debt or housing advice and solving social problems. Then we need to make healthy choices the easy ones to make – for instance, by implementing policies such as financial subsidies on fruit and vegetables and taxes on less healthy foods, plain packaging of tobacco and minimum price per unit of alcohol (Wolfe et al., Reference Wolfe, Macfarlane, Donkin, Marmot and Viber2014). We need to ensure that decent housing is affordable, adequately insulated and free from damp. And all these policies to improve social determinants must be targeted proportionately across the social gradient to reduce health inequalities. We need to recognise that it is not just the difference between the richest and poorest but that there is a social gradient, and ignoring those in the middle, who have worse outcomes than the wealthiest, will miss much of the problem.
I will conclude with two points. The first is that approximately a quarter of all deaths under the age of one could potentially be avoided if all births had the same level of risk as those to women with the lowest level of deprivation (The Marmot Review Team, 2010). And the second is that while we have focused here on determinants of child health, we do believe that practitioners should not lose sight of the determinants of adult health that arise in childhood. For optimal adult health, we need to address not only child health, but also wider development outcomes, because these will impact on economic security in later life. The Equal Start framework developed by the Institute of Health Equity lists the wider set of outcomes that children’s services should be seeking to improve and maximise children’s life chances (Pordes-Bowers et al., Reference Pordes-Bowers, Strelitz, Allen and Donkin2012) and Measuring What Matters sets out how to measure these outcomes (Roberts and Donkin, Reference Roberts and Donkin2013; Roberts et al., Reference Roberts, Cavill, Hancock and Rutter2013).